Abstract
Silicosis had been considered for decades as an illness with manifestations of lung fibrosis due to inhalation of overconcentrated SiO2 dust. To the best of our knowledge, studies have yet to report SiO2 deposits in any other tissues and organs. In the present case, while performing bilateral artificial total hip arthroplasty for one patient, we found that the articular cartilage of the bilateral femoral head was black. Therefore, specimens thereof were sent for pathological examination. Pathological examination (immunohistochemistry) and polarized light microscopy revealed the presence of considerable brown, acicular, rhombic, and crumb-like crystals. The crystals were mainly composed of SiO2. SiO2 could deposit in vessels and femoral head cartilage via blood circulation.
Silicosis had been considered for decades as an illness with manifestations of lung fibrosis due to inhalation of overconcentrated SiO2 dust. Many studies have shown that silicotic nodules can form in other tissues and organs, including the liver, kidneys, spleen, heart, abdominal lymph nodes, and so on.1,2,3,4,5,6,7,8 However, none have reported on SiO2 deposits in vessels and femoral head cartilage.
A 50-year-old patient was admitted to the Department of Orthopedics at our hospital. He had complained of pain in the left hip for more than 3 years and in the right hip for more than 1 year. The symptoms had deteriorated with joint dysfunction for 2 months. He had no history of hypertension or diabetes mellitus and he did not smoke or drink. The patient had worked as a coal miner for more than 10 years.
Upon physical examination, we noted rachioscoliosis to the right. Intervertebral space had no tenderness or percussion pain. Spinal mobility was normal. His pelvis tilted to the right and the left hip joint was flexion deformed. Sensation, locomotion, and circulation of the four limbs were good. Routine blood test, liver and renal function, E6A, ESR, CRP, HLA-B27, ASO, and RHF were all in their normal ranges. Radiograph of the patient's lungs revealed the lung markings of increased and thick bilateral lungs, in addition to mottled unclear edges and diffuse distribution of high density material in both lungs. The radiograph was consistent with early silicosis (Fig. 1). Radiograph and CT of the pelvis and bilateral hip joints revealed bilateral avascular necrosis of the femoral head, bilateral degeneration of hip joints, and subluxation of left hip joint. Accordingly, we diagnosed the patient with bilateral avascular necrosis of the femoral head, bilateral degeneration of hip joints, and subluxation of left hip joint.
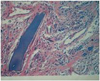
Thereafter, we performed bilateral artificial total hip arthroplasty. During the operation, we found that the capsula articularis coxae, synovial membrane, and articular cartilage of the bilateral femoral head, as well as the vessels of bilateral greater trochanter, were black (Figs. 2 and 3). These specimens were sent for pathological examination. Pathological examination (immunohistochemistry) and polarized light microscopy revealed chronic synovitis and proliferation of granuloma, as well as the presence of considerable brownish acicular, rhombic, and crumb-like crystals. At their edges, giant cell reactions of foreign-bodies were found. The crystals mainly comprised SiO2 (Fig. 4).
In modern medicine, silicosis is considered an illness with main manifestations of lung fibrosis due to inhalation of overconcentrated SiO2 dust.1 SiO2 dust destroys alveolar macrophages, thus inducing pathological changes indicative of silicosis. So far, there has been no case report about SiO2 deposits in vessels or cartilages. The anatomical factors of the femoral head and neck are beneficial to silica deposition. First, the femoral head is widely covered by articular cartilage, thus making its blood supply the end of the circulation. Second, its vessels supply nutrients to thread joint capsules, and then the femoral neck and the bone at the junction of the head and neck. The stroke of nutrient vessels is long and blood flow is slow. All of the above conditions are advantageous to silica deposition.
It is highly likely that two mechanisms are involved in the induction silica deposition in the vessels and femoral head cartilage: first, at the initial inhalation of silica dust, the function of the lungs in the lymphatic system remained normal, and silica dust and dust cells were carried to the lung lymph nodes by lymphatic ducts, and then to the right or left angle of the jugular vein. Subsequently, they reached the vessels of the hip and femoral head via pulmonary and systemic circulation. As well, silica dust inhaled into the alveoli through the respiratory system caused pressure in the alveolar to increase sharply, and free silicon dioxide particles entered the intravascular system, finally reaching the vessels of hip and femoral by blood circulation. Deposited in the vessels of the greater trochanter and cartilages of the femoral head, SiO2 particles ultimately cause avascular necrosis of the femoral head.
In this case, we clearly recognized that the effects of SiO2 were not confined only to the lungs, but also other tissues and organs through blood circulation, inducing pathological changes. It is, therefore, appropriate to consider silicosis as an occupational disease.
Figures and Tables
Fig. 1
Radiograph of the lungs: lung markings of both lungs are increased and thick; mottled, unclear edges and diffuse distribution of high density material in the bilateral lungs are visible. The radiograph is consistent with early silicosis.

Fig. 4
Pathological examination (immunohistochemistry) and polarized light microscopy: chronic synovitis and proliferation of granuloma are visible under a microscope. Note the considerable amounts of brownish acicular, rhombic, and crumb-like crystals. At their edges, giant cell reactions of foreign-bodies are seen. Crystals mainly comprised SiO2 (H&E ×100).
References
1. Ambrosi L. [Histologic aspects of the spleen in silicosis patients]. Med Lav. 1966; 57:10–19.
2. Ambrosi L. [Histologic aspects of the liver in silicosis patients]. Med Lav. 1965; 56:795–804.
3. Ambrosi L. [Histologic aspects of the kidney in silicosis]. Med Lav. 1965; 56:716–726.
4. Ambrosi L. [Histological aspects of the heart in silicotic patients]. Med Lav. 1966; 57:104–110.
5. Carmichael GP Jr, Targoff C, Pintar K, Lewin KJ. Hepatic silicosis. Am J Clin Pathol. 1980; 73:720–722.

6. Autio L, Turunen M, Lahtiharju A. Experimental silica cirrhosis in dog. Ann Med Exp Biol Fenn. 1964; 42:173–176.
7. Roperto F, Troncone A, Tranquillo A, Galati P. Extrapulmonary silicosis in two water buffaloes. J Comp Pathol. 1995; 112:97–103.

8. Montaldo G, Onnis C, Montaldo S. [Pneumosilicosis]. Arch De Vecchi Anat Patol. 1976; 61:487–495.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download