Abstract
Purpose
The object of this study was to determine the shortest possible distances of antero-medial (AM) and postero-lateral (PL) guide wire tunnel positions required to prevent femoral bone tunnel communication in double-bundle anterior cruciate ligament (ACL) reconstruction using human cadaver knees.
Materials and Methods
The centers of femoral AM and PL bundles of 16 cadaveric knees were drilled with guide wires and the distances of guide wires, were measured upon entrance into the bone. Femoral tunnel drilling was performed using transportal technique. The diameters of AM and PL graft were 8 mm and 6 mm, respectively. CT scans were taken on each knee, and 3-dimensional models were constructed to identify the femoral tunnel position and to create AM and PL tunnel virtual cylinders. Thickness of the bone bridge between the two tunnels was measured.
Results
In four out of six specimens, in which the guide wires were placed at less than or equal to 9 mm, communication was noted. In specimens with guide wires placed at distances greater than or equal to 10 mm, communication was not noted. The two groups showed a statistically significant difference (p=0.008). In cases where the distance between the AM and PL femoral tunnel guide wires was 12 mm, the bone bridge thickness was greater than 2 mm along the tunnel.
The anterior cruciate ligament (ACL) consists of two bundles, the antero-medial (AM) bundle and the postero-lateral (PL) bundle. Rupture of the ACL is one of the most common ligamentous injuries of the knee.1 Over the past years, various different techniques have been developed to reconstruct the torn ACL under the concept of reproducing the original anatomy of two bundled ACL.2 However, no consensus has developed to date as to which technique is better among various techniques.3 As the focus shifted towards the restoration of the native anatomy of ACL, recent studies on anatomical double bundle-anterior cruciate ligament (DB-ACL) reconstruction increasingly by showed biomechanical advantages of this technique compared to single bundle-anterior cruciate ligament (SB-ACL) reconstruction.4,5,6,7,8,9,10 Unfortunately, however, the anatomical DB-reconstruction technique is more technically demanding and increases the risk of complications compared with the SB technique. One of the complications associated directly with the DB-ACL reconstruction technique is communication of the tunnels. This complication can occur either intraoperatively or postoperatively due to tunnel enlargement. It is a serious complication that jeopardizes knee stability and graft function.11,12,13 Hence, accurate anatomical tunnel placement is an important factor for obtaining optimal clinical results in DB-ACL reconstruction.8,10 Despite its importance, few studies have documented the femoral tunnel distance between the AM and PL bundles necessary to provide sufficient bone bridge thickness resistance against tunnel communication in DB-ACL reconstruction. Additionally, there are no reports on the distance between AM and PL tunnel guide wires required to prevent femoral bone tunnel communication during DB-ACL reconstruction.
The purpose of our study was to evaluate the correlation between intraoperative femoral guide-wire position and femoral bone tunnel communication during DB-ACL reconstruction. We also determined the distance between AM and PL femoral guide wires required to prevent femoral bone tunnel communication during DB-ACL reconstruction. We suggest that a distance of at least 10-mm would have to be preserved to avoid bone tunnel communication between AM and PL femoral tunnel guide wires.
Human cadaveric knees (10 males, 6 females) were kept at -20℃ until use. Specimens were thawed for 24 hours at room temperature before testing. The mean subject age at the time of death was 60.3±8.6 years (range: 47-72 years). The specimens had no gross deformities, flexion contracture, or physiologic hyperextension. The specimen were prepared to include the distal 12 cm of the femur and the proximal 12 cm of the tibia, and all soft tissues structures were carefully dissected except the fibers of ACL. We also used anatomic landmark such as lateral intercondylar ridge to detect accurate ACL footprint. And the perimeter of the femoral ACL footprint was marked using a 1.5 mm drill bit.
Fibers that were relaxed in the ACL when the knee was flexed at 90° were identified as the PL bundle. The center point of the femoral PL bundle insertion site was visually defined and marked with guide wires. The remaining fibers that were taut at 90° of knee flexion were identified as the AM bundle. Tunnel placement was performed by single surgeon using guide wires inserted through the center of the femoral AM and PL footprint of the ACL at a angle of 45° in the axial plane using anglometer to maintain a constant enterance angle for each specimens with knee flexion of 110°. The distance between the AM and PL femoral guide wires was measured with a ruler at the entrance (Fig. 1).
