Abstract
Purpose
Autophagy has been reported to be involved in treatment failure in tumor. We aimed to evaluate autophagy activity in tumor tissue and compare them between the recurrence and non-recurrence groups.
Materials and Methods
We analyzed expressions of autophagy-related proteins in tumor tissues which were obtained from pulmonary metastases of colorectal cancer patients by Western blot. We also analyzed autophagosomes by transmission electron microscopy.
Autophagy is a catabolic digestion process of cellular organelles1 and plays an important role in protecting cells from adverse conditions2,3,4,5,6 by degrading and recycling of cytosolic, or aggregated proteins, as well as excess or defective organelles. The process of autophagy has been implicated in both cellular survival and cell death.7,8 The role of autophagy in tumor is commonly expressed by double-edged sword.9,10 Before the development of a tumor, autophagy is considered to act as a tumor suppressor; however, after tumor develops, it supports the growth of the tumor. Specifically, autophagy activities have been reported to be enhanced in response to metabolic stress caused by chemotherapy or radiation as a cell survival mechanism, contributing to treatment resistance in cancer.9,10,11,12 Furthermore, elevated autophagy activity has been reported to be associated with aggressiveness in cancer tissue.13
Colorectal cancer (CRC) brings about metastases in 60% of the cases, with involvement of the liver (40%), lung (15%), or both (10%).14 Although development of chemotherapeutic regimens combined with surgical resection has made it possible to treat the metastatic CRC, half of patients develop local or distant recurrence.15 The treatment failure in some individuals is due to the development of resistance, and the mechanisms involved in chemotherapy resistance remain unknown.
We hypothesized that autophagy may contribute to the treatment failure of cancer patients. To test this hypothesis, we investigated the autophagy activity in tumor tissue obtained from patients who had pulmonary metastasis from CRC.
To test autophagy-related activity in tumor tissue, 10 pulmonary metastasis tissues from CRC patients who had over 12 months follow up period were selected from prospective collections of the Department of Thoracic and Cardiovascular Surgery, Yonsei University College of Medicine. Patients underwent curative intent pulmonary resection for metastasis from CRC from November 2011. Clinical records were reviewed retrospectively. The research has been approved by the Institutional Review Board of Yonsei University College of Medicine, and all the patients had signed an informed consent. Tumor specimens were obtained at surgery. The specimens were prepared for protein extraction and electron microscopy.
Tumor tissues were homogenized in 1 mL of RIPA buffer (50 mM Tris-HCl, pH 7.5, 0.1% SDS, 2 mM EDTA, 150 mM NaCl, 1% sodium deoxycholate, 1% Triton X-100) and protease inhibitor cocktail. The homogenate was incubated for 20 minutes on ice and then centrifuged at 14000 rpm for 15 minutes at 4℃. The supernatant was collected and the same volume of 5X SDS buffer was added to the supernatant. The mixture was then boiled for 5 minutes and stored at -80℃. Proteins were separated by sodium dodecy1 sulfate polyacrylamide gel electrophoresis (SDS-PAGE) on 8-16% polyacrylamide gels. After electrophoresis, proteins were transferred to PVDF membranes (Millipore Corporation, Billerica, MA, USA), membranes were blocked in 5% nonfat milk, in Tris-buffered saline containing 0.05% Tween-20 (TBST), at room temperature for 1 hour. The membranes were then incubated with a rabbit monoclonal antibody against LC3 (1:2000 diluted in TBST, Novus, Santa Cruz, CA, USA) overnight at 4℃ and washed five times with TBST for 10 minutes each at room temperature. Membranes were then incubated with horseradish peroxidase-conjugated anti-rabbit secondary antibody (1:2000 dilution in TBST, Santa Cruz, CA, USA) at 37℃ for 1 hour and were washed five times with TBST for 10 minutes each at room temperature. Membranes were treated with ECL (Thermo Scientific, Rockford, IL, USA) reagent and exposed to photographic film. Each band was quantified using densitometry, and the results were shown as relative expression of each protein from different samples compared to that of control sample.
After thermal stresses for 12 hours, each sample was fixed with 2% glutaraldehyde-paraformaldehyde in 0.1 M phosphate buffer (PB), pH 7.4 for 2 hours and washed three times for 30 minutes each in 0.1 M PB. Samples were then postfixed with 1% OsO4 dissolved in 0.1 M PB for 2 hours and dehydrated in an ascending gradual series (50-100%) of ethanol and infiltrated with propylene oxide. Specimens were embedded using a Poly/Bed 812 kit. After pure fresh resin embedment and polymerization at 60℃ in an electron microscope oven (TD-700, DOSAKA, Kyoto, Japan) for 24 hours, 350 nm thick sections were cut and stained with toluidine blue for light microscopy. Next, 70 nm thin sections were double stained with 7% uranyl acetate and lead citrate for contrast staining. The sections were cut by a LEICA Ultracut UCT Ultra-microtome (Leica Microsystems, Wetzlar, Germany). All of the thin sections were observed by transmission electron microscopy (JEM-1011, JEOL, Tokyo, Japan) at an acceleration voltage of 80 kV.
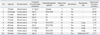
