Abstract
Purpose
Pulmonary arterial hypertension (PAH) is an orphan disease showing poor prognosis. The purpose of study was to evaluate clinical factors influencing outcomes in PAH.
Materials and Methods
Patients who were diagnosed with PAH at a single center were reviewed retrospectively. Forty patients (34.9±14.5 years, 80% of female) were enrolled.
Results
Causes were congenital heart disease in 24 (60%), connective tissue disease in 8 (20%) and idiopathic PAH in 6 (15%). Sixteen patients (40%) were WHO functional class III or IV at the time of diagnosis. Twenty seven patients (67.5%) received molecular targeted therapy. During follow-up (53.6±45.5 months), 10 patients (25%) died and 1-, 2-, and 8 year survival rates were 91.3%, 78.7%, and 66.8%, respectively. As expected, median survival of patients with functional class I or II were significantly longer than patients with III or IV (p=0.041). Interestingly, patients with molecular targeted therapy showed longer survival than conventional therapy (p=0.021).
Pulmonary arterial hypertension (PAH) is an orphan disease showing poor prognosis. It results in a progressive increase in pulmonary vascular resistance, ultimately leading to right heart failure and death.1 PAH is defined as a mean pulmonary artery pressure (mPAP) >25 mm Hg at rest and pulmonary capillary wedge or left ventricular end-diastolic pressure <15 mm Hg.2,3
The incidence is rare, therefore, there have been limited study about the etiology, clinical and hemodynamic variables and outcomes of PAH in Korean, and the factors influencing poor prognosis remain to be determined. Conventional therapy of PAH includes warfarin, diuretics, digoxin, oxygen supplementation and high dose calcium channel blockers, but these therapies generally are effective for only a few patients and are not successful in improving long-term survival.4 Recently, many promising new therapeutic options, including prostacyclin analogues, endothelin-1-receptor antagonists, and phosphodiesterase-5 inhibitors, have been introduced, and they improved clinical function and hemodynamic measures and prolonged survival.5
The objectives of this study were to characterize the clinical outcomes and evaluate the factors influencing survival time of the PAH patients in Korean.
This is a retrospective study. The study population included all patients who met the diagnosis criteria of PAH at Gachon University Gil Medical Center from February 2000 to March 2010. The patients with PAH by classification of Dana Point 2008 were included.6 Chronic thromboembolic pulmonary hypertension patients were excluded after confirming the results of right cardiac catheterization with pulmonary angiography, V/Q scan, or chest computed tomography angiography.
PAH was defined as follows: 1) mPAP >25 mm Hg at rest and 2) pulmonary capillary wedge pressure <15 mm Hg at the time of cardiac catheterization.2,3 If cardiac catheterization was not available, tricuspid valve regurgitation (TR) velocity repeatedly >3.5 m/sec on echocardiography in the cases with no pulmonary stenosis was included. Preoperative PAH of congenital heart disease which was reversible and regressed were excluded.
A retrospective data analysis of the medical records was conducted with particular attention to the following findings: clinical history, etiology, symptoms and functional capacity at diagnosis and hemodynamic measures of echocardiography and cardiac catheterization. Functional classification of the patients at the diagnosis was divided from I to IV according to 1998 WHO classification.
Transthoracic echocardiography was performed at the time of diagnosis. The two-dimensional and M-mode echocardiograms were obtained in the left lateral decubitus position according to the recommendation of American Society of Echocardiographpy.7 Three consecutive cycles were averaged for every parameter. Left ventricular (LV) end-diastolic dimension and end-systolic dimension were measured using M-mode echocardiographic recorded from the parasternal long axis view. LV end-diastolic volume and end-systolic volume were measured.
The maximal TR velocity (TR Vmax; in cm/sec) was obtained from continuous-wave Doppler of the TR signal. The Doppler derived systolic PAP (sPAP; in mm Hg) was then calculated from the maximal TR Vmax using the simplified Bernoulli formula as follows: sPAP=4×(TR Vmax)2+right atrial pressure (RAP). RAP was estimated by the response of the inferior vena cava to deep inspiration.8 The mPAP was estimated by the Mahan's equation as follows: mPAP=90-(0.62×acceleration time).9
Right cardiac catheterization was performed in 19 patients (44.2%) at the diagnosis with the use of standard techniques. After base-line hemodynamic variables were measured, the patients received 100% oxygen via facial mask for 10 minutes and the cardiac hemodynamic variables were measured again. After 20 minutes of oxygen interruption-for wash out of oxygen effect, the patients received inhaled iloprost via mouthpiece of nebulizer (10 microgram for 5 minutes) and the same cardiac hemodynamic variables were measured.10,11
On the basis of the hemodynamic response to the short-term vasodilator trial, we classified the patients into 2 groups (responders and non-responders). The criteria for a favorable response to vasoreactivity test included the following: 1) the cardiac output must not change, 2) a significant decrease (>10 mm Hg) in mPAP and the final mPAP is less than 40 mm Hg, 3) a significant decrease in pulmonary vascular resistance index (Rp, >20% from baseline), 4) a significant decrease in pulmonary/systemic vascular resistance ratio (Rp/Rs, >20%), and 5) the final pulmonary vascular resistance index is less than 6 wood unit·m2.