Femoral tunnel drilling was performed using transportal technique with the knee flexed at 110°. Even though all soft tissues are dissected, we drilled tunnel with careful attention in order to avoid iatrogenic damage to the cartilage of medial femoral condyle and tibia plateau, because ideal portal is located superior to the medial joint line approximately 1.5 centimeters medial to the border of the patellar tendon. The reamer diameters of the AM and the PL tunnels were defined and set at 8 mm and 6 mm, respectively, since it is commonly used parameter to standardize for 3-dimensional simulation. Divergent tunnel placement for the double bundles was based on an angle of 45° in the axial plane. The bone bridge between the two tunnels was carefully inspected to ensure whether a tunnel communication occurred or not in the virtual AM tunnel cylinder and the virtual PL tunnel cylinder created by Geomagic® Software (Research Triangle Park, NC, USA). CT scans of each knee were taken. From the CT images, landmark bony morphology such as notch width, and condylar size of each cadaveric knees was measured (Table 1). A 3-dimensional model of each knee was reconstructed using MIMICS® software (Mimics 12.3, Materialise, Belgium) to identify femoral tunnel positions. Geomagic® Software was used to create the virtual AM and PL tunnel cylinders on the femoral side (Fig. 2). Bone bridge thickness between the two tunnels was measured twice on the femoral side at three locations: femur entrance, mid-portion, and exit by two experienced orthopaedic surgeons at 4 weeks apart.
The SPSS software package (SPSS Inc., Version 18, Chicago, IL, USA) was used to perform statistical analyses. Mann-Whitney test was used for comparision of bony morphometery of cadaveric knees. A Fisher's exact test was performed to compare the differences in communication occurrence rates by femoral guide wire distance. The intra and inter observer reliability were calculated using the correlation coefficient. Statistical significance was assumed at p<0.05.
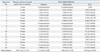
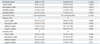
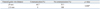
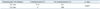
In 4 cadaveric knees (66.7%), tunnel communication caused by bone tunnel drilling was observed on the femoral side at the level of the entrance and mid-portion. This communication occurred when the distance between guide wires was less than or equal to 9 mm between AM and PL tunnel cylinders; images were created by Geomagic Software (Fig. 3). In the femoral tunnels, the mean bone bridge thickness without communication at the level of entrance was 2.10±0.72 mm (range: 1.57-3.89 mm). The mean distance between the mid-portions of AM and PL femoral bone tunnels without communication was 4.45±2.29 mm (range: 4.87-7.17 mm). The mean distance between the exits of AM and PL femoral bone tunnels without communication was 8.10± 2.14 mm (range: 2.98-11.23 mm) (Table 2). In 4 out of 6 specimens (67%) with guide wires spaced less than or equal to 9 mm apart, communication was noticed. In specimens with guide wires space greater than or equal to 10 mm apart, femoral tunnel communication did not occur. There was a statistically significant difference between the two groups (p=0.008) (Table 3). The intra- and inter-observer reliability of the measurement showed an average 0.986 in the intra-observer relationship, and 0.954 in the inter-observer relationship, showing relatively high reliability (Table 4).
When femoral bone bridge thickness is less than or equal to 2 mm, it is assumed that tunnel widening allows for communication. There was a statistically significant difference between communication in groups with guide wire distances of less than or equal to 11 mm and in groups with distances greater than or equal to 12 mm (p=0.003) (Table 5).
The objective of this study was to evaluate the correlation between femoral guide wire position and femoral bone tunnel communication. We also aimed to determine the distance between two femoral guide wires required to prevent femoral bone tunnel communication in DB-ACL reconstruction. Our most important finding was that two thirds of cadaveric knees (67%) displayed tunnel communication after tunnel drilling at AM and PL femoral guide wire distances of less than or equal to 9 mm. This finding indicates that when guide wire distance is less than or equal to 9 mm, there is a higher risk of communication intraoperatively during reaming versus the group with guide wires greater than or equal to 10 mm.
