Abstract
Purpose
The aim of this study was to evaluate the feasibility of short hospital stays after laparoscopic appendectomy for uncomplicated appendicitis.
Materials and Methods
The records of 142 patients who underwent laparoscopic appendectomy for uncomplicated appendicitis from January 2010 to December 2012 were analyzed retrospectively. Patients were allocated to an early (<48 hours) or a late (>48 hours) group by postoperative hospital stay. Postoperative complications and readmission rates in the two groups were evaluated and compared.
Results
Overall mean patient age was 50.1 (±16.0) years, and mean hospital stay was 3.8 (±2.8) days. Fifty-four patients (group E, 38.0%) were discharged within 48 hours of surgery, and 88 patients (group L, 62.0%) stayed more than 48 hours. Overall complication rates were similar in the two groups (14.8% vs. 21.6%, p=0.318), and wound complications (13.0% vs. 12.5%), postoperative bowel obstruction (1.9% vs. 2.3%), and abdominal pain (1.9% vs. 3.4%) were not significantly different.
Laparoscopic surgery for appendicitis is being widely performed worldwide, and is now regarded as the gold standard. Compared with open appendectomy, laparoscopic appendectomy has the advantages of less postoperative pain, better cosmesis, and shorter hospital stays. Furthermore, laparoscopic surgery probably reduces hospital costs by shortening hospital stay and providing early postoperative recovery. Recently, many efforts have been made to reduce hospital costs, and the topic of shortening hospital stay after appendectomy has attracted some interest, especially in the context of one-day surgery,1,2,3,4 because hospital stays after appendectomy usually exceed 3 days.5,6,7,8,9 The reports issued on this topic have cited hospital stays of from 2.2 to 6 days after uncomplicated appendectomy.6,7,8,9,10,11
With regard to reducing costs, non-operative management has been tried and reported to be both safe and feasible for uncomplicated appendicitis.12 However, surgical intervention remains the treatment standard.
The aim of this study was to evaluate the feasibility of short hospital stays after laparoscopic appendectomy for uncomplicated appendicitis.
The medical records of patients who underwent laparoscopic appendectomy for uncomplicated appendicitis from January 2010 to December 2012 at Severance Hospital were reviewed retrospectively. In total, 538 patients were diagnosed as having appendicitis and all underwent appendectomy during the study period. Laparoscopic appendectomy was performed in 362 patients and open appendectomy in 43. Uncomplicated appendicitis was defined as an acutely inflamed appendix with no evidence of perforation or generalized peritonitis by computed tomography or based on operative findings. All patients were admitted through an emergency room, and received surgical treatment and post-operative management based on physician's discretion. Only patients aged >18 years were included, and patients with a peri-appendiceal abscess or perforation or drain insertion were excluded (Fig. 1). After applying these criteria, 142 patients were enrolled and allocated to one of two groups according the duration of postoperative hospital stay; that is, to an early group (group E, <48 hours, n=54) or to a late group (group L, >48 hours, n=88). The discharge criteria used were as follows; 1) tympanic temperature <38.3℃, 2) a visual analogue scale (VAS) pain score of <4, 3) no aggravated physical signs, and 4) toleration of diet (>50%). However, these discharge criteria were not applied to all patients, because of primary physician's or patient's preference. Patient medical records were reviewed, and baseline characteristics, hospital stays, types and durations of antibiotics used, and postoperative complications, such as wound complications, intra-abdominal abscess development, urinary retention, pneumonia, postoperative bowel obstruction, abdominal pain, and readmission rate, were collated. Wound complications were defined as postoperative wound problems, including seroma and infection. Wound seroma and infection were not differentiated because of a lack of records. Postoperative bowel obstruction was the presence of gastrointestinal symptoms, such as nausea, vomiting, and abdominal pain with a VAS score of >5 on postoperative day 2 or more. Abdominal pain was defined as intolerable pain at time of discharge. Complication rates were analyzed according to the length of hospital stay, types of antibiotics used, and the relation between complication occurrence and duration of antibiotic use. Statistical analysis was performed using the chi-square test, the t-test, and the Mann-Whitney U test in SPSS ver. 20 (SPSS Inc., Chicago, IL, USA). Statistical significance was accepted for p-values <0.05. Continuous variables are presented as means (±standard deviations) or as medians and interquartile ranges.
This study was approved by the Severance Hospital Institutional Review Board (Institutional Review Board approval no. 4-2013-0785).
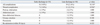
One hundred and forty two patients were included in this study. Mean study subject age was 50.1 years (±16.0) and there were 72 men (50.7%). Overall mean hospital stay was 3.8 days (±2.8), and overall time elapsed from entering the emergency room to surgery was 479.5 minutes (353.0-708.0). Fifty-four patients (38.0%) were discharged within 48 hours (the E group), and 88 stayed more than 48 hours (the L group). Patient baseline characteristics are summarized in Table 1. Times to diet and duration of antibiotic use after surgery were significantly different in the two groups (one vs. two days, and two vs. four days, respectively; p<0.001 for both).
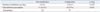