Conventional medical therapy of PAH includes warfarin, diuretics, digoxin, oxygen supplementation and high dose calcium channel blockers, and all patients received conventional therapy. Molecular targeted therapy included prostacyclin analogues, endothelin-1-receptor antagonists, and phosphodiesterase-5 inhibitors. Selected patients received molecular targeted therapy combined with conventional therapy.
Continuous data are presented as mean with standard deviation when distributed normally or as the mean with range otherwise. Discrete data were given as counts or as percentages. The cumulative survival was estimated using the Kaplan-Meier method, and the differences between two groups according to WHO functional classification and treatments were assessed by the log-rank test. Cox proportional regression model was used to analyze independent predictors of survival.
All statistical analyses were performed with the Statistical Package for Social Science (SPSS) 12.0 for Windows (SPSS Inc., Chicago, IL, USA). Values of p<0.05 were considered significant.
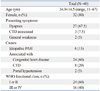
During the study period, a total of 40 patients (8 males and 32 females with a mean age of 34.9±14.5, range 11 to 67) were diagnosed as PAH and successfully followed-up with a mean period of 54.7±48.8 months. The baseline characteristics of the patients are shown in Table 1. Eight male patients were PAH associated with congenital heart disease. All patients except congenital heart disease were females (Table 1).
The causes of PAH were congenital heart disease in 24 patients (60%), connective tissue disease associated in 8 patients (20%), idiopathic PAH in 6 patients (15%), and portal hypertension associated in 2 patients (5%).
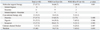
The most common presenting symptom was dyspnea in 27 patients (67.5%) followed by symptoms associated with collagen vascular disease in 3 patients (7.5%), and general weakness in 2 patients (5.0%). Two patients among eight who were associated with connective tissue disease presented with pericarditis besides PAH. Sixteen patients (40%) were WHO functional classification III or IV at the time of diagnosis. The distance of mean six minutes walking test was 298±167 m. Mean N-terminal-pro-Brain Natriuretic Peptide (NT-proBNP) level was 1963±2666 pg/mL. Mean NT-proBNP was higher in patients with WHO functional classification III or IV than in those with I or II without statistical significance (1507±2007 pg/mL vs. 2481±3254 pg/mL, p=0.31) (Table 2).
Echocardiographic hemodynamic profiles were measured at the time of diagnosis. Mean TR velocity was 4.5±0.9 m/sec and right atrial pressure was 11.6±5.6 mm Hg. The mean value of doppler derived systolic pulmonary artery pressure and mPAP by Mahan's equation on echocardiography was 95.5±32.8 mm Hg and 47.9±12.7 mm Hg, respectively. Echocardiographic hemodynamic parameters were compared according to the WHO classification I or II and III or IV (Table 3). There were no significant differences between the two groups except LV end-systolic dimension.
Nineteen patients (47.5%) underwent right cardiac catheterization and vasoreactivity test. The mPAP was 53.8±18.4 mm Hg (range 28-87 mm Hg), and only 3 patients (7.5%) responded to vasodilator in vasoreactivity test. These three patients received calcium channel blocker. Two patients of them did not show improvement, therefore, they received molecular targeted therapy (bosentan). One patient showed improvement of functional classification.
Of 40 patients, 27 patients (67.5%) received molecular targeted therapy combined with conventional therapy. Eight patients received inhaled iloprost and 11 patients received bosentan as a first line molecular targeted therapy. Eight patients received inhaled iloprost at first and then changed to bosentan due to treatment failure. On the other hand, 13 patients (32.5%) received only conventional therapy, including anticoagulation, digoxin, furosemide and spironolactone. The proportion who received molecular targeted therapy was similar between patients with WHO functional classification I or II and patients with III or IV [66.7% (16/24) vs. 68.8% (11/16), p=0.89] (Table 4).
Mean clinical follow-up duration was 53.6±45.5 months and 21 patients (52.5%) finished 3 year follow-up. Ten of 40 patients (25.0%) died during follow-up. The most common cause of death was right ventricular failure due to disease progression in six patients, followed by septic shock in two patients, a cerebral infarction in one patient, and aggravation of acute renal failure in one patient.
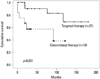
1-, 2-, and 8-year survival rates from the diagnosis were 91.3%, 78.7%, and 66.8%, respectively. Median overall survival time of patients with WHO functional classification I or II was significantly longer than patients with III or IV (p=0.041) (Fig. 1). And the patients with molecular targeted therapy showed significantly longer median overall survival time than that of patients with conventional therapy only (p=0.021) (Fig. 2). Death rate was not significantly different in patients who were treated with bosentan and those with iloprost [6.3% (1/16) vs. 27.3% (3/11), p=0.273]. Cox proportional regression was performed incorporating gender, WHO functional classification and molecular targeted therapy. The molecular targeted therapy was statistically associated with better clinical survival (HR 0.271; 95% CI; 0.074-0.992, p=0.049), and WHO functional classification III or IV was associated with poor survival (HR 3.379; 95% CI; 0.874-13.069, p=0.078) with borderline significance.
Our present data showed that WHO functional class at the time of diagnosis and molecular targeted therapy can be a predictor of survival.