Several studies suggest that in DB-ACL reconstruction technique, AM and PL reconstructed grafts share the load during normal knee range of motion, and that the presence of the PL bundle can restore normal knee rotation more readily.14,15 However, DB-ACL reconstruction technique is technically more demanding and more prone to complications for inexperienced surgeon. In addition, DB-ACL reconstruction technique has relatively limited indications, compared with SB-ACL reconstruction technique.2,16 Especially, the most difficult part of DB-ACL reconstruction is to create two tunnels in the femur while keeping an intact bone bridge between them.11 One of the complications associated directly with the double bundle technique is communication of the femoral tunnels.11,12,13 The plausible etiology of tunnel communication is multifactorial with several mechanical and biological contributing factors.17,18 In this study, we focused on verifying the cause of geometrical tunnel communication associated with bone tunnel bridge thickness according to femoral guide wires distance. Therefore, it was necessary to determine the distance between AM and PL tunnel guide wires required to prevent femoral bone tunnel communication in DB-ACL reconstruction. To our best knowledge, no previous studies have focused on femoral guide wire distance and tunnel communication following DB-ACL reconstruction. The present data indicate that AM and PL femoral tunnel guide wires should be at least 10 mm apart to avoid bone tunnel communication. A few studies on bone bridge thickness following DB-ACL reconstruction only have been reported. Specifically, Basdekis, et al.19 applied CT to evaluate and validate the position of femoral tunnels after DB-ACL reconstruction. This study found that bone bridge thickness at the level of the entrance was 2.9 mm. Lehmann, et al.20 conducted a study on cyclic loading in cadaveric knees to test varying bone bridge thicknesses during DB-ACL reconstruction, and found that a 1-mm bone bridge thickness resulted in significantly reduced structural properties of the graft-femur complex compared to a 2- or 3-mm bone bridge thickness. Hantes, et al.11 applied CT and determined that the well-defined triangular bone bridge established between the AM and PL tunnel at the femoral side had a mean bone bridge thickness of 2.2 (±0.9) mm at the entrance, 5.2 (±2.3) mm at the mid-portion, and 11.4 (±4.5) mm at the exit. This study is an in vitro cadaveric study, and did not consider each specimen's anatomic variations such as notch shape and footprint size. Furthermore, the study defined the size of reaming diameter at 8 mm for AM and 6 mm for PL tunnel, however, surgeons clinically can select different reaming diameter case by case. Some studies suggest that 6 or 7 mm graft thickness is most appropriate for AM bundle,13,21,22 however, we standardized 8 mm tunnel for AM bundle in this experimental cadaveric study because basic science is the foundation for the clinical research and ultimately treatment strategies and also we tried to occupy as much native footprint of AM bundle as possible by graft. The present in vitro cadaveric basic science study is more standardized than the clinical research. Therefore, we could obtain more accurate and credible results, and such results play an important role and are expected to form the foundation of clinical outcomes and strategies of surgical treatments. As mentioned above, we described herein the anatomical femoral AM and PL tunnel position by gross footprint center using anatomic landmark such as lateral intercondylar ridge and perimeter of ACL bundle instead of using a 'Quadrant assessment method' described by Bernard, et al.23 that measures femoral tunnel position using radiographic data. In the present study, radiologic method was not used to determine anatomical ACL footprint center, because the actual arthroscopic operation does not use radiologic modalities for determining each different bundles center of ACL. However, there is a possibility that our technique to determine the ACL footprint center could not represent accurate ACL foot print center, therefore, we cautiously suggest that we found the exact anatomical ACL footprint center in this study. At this point, we need to introduce engineering concepts in order to evaluate distance, based on distance of inserted pins, size of reamer and remaining bone bridge thickness between two tunnels. If the distance between guide wires was greater than 10 mm, by using reaming radii of 4 mm and 3 mm for AM and PL, respectively, the actual reaming should be as expected, and the bone bridge at the entrance should be greater than 2 mm. In this study, we showed that the bone bridge at the entrance was smaller than 2 mm in some cases. The reason for this discrepancy between what was observed and what was expected might be found in the fact that tunnel size was inadequate due to the use of a flexible guide wire and micro-motion during reaming. Hensler, et al.24 found that if a drill angle is vertical to the ACL footprint, the tunnel entrance aperture would be circular and the tunnel length would equal to drill diameter. However, as drill angle increases, tunnel entrance aperture widens and lengthens. If the two tunnels were not parallel and reaming occurred at an angle with one another, bone bridge thickness would be less than expected.