Complication rates were similar in the two study groups (p=0.318), and no intergroup difference was found with respect to complications; that is, wound complications, obstruction, postoperative abdominal pain, pneumonia, intra-abdominal abscess, urinary retention, or re-admission (p=0.936, p=1.000, p=1.000, p=1.000, p=0.288, and p=0.525) (Table 2).
Relationships between duration of antibiotic use and complications showed that 126 patients (88.7%) received 2nd generation cephalosporin, 3 (2.1%) received a combination of 3rd generation cephalosporin, aminoglycosides, and metronidazole, 5 (3.5%) received a combination of 3rd generation cephalosporin, and metronidazole (3.5%), and 6 (4.2%) received tazobactam+piperacillin (4.2%). When patients with or without complication were compared, mean durations of antibiotics use were 3.2±2.4 and 3.9±2.9 days, respectively, being not significantly different (p=0.133) (Table 3).
It is widely known that laparoscopic surgery results in less postoperative pain, earlier recovery, and shorter hospital stays than open surgery. The selective application of outpatient laparoscopic cholecystectomy was advocated as early as 1990,11 and has now become a recognized postoperative strategy after cholecystectomy.12,13,14 Furthermore, an outpatient approach has been suggested after laparoscopic adrenalectomy and laparoscopic splenectomy.15,16
However, no standards have been issued regarding the duration of hospitalization or antibiotic usage after laparoscopic appendectomy for uncomplicated appendicitis, probably because appendicitis is an acute inflammatory infectious disease, therefore, postoperative complications and recovery are largely dependent on underlying patient condition. Furthermore, hospital stay after laparoscopic appendectomy varies by country, surgeon's preference, and culture. In Korea, postoperative hospital stays after appendectomy for uncomplicated appendicitis range from 3.6 to 6.06 days6,7,8,9 and from 2.2 to 3 days in other countries.11,12 These longer hospital stays in Korea probably reflect a generous national public medical insurance system.
Several authors have concluded that outpatient laparoscopic appendectomy for uncomplicated appendicitis is feasible,11,12,17 and reported no increase in complication rates among outpatients. However, the adoption of outpatient laparoscopic appendectomy would not be straightforward in some countries.
In the present study, we analyzed the medical records of 142 patients who underwent laparoscopic appendectomy for uncomplicated appendicitis. Patients were dichotomized by duration of hospitalization after appendectomy about a cut-off of 48 hours. To develop a consensual protocol and suggest a standard length of stay after laparoscopic appendectomy for uncomplicated appendicitis, we examined the safety of short hospital stay after laparoscopic appendectomy. Our analysis revealed no significant differences between the E and L groups in terms of age, body mass index, American Society of Anesthesiology score, or time from emergency room admission to surgery. However, members of the E group resumed an oral diet significantly sooner (1 day vs. 2 days). Traditionally an oral diet is started after flatus passage, but early diet initiation has recently been attempted before flatus passage in uncomplicated situations. Furthermore, an early enteral diet start has been recommended by several parenteral and enteral nutrition societies,18,19 and has been actively adopted after colon surgery. Unfortunately, due to retrospective nature of the present study, no information was available about time to first flatus. Nevertheless, we have tried to start early feeding within 1 day or appendectomy regardless of flatus or bowel motility, because patients who tolerate an early diet can be discharged earlier. In the present study, the E and L groups showed similar complication rates, and no significant increase in the postoperative obstruction rate was observed in the E group (1.9% vs. 2.3%, p=1.00). These findings suggest the feasibility of early discharge, which we attribute to an early diet after laparoscopic appendectomy in patients with uncomplicated appendicitis.
Interestingly, a significant difference was observed between the two study groups in terms of duration of antibiotic use (1 day vs. 2 days in the E and L groups, respectively; p<0.001), but no difference was observed for wound complication (13% vs. 12.5%). One case of pneumonia developed in the L group in a patient that had undergone lung lobectomy for lung cancer, and thus, was at high risk of developing a postoperative lung complication.
However, no significant difference was found between patients that developed a complication and those that did not in terms of duration of antibiotic use (p=0.133), and no significant difference was observed between patients prescribed or not prescribed oral antibiotics with respect to complication rate (p=0.654), suggesting that long-term antibiotic treatment might be unnecessary in preventing post-operative complications.
A major limitation of this study is that it was performed retrospectively without randomization. Therefore, our results are prone to selection bias, particularly regarding discharge. In particular, the initiation of diet was subject to surgeons' preference, and because of a lack of consensus, not all patients were provided an early diet. In addition, discharge times were depended on patients' and surgeons' preferences despite meeting discharge criteria.
In conclusion, the present study suggests that discharge within 48 hours of laparoscopic appendectomy for uncomplicated appendicitis is probably safe and feasible, and does not increase complications. Further studies should be undertaken to determine optimal hospital stay after laparoscopic appendectomy for uncomplicated appendicitis with the objective of reducing treatment costs.
Figures and Tables
References
1. Cash CL, Frazee RC, Smith RW, Davis ML, Hendricks JC, Childs EW, et al. Outpatient laparoscopic appendectomy for acute appendicitis. Am Surg. 2012; 78:213–215.