The US National Institutes of Health registry of patients with primary pulmonary hypertension records a median life expectancy of 2.8 years (95% CI, 1.9 to 3.7 years) from diagnosis. Estimated 1-, 3-, 5-year survival rates were 68%, 48%, and 34%, respectively.12 Although the clinical cause of death is highly variable and spontaneous regression has been sometimes described, survival rates are usually poor, averaging only three years after diagnosis.13 Our study showed somewhat higher survival rates compared to previous study, and it appeared to be because we included patients of PAH associated with grown-up congenital heart disease. Another reason of better survival is more common use of molecular targeted therapy (62.8%) than previous studies. Actually 5-year survival among epoprostenol-treated patients has been reported to be 47% to 55% in primary pulmonary hypertension.14,15
There are currently three major drug classes available for the molecular targeted treatment of PAH. As a potent vasodilator, prostacyclin has been shown to improve hemodynamic function, exercise tolerance, and the quality of life.16 Epoprostenol has been more effective than conventional treatment and has greatly improved the life expectancy of patients with severe pulmonary hypertension.5,17 Treprostinil, which can be given either as a continuous intravenous or subcutaneous infusion, also significantly improved functional capacity and hemodynamic values, compared to placebo, in patients with pulmonary hypertension.18 Similar results were shown with aerosolized prostacyclin, iloprost.19 Bosentan, an orally active non-peptide antagonist of both endothelin receptor subtypes (ETA and ETB), improved pulmonary hemodynamics and exercise tolerance.20 Bosentan monotherapy for patients with idiopathic PAH resulted in estimated 1- and 2-year survival rates of 85% and 70%, respectively.21 It was also effective in Korean PAH patients for improving right ventricular hemodynhamics, exercise and functional capacity.22 Phosphodiesterase-5 inhibitors, such as sildenafil, have an acute pulmonary vasodilator effect. Sildenafil causes an increase in cyclic guanosine monophosphate levels, which have a role in causing pulmonary vasodilation. In Korea, only few drugs, including inhaled iloprost, oral beraprost, and oral bosentan, were approved currently for PAH treatment.23 According to the current guidelines, in the absence of acute vasodilator response or absence of long-term response to calcium channel blocker, specific PAH targeting therapies for endothelial dysfunction are indicated.24,25 Sequential combination therapy including three classes of drug was proposed. More aggressive therapeutic approach with combination therapy may be more effective to improve hemodynamics in severe PAH patients,26 however, there are some limitations in aggressive combination therapy due to insurance problem in Korea.
Several factors which determine survival time in patients with PAH were evaluated.12,27 The WHO functional classification at presentation has been reported as the significant clinical predictors of mortality and survival for patients with PAH.28 Even though the patients received molecular targeted therapy, patients who do not show improvement in WHO functional classification after treatment also showed poor prognosis compared with patients improving to functional class I or II.14 Other clinical factor associated with poor survival included the presence of Raynaud phenomenon.12 Hemodynamic variables include elevated mPAP, decreased cardiac index, and decreased diffusing capacity for carbon monoxide (DLCO).12 In our present study, patients with WHO functional classification I or II and patients who received molecular targeted therapy showed significantly longer survival time.
The gender ratio of adult women to men with PAH has been reported to be 1.7-3:1,13,29 and our study showed the ratio of 4.4:1. Of the PAH patients, idiopathic PAH showed that female was exclusive as 8:1 in Korean.30 Our study showed similar results.
Our study has some limitations. First, the current study was a retrospective study in a single center. Second, enrollment period was relatively long. Nevertheless, our study showed a valuable data for the perspectives, and further study is necessary to investigate the clinical characteristics and outcomes of PAH in larger groups of patients, including multi-centers throughout the country. Cardiac catheterization for the confirmation of PAH was done in only half of the patients, however, noninvasive echocardiography is also a feasible tool for evaluation of pulmonary arterial pressure.2
In conclusions, poor WHO functional classification at the time of diagnosis which reflects advanced disease has a prognostic factor in survival time, and molecular targeted therapy could significantly improve the survival time. Therefore, early screening by multi-disciplinary approach with cardiologist, pediatric cardiologist, pulmonologist and rheumatologist and referral to the expert center is crucial to improve the prognosis. Proper management with molecular targeted therapy in selected patients is important to improve outcome. Randomized prospective study of treatment with molecular targeted agent is necessary.
Figures and Tables
Fig. 1
Median overall survival time of patients by NYHA functional classification. Patients with NYHA class I or II at the time of diagnosis showed significantly better survival than those with more severe functional class.
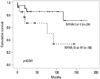
Fig. 2
Median overall survival time of patients according to the treatment. Patients with molecular targeted therapy showed significantly better survival than those with conventionally therapy only.
References
2. Badesch DB, Champion HC, Sanchez MA, Hoeper MM, Loyd JE, Manes A, et al. Diagnosis and assessment of pulmonary arterial hypertension. J Am Coll Cardiol. 2009; 54:1 Suppl. S55–S66.