Over the last few decades, many groups reported anatomical DB-ACL reconstructions that have tunnel enlargement complications,11,25 and many studies demonstrated that the majority (75%) of tunnel widening occurs during the first 3 to 6 months.11,17,18,26 Tunnel enlargement could be caused intraoperatively by the surgical procedure, by graft fixation with hardware, or by a multifactorial process early in the postoperative period. Graft tunnel motion may impair bone resorption, contributing to tunnel widening which is caused by bungee cord effect, windshield wiper effect, and redirecting forces at the tunnel aperture.24,27,28 Previous studies suggest that, despite the utilization of different materials and methods, intraoperative or postoperative bone tunnel communication can be avoided with a bone bridge of 2 mm along the tunnel.20,25,29,30 In this study, when guide wire distance was less than or equal to 11 mm, only one specimen's bone bridge thickness was greater than 2 mm at the entrance. When guide pin distance was 12 mm, each specimen's bone bridge thickness was greater than 2 mm along the tunnel. It is assumed that there is a high risk of tunnel enlargement that promotes communication at bone bridge thicknesses of less than 2 mm.20 In these cases, the AM and PL femoral guide wires should be at least 12 mm apart to avoid postoperative bone tunnel communication during DB-ACL reconstruction.
The present study had several limitations that require consideration. First, we used ruler for measuring the distance of enterance of two femoral tunnel instead of caliper. Therefore, bias arising from measurement error is likely to have occurred. Second, there are multifactorial factors that influence the tunnel communication. However, we did not consider other factors, except geometrical distance of guide wires and bone bridge thickness. The third weakness was that the average age of the cadavers (mean age: 60.3±8.6, range: 47-72) was significantly greater than the average age of most patients undergoing DB-ACL reconstruction. Hence, the cadaveric specimens used in the present study might not represent anatomical features and bone quality of femurs in patients undergoing ACL reconstruction. Even though no specimens had osteoarthritic changes, the ages of the specimens should be considered in such anatomical studies. Fourth, the enterance angle of tunnel was fixed at 45° in the axial plane using anglometer to maintain a constancy for each specimen. However, such technique is thought to have several limitations; it does not ensure a repeatable standardized angle for tunnel, and this might result in human error and bias. Consequently, these specialized setting technique for DB-ACL reconstruction might significantly be different from in vivo situation. On the other hand, the present study does have several strong points. Several recent studies have examined the utility of conventional radiography, CT, and MRI for evaluating bone tunnel locations after DB-ACL reconstruction. However, all these imaging methods suffer from various limitations. The present study is the first to display a 3-dimensional image of the whole tunnel position and to report tunnel communication occurrence during DB-ACL reconstruction. The study was conducted using 3-dimensional images instead of 2-dimensional images by 3-dimensional reconstruction to confirm geometry at all ranges, observe tunnel communication, and measure distances more precisely. Our study reflects the level of technical variation that surgeons encounter, such as bone bridge communication that can occur during intraoperative drilling due to micro-motion of the flexible guide pin and inadequate femoral tunnel angles. Moreover, this novel imaging method will contribute to greater accuracy of ACL reconstruction surgery and will help surgeons confirm the success of surgical techniques, thereby improving clinical outcomes.
The technique described hurein for DB-ACL reconstruction will make it possible to avoid bone tunnel communication if AM and PL femoral guide wires are placed at least 10 mm apart, and 12 mm should be kept to preserve 2 mm bone bridge thickness.
Figures and Tables
 | Fig. 1Guide wires were inserted through the center of the femoral anteromedial and posterolateral footprint of the anterior cruciate ligament at angle of 45° in the axial plane on knees flexed at 110°. Two guide wires were inserted in cadaveric femur: (A) Anteroposterior view. (B) Lateral view. |
 | Fig. 2The virtual anteromedial and posterolateral tunnel cylinders were created at the femoral side using Geomagic Software (Research Triangle Park, NC, USA) and bone bridge thickness were measured. (A) Anteroposterior view. (B) Lateral view. |
 | Fig. 3Tunnel communication caused by drilling was observed. (A) At the level of the enterance by gross specimen. (B) Along the whole tunnel using a 3 dimensional virtual cylinder model. |
Table 2
Distance between Anteromedial (AM) and Posterolateral (PL) Femoral Guide Wires at Entrance into the Bone and Bone Bridge Thickness
ACKNOWLEDGEMENTS
This work (RPP-2012-012) was supported by the fund of Research Promotion Program, Gyeongsang National University, Korea, 2012.
References
1. Gianotti SM, Marshall SW, Hume PA, Bunt L. Incidence of anterior cruciate ligament injury and other knee ligament injuries: a national population-based study. J Sci Med Sport. 2009; 12:622–627.