2. Dubois L, Vogt KN, Davies W, Schlachta CM. Impact of an outpatient appendectomy protocol on clinical outcomes and cost: a case-control study. J Am Coll Surg. 2010; 211:731–737.

3. Jain A, Mercado PD, Grafton KP, Dorazio RA. Outpatient laparoscopic appendectomy. Surg Endosc. 1995; 9:424–425.

4. Frutos MD, Abrisqueta J, Lujan J, Abellan I, Parrilla P. Randomized prospective study to compare laparoscopic appendectomy versus umbilical single-incision appendectomy. Ann Surg. 2013; 257:413–418.

5. Wang CC, Tu CC, Wang PC, Lin HC, Wei PL. Outcome comparison between laparoscopic and open appendectomy: evidence from a nationwide population-based study. PLoS One. 2013; 8:e68662.

6. Lee HJ, Park YH, Kim JI, Choi PW, Park JH, Heo TG, et al. Comparison of clinical outcomes and hospital cost between open appendectomy and laparoscopic appendectomy. J Korean Surg Soc. 2011; 81:321–325.

7. Lee JS, Hong TH, Kim JG. A comparison of the periumbilical incision and the intraumbilical incision in laparoscopic appendectomy. J Korean Surg Soc. 2012; 83:360–366.

8. Shin CS, Kim JI, Roh YN, Choi PW, Heo TG, Park JH. Clinical outcomes and costs of laparoscopic versus open appendectomy for appendicitis. J Surg. 2013; 1:37–42.

9. Kim CB, Kim MS, Hong JH, Lee HY, Yu SH. Is laparoscopic appendectomy useful for the treatment of acute appendicitis in Korea? A meta-analysis. Yonsei Med J. 2004; 45:7–16.

10. Varadhan KK, Neal KR, Lobo DN. Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: meta-analysis of randomised controlled trials. BMJ. 2012; 344:e2156.

11. Reddick EJ, Olsen DO. Outpatient laparoscopic laser cholecystectomy. Am J Surg. 1990; 160:485–487.

12. Swank HA, Eshuis EJ, van Berge Henegouwen MI, Bemelman WA. Short- and long-term results of open versus laparoscopic appendectomy. World J Surg. 2011; 35:1221–1226.

13. Tenconi SM, Boni L, Colombo EM, Dionigi G, Rovera F, Cassinotti E. Laparoscopic cholecystectomy as day-surgery procedure: current indications and patients' selection. Int J Surg. 2008; 6:Suppl 1. S86–S88.

14. Marinis A, Stamatakis E, Tsaroucha A, Dafnios N, Anastasopoulos G, Polymeneas G, et al. Safety and effectiveness of outpatient laparoscopic cholecystectomy in a teaching hospital: a prospective study of 110 consecutive patients. BMC Res Notes. 2010; 3:207.

15. Ramírez-Plaza CP, Perales JL, Camero NM, Rodríguez-Cañete A, Bondía-Navarro JA, Santoyo-Santoyo J. Outpatient laparoscopic adrenalectomy: a new step ahead. Surg Endosc. 2011; 25:2570–2573.

16. Skattum J, Edwin B, Trondsen E, Mjåland O, Raede J, Buanes T. Outpatient laparoscopic surgery: feasibility and consequences for education and health care costs. Surg Endosc. 2004; 18:796–801.

17. Kehagias I, Karamanakos SN, Panagiotopoulos S, Panagopoulos K, Kalfarentzos F. Laparoscopic versus open appendectomy: which way to go? World J Gastroenterol. 2008; 14:4909–4914.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download