Clinical features of the cases are summarized in Table 1. Five patients experienced recurrence during the follow up time. All recurrences occurred in lung except one case. All 10 patients had been treated by pulmonary resection and chemotherapy before or after operation.
To investigate whether autophagy activity correlates with treatment failure in patients with pulmonary metastasis from CRC, we analyzed the protein level of LC3B-II which is a hallmark of autophagy by Western blotting. Tumor tissues of patients who experienced recurrence showed increased level of LC3B-II compared with tissues from patients who had no recurrence (p<0.05) (Fig. 1). At the same time, we analyzed the protein levels of p62/sequestosome1 (SQSTM1) which is degraded in the autolysosome, thus testing an another marker of autophagy flux. Tumor tissues of patients who experienced recurrence showed trends of decreased level of p62/SQSTM1 compared with tissues from patients who had no recurrence (p=0.201) (Fig. 2). On the other hand, autophagy activity of peri-tumor tissue showed no difference between no recurrence and recurrence group (p=0.797) (Fig. 3).
Transmission electron microscopy, another gold standard assay of autophagy showed a marked accumulation of autophagosomes in cells of treatment failed patients (p<0.05), where cytoplasmic material and/or membrane vesicles were encapsulated in vacuoles (black arrows, Fig. 4). These results indicate that increased autophagy activity is associated with treatment failure in patients after combined chemotherapy and surgical resection.
In this study, we showed that autophagy activities were enhanced in tumor tissue from recurrence group compared with non-recurrence group, suggesting that autophagy activity could be one of the mechanisms associated with treatment failure in patients with pulmonary metastasis from colorectal cancer. To the best of our knowledge, the present study is the first to correlate autophagy activity and treatment failure in tumor tissue obtained from pulmonary metastasis of colorectal cancer.
Autophagy is a catabolic digestion process of cellular organelles1, and essential for protecting cells from adverse conditions.2,3,4,5,6 The process of autophagy has been implicated in both cellular survival and cell death.7,8 Cytoplasmic organelles are engulfed by double membrane structures and conveyed to lysosomes/vacuoles for degradation and recycling during the process. LC3 is autophagy-related protein that is associated with autophagosome membranes. The cytoplasmic form (LC3B-I) is processed and recruited to autophagosomes, where LC3B-II is produced by proteolysis and lipidation. The protein p62/SQSTM1 acts as an adaptor to target ubiquinated protein by binding both ubiquitin and LC3.16 Following the binding of p62/SQSTM1 to LC3B-II, the autophagosome completes and fuses with lysosomes, resulting in the degradation of p62/SQSTM1. Thus, p62/SQSTM1 degradation can be used as an another marker of autophagy flux.17 To assess the autophagy activity, therefore, monitoring of protein levels of LC3B-II and p62/SQSTM1 by Western blot and confirming the ultrastructure of autophagic vacuoles by electron microscopy are essential, as described in the present study. Recently, autophagy has been suggested to explain for the mechanism of treatment resistance in cancer patients. However, the role of autophagy in tumor is controversial, and has commonly been described as a double-edged sword because it functions both as a tumor suppressor and a protector of cancer cell.9,10 Specifically, after a tumor develops, autophagy acts to support the persistence of the tumor. According to many studies, autophagy activities are enhanced in response to treatment such as chemotherapy and radiation, contributing to treatment resistance in cancer cell.9,10,11,12 In addition, autophagy has been reported to correlate with tumor aggressiveness, including tumor differentiation, growth pattern of the tumor margin, pN, pstage as well as vessel and nerve plexus invasion in colorectal cancer.13 In the present study, we showed that autophagy was enhanced in recurrence group. This might be related with chemotherapy resistance or tumor aggressiveness. However, we could not confirm underlying mechanism of this treatment failure. To assess the underlying mechanism, further study is needed with more patient data.
Most of the understanding on the role of autophagy in cancer have come from the studies with cancer cell lines expressing autophagy markers. There is, however, little knowledge regarding the autophagy in clinical tumor samples; especially the extent of which varies depending on tumor tissues. To test our hypothesis, therefore, we measured autophagy activity in tumor tissues obtained from pulmonary metastasis of colorectal cancer patients who were followed up for over one year. To the best of our knowledge, this is the first report on enhanced autophagy activity in human metastatic lung cancer tissue.
Figures and Tables
Fig. 1
Increased autophagy activity (LC3II) correlates with treatment failure of pulmonary metastasis in colorectal cancer patients. (A) Western blot analysis for LC3B-II protein in tumors of CRC patients. The levels of LC3B-II were higher in tumor tissues from patients who had experienced recurrence than tissues from patients who had no recurrence. (B) Expression intensity of Western blot was measured by image J program. The data are mean±SEM (*p<0.05). CRC, colorectal cancer; SEM, standard error of mean.