2. Muller B, Hofbauer M, Wongcharoenwatana J, Fu FH. Indications and contraindications for double-bundle ACL reconstruction. Int Orthop. 2013; 37:239–246.

3. Schreiber VM, van Eck CF, Fu FH. Anatomic Double-bundle ACL Reconstruction. Sports Med Arthrosc. 2010; 18:27–32.

4. Fu FH, Shen W, Starman JS, Okeke N, Irrgang JJ. Primary anatomic double-bundle anterior cruciate ligament reconstruction: a preliminary 2-year prospective study. Am J Sports Med. 2008; 36:1263–1274.

5. Mae T, Shino K, Miyama T, Shinjo H, Ochi T, Yoshikawa H, et al. Single-versus two-femoral socket anterior cruciate ligament reconstruction technique: biomechanical analysis using a robotic simulator. Arthroscopy. 2001; 17:708–716.

6. Muneta T, Koga H, Mochizuki T, Ju YJ, Hara K, Nimura A, et al. A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy. 2007; 23:618–628.

7. Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2002; 30:660–666.

8. Yasuda K, Kondo E, Ichiyama H, Tanabe Y, Tohyama H. Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among 3 different procedures. Arthroscopy. 2006; 22:240–251.

9. Neven E, D'Hooghe P, Bellemans J. Double-bundle anterior cruandciate ligament reconstruction: a cadaveric study on the posterolateral tunnel position and safety of the lateral structures. Arthroscopy. 2008; 24:436–440.

10. Tsukada H, Ishibashi Y, Tsuda E, Fukuda A, Toh S. Anatomical analysis of the anterior cruciate ligament femoral and tibial footprints. J Orthop Sci. 2008; 13:122–129.

11. Hantes ME, Liantsis AK, Basdekis GK, Karantanas AH, Christel P, Malizos KN. Evaluation of the bone bridge between the bone tunnels after anatomic double-bundle anterior cruciate ligament reconstruction: a multidetector computed tomography study. Am J Sports Med. 2010; 38:1618–1625.

12. Christel P, Sahasrabudhe A, Basdekis G. Anatomic double-bundle anterior cruciate ligament reconstruction with anatomic aimers. Arthroscopy. 2008; 24:1146–1151.