4. Weir EK, Rubin LJ, Ayres SM, Bergofsky EH, Brundage BH, Detre KM, et al. The acute administration of vasodilators in primary pulmonary hypertension. Experience from the National Institutes of Health Registry on Primary Pulmonary Hypertension. Am Rev Respir Dis. 1989; 140:1623–1630.

5. Barst RJ, Rubin LJ, Long WA, McGoon MD, Rich S, Badesch DB, et al. A comparison of continuous intravenous epoprostenol (prostacyclin) with conventional therapy for primary pulmonary hypertension. N Engl J Med. 1996; 334:296–301.

6. Simonneau G, Robbins IM, Beghetti M, Channick RN, Delcroix M, Denton CP, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2009; 54:1 Suppl. S43–S54.

7. Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978; 58:1072–1083.

8. Kircher BJ, Himelman RB, Schiller NB. Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardiol. 1990; 66:493–496.

9. Dabestani A, Mahan G, Gardin JM, Takenaka K, Burn C, Allfie A, et al. Evaluation of pulmonary artery pressure and resistance by pulsed Doppler echocardiography. Am J Cardiol. 1987; 59:662–668.

10. Opitz CF, Blindt R, Blumberg F, Borst MM, Bruch L, Leuchte H, et al. [Pulmonary hypertension: hemodynamic evaluation: hemodynamic evaluation - recommendations of the Cologne Consensus Conference 2010]. Dtsch Med Wochenschr. 2010; 135:Suppl 3. S78–S86.
11. Jing ZC, Jiang X, Han ZY, Xu XQ, Wang Y, Wu Y, et al. Iloprost for pulmonary vasodilator testing in idiopathic pulmonary arterial hypertension. Eur Respir J. 2009; 33:1354–1360.