Fig. 2
Decreased p62/SQSTM1 correlates with treatment failure of pulmonary metastasis in colorectal cancer patients. (A) Western blot analysis for p62/SQSTM1 in tumors of CRC patients. The p62/SQSTM1 expressions of tumor tissue from patients who had experienced recurrence showed trends of lower levels than tissues from patients who had no recurrence. (B) Expression intensity of Western blot was measured by image J program. The data are mean±SEM (p=0.201). CRC, colorectal cancer; SEM, standard error of mean.

Fig. 3
Autophagy activity (LC3II) of peri-tumor tissue shows no difference between no recurrence and recurrence group. (A) Western blot analysis for LC3B-II protein in peri-tumors of CRC patients. The levels of LC3B-II were not different in both no recurrence and recurrence group. (B) Expression intensity of Western blot was measured by image J program. The data are mean±SEM (p=0.797). CRC, colorectal cancer; SEM, standard error of mean.

Fig. 4
Autophagy vacuoles in tumor tissue from pulmonary metastasis in colorectal cancer patients by electron microscopy. (A) Electron micrographs showing ultrastructure of tumor tissue. Arrows indicate double-membraned autophagic vacuoles (magnification, ×20000). (B) Quantification of autophagic vacuoles in tumor cells was performed. The number of autophagic vacuoles in each cell was counted. The data are mean±SEM (*p<0.05). N, no recurrence; R, recurrence; SEM, standard error of mean.

References
1. Maiuri MC, Zalckvar E, Kimchi A, Kroemer G. Self-eating and self-killing: crosstalk between autophagy and apoptosis. Nat Rev Mol Cell Biol. 2007; 8:741–752.

2. Papandreou I, Lim AL, Laderoute K, Denko NC. Hypoxia signals autophagy in tumor cells via AMPK activity, independent of HIF-1, BNIP3, and BNIP3L. Cell Death Differ. 2008; 15:1572–1581.

3. Abedin MJ, Wang D, McDonnell MA, Lehmann U, Kelekar A. Autophagy delays apoptotic death in breast cancer cells following DNA damage. Cell Death Differ. 2007; 14:500–510.

4. Sato K, Tsuchihara K, Fujii S, Sugiyama M, Goya T, Atomi Y, et al. Autophagy is activated in colorectal cancer cells and contributes to the tolerance to nutrient deprivation. Cancer Res. 2007; 67:9677–9684.

5. Degenhardt K, Mathew R, Beaudoin B, Bray K, Anderson D, Chen G, et al. Autophagy promotes tumor cell survival and restricts necrosis, inflammation, and tumorigenesis. Cancer Cell. 2006; 10:51–64.

6. Katayama M, Kawaguchi T, Berger MS, Pieper RO. DNA damaging agent-induced autophagy produces a cytoprotective adenosine triphosphate surge in malignant glioma cells. Cell Death Differ. 2007; 14:548–558.

7. Shintani T, Klionsky DJ. Autophagy in health and disease: a double-edged sword. Science. 2004; 306:990–995.

9. Chen N, Karantza-Wadsworth V. Role and regulation of autophagy in cancer. Biochim Biophys Acta. 2009; 1793:1516–1523.

10. White E, DiPaola RS. The double-edged sword of autophagy modulation in cancer. Clin Cancer Res. 2009; 15:5308–5316.

11. Mathew R, Karantza-Wadsworth V, White E. Role of autophagy in cancer. Nat Rev Cancer. 2007; 7:961–967.

12. Lum JJ, Bauer DE, Kong M, Harris MH, Li C, Lindsten T, et al. Growth factor regulation of autophagy and cell survival in the absence of apoptosis. Cell. 2005; 120:237–248.

13. Zheng HY, Zhang XY, Wang XF, Sun BC. Autophagy enhances the aggressiveness of human colorectal cancer cells and their ability to adapt to apoptotic stimulus. Cancer Biol Med. 2012; 9:105–110.
15. Chao YK, Chang HC, Wu YC, Liu YH, Hsieh MJ, Chiang JM, et al. Management of lung metastases from colorectal cancer: video-assisted thoracoscopic surgery versus thoracotomy--a case-matched study. Thorac Cardiovasc Surg. 2012; 60:398–404.

16. Johansen T, Lamark T. Selective autophagy mediated by autophagic adapter proteins. Autophagy. 2011; 7:279–296.

17. Klionsky DJ, Abeliovich H, Agostinis P, Agrawal DK, Aliev G, Askew DS, et al. Guidelines for the use and interpretation of assays for monitoring autophagy in higher eukaryotes. Autophagy. 2008; 4:151–175.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download