13. Pombo MW, Shen W, Fu FH. Anatomic double-bundle anterior cruciate ligament reconstruction: where are we today? Arthroscopy. 2008; 24:1168–1177.

14. Zantop T, Wellmann M, Fu FH, Petersen W. Tunnel positioning of anteromedial and posterolateral bundles in anatomic anterior cruciate ligament reconstruction: anatomic and radiographic findings. Am J Sports Med. 2008; 36:65–72.

15. Petersen W, Tretow H, Weimann A, Herbort M, Fu FH, Raschke M, et al. Biomechanical evaluation of two techniques for double-bundle anterior cruciate ligament reconstruction: one tibial tunnel versus two tibial tunnels. Am J Sports Med. 2007; 35:228–234.

16. Steckel H, Starman JS, Baums MH, Klinger HM, Schultz W, Fu FH. The double-bundle technique for anterior cruciate ligament reconstruction: a systematic overview. Scand J Med Sci Sports. 2007; 17:99–108.

17. Lind M, Feller J, Webster KE. Bone tunnel widening after anterior cruciate ligament reconstruction using EndoButton or EndoButton continuous loop. Arthroscopy. 2009; 25:1275–1280.

18. Wilson TC, Kantaras A, Atay A, Johnson DL. Tunnel enlargement after anterior cruciate ligament surgery. Am J Sports Med. 2004; 32:543–549.

19. Basdekis G, Abisafi C, Christel P. Effect of knee flexion angle on length and orientation of posterolateral femoral tunnel drilled through anteromedial portal during anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2009; 25:1108–1114.

20. Lehmann AK, Osada N, Zantop T, Raschke MJ, Petersen W. Femoral bridge stability in double-bundle ACL reconstruction:impact of bridge width and different fixation techniques on the structural properties of the graft/femur complex. Arch Orthop Trauma Surg. 2009; 129:1127–1132.

21. Chae IJ, Bae JH, Wang JH, Jeon J, Park JH. Double-bundle anterior cruciate ligament reconstruction with split Achilles allograft and single tibia tunnel for small ACL tibial footprint: technical note with clinical results. Arch Orthop Trauma Surg. 2013; 133:819–825.

22. Tajima T, Chosa E, Yamamoto K, Yamaguchi N. Arthroscopic anatomical double-bundle anterior cruciate ligament reconstruction for asian patient using a bone-patellar tendon-bone and gracilis tendon composite autograft: a technical note. Sports Med Arthrosc Rehabil Ther Technol. 2012; 4:9.

23. Bernard M, Hertel P, Hornung H, Cierpinski T. Femoral insertion of the ACL. Radiographic quadrant method. Am J Knee Surg. 1997; 10:14–21.
24. Hensler D, Working ZM, Illingworth KD, Thorhauer ED, Tashman S, Fu FH. Medial portal drilling: effects on the femoral tunnel aperture morphology during anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2011; 93:2063–2071.

25. Lee YS, Lee SW, Nam SW, Oh WS, Sim JA, Kwak JH, et al. Analysis of tunnel widening after double-bundle ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2012; 20:2243–2250.

26. Clatworthy MG, Annear P, Bulow JU, Bartlett RJ. Tunnel widening in anterior cruciate ligament reconstruction: a prospective evaluation of hamstring and patella tendon grafts. Knee Surg Sports Traumatol Arthrosc. 1999; 7:138–145.

27. Ahn JH, Park JS, Lee YS, Cho YJ. Femoral bioabsorbable cross-pin fixation in anterior cruciate ligament reconstruction. Arthroscopy. 2007; 23:1093–1099.

28. L'Insalata JC, Klatt B, Fu FH, Harner CD. Tunnel expansion following anterior cruciate ligament reconstruction: a comparison of hamstring and patellar tendon autografts. Knee Surg Sports Traumatol Arthrosc. 1997; 5:234–238.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download