12. D'Alonzo GE, Barst RJ, Ayres SM, Bergofsky EH, Brundage BH, Detre KM, et al. Survival in patients with primary pulmonary hypertension. Results from a national prospective registry. Ann Intern Med. 1991; 115:343–349.
13. Olivari MT. Primary pulmonary hypertension. Am J Med Sci. 1991; 302:185–198.
14. Sitbon O, Humbert M, Nunes H, Parent F, Garcia G, Hervé P, et al. Long-term intravenous epoprostenol infusion in primary pulmonary hypertension: prognostic factors and survival. J Am Coll Cardiol. 2002; 40:780–788.

15. McLaughlin VV, Shillington A, Rich S. Survival in primary pulmonary hypertension: the impact of epoprostenol therapy. Circulation. 2002; 106:1477–1482.
16. Humbert M, Sitbon O, Simonneau G. Treatment of pulmonary arterial hypertension. N Engl J Med. 2004; 351:1425–1436.

17. Barst RJ, Rubin LJ, McGoon MD, Caldwell EJ, Long WA, Levy PS. Survival in primary pulmonary hypertension with long-term continuous intravenous prostacyclin. Ann Intern Med. 1994; 121:409–415.

18. Simonneau G, Barst RJ, Galie N, Naeije R, Rich S, Bourge RC, et al. Continuous subcutaneous infusion of treprostinil, a prostacyclin analogue, in patients with pulmonary arterial hypertension: a double-blind, randomized, placebo-controlled trial. Am J Respir Crit Care Med. 2002; 165:800–804.

19. Olschewski H, Simonneau G, Galiè N, Higenbottam T, Naeije R, Rubin LJ, et al. Inhaled iloprost for severe pulmonary hypertension. N Engl J Med. 2002; 347:322–329.

21. Galiè N, Torbicki A, Barst R, Dartevelle P, Haworth S, Higenbottam T, et al. Guidelines on diagnosis and treatment of pulmonary arterial hypertension. The Task Force on Diagnosis and Treatment of Pulmonary Arterial Hypertension of the European Society of Cardiology. Eur Heart J. 2004; 25:2243–2278.
22. Sohn DW, Kim HK, Kim MA, Song YW, Noh CI, Kim DK, et al. Beneficial and adverse effects of bosentan treatment in Korean patients with pulmonary artery hypertension. Korean Circ J. 2009; 39:105–110.

23. Chung WJ. Treatment of pulmonary hypertension. Korean J Med. 2010; 78:28–35.
24. Galiè N, Hoeper MM, Humbert M, Torbicki A, Vachiery JL, Barbera JA, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension: the Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS), endorsed by the International Society of Heart and Lung Transplantation (ISHLT). Eur Heart J. 2009; 30:2493–2537.
25. Task Force for Diagnosis and Treatment of Pulmonary Hypertension of European Society of Cardiology (ESC). European Respiratory Society (ERS). International Society of Heart and Lung Transplantation (ISHLT). Galiè N, Hoeper MM, Humbert M, Torbicki A, Vachiery JL, et al. Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J. 2009; 34:1219–1263.

26. Kemp K, Savale L, O'Callaghan DS, Jaïs X, Montani D, Humbert M, et al. Usefulness of first-line combination therapy with epoprostenol and bosentan in pulmonary arterial hypertension: an observational study. J Heart Lung Transplant. 2012; 31:150–158.

27. Fuster V, Steele PM, Edwards WD, Gersh BJ, McGoon MD, Frye RL. Primary pulmonary hypertension: natural history and the importance of thrombosis. Circulation. 1984; 70:580–587.

28. Lee WS, Kim KH, Jeong DH, Lee KH, Hong SN, Park HW, et al. Clinical characteristics and prognostic factors of patients with severe pulmonary hypertension. Korean Circ J. 2007; 37:265–270.

29. Rich S, Dantzker DR, Ayres SM, Bergofsky EH, Brundage BH, Detre KM, et al. Primary pulmonary hypertension. A national prospective study. Ann Intern Med. 1987; 107:216–223.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download