Abstract
Purpose
Endoscopic submucosal dissection (ESD) is a technically difficult and lengthy procedure requiring optimal depth of sedation. The bispectral index (BIS) monitor is a non-invasive tool that objectively evaluates the depth of sedation. The purpose of this prospective randomized controlled trial was to evaluate whether BIS guided sedation with propofol and remifentanil could reduce the number of patients requiring rescue propofol, and thus reduce the incidence of sedation- and/or procedure-related complications.
Materials and Methods
A total of 180 patients who underwent the ESD procedure for gastric adenoma or early gastric cancer were randomized to two groups. The control group (n=90) was monitored by the Modified Observer's Assessment of Alertness and Sedation scale and the BIS group (n=90) was monitored using BIS. The total doses of propofol and remifentanil, the need for rescue propofol, and the rates of complications were recorded.
Therapeutic endoscopic procedures requiring sedation of the patient have become popular worldwide. Endoscopic submucosal dissection (ESD) is a new and minimally invasive method for the resection of early gastric cancers and gastric adenomas that allows for en-bloc resection and an accurate histological evaluation.1,2 However, ESD is a technically difficult procedure requiring a longer procedure time than conventional endoscopic mucosal resection.3 Moreover, patients experience discomfort and pain caused by rotation of the scope, overextension of the gastric wall, and the ripple effect of direct heat coagulation of the muscularis.4 Although general anesthesia is rarely considered in difficult cases requiring a high level of technical expertise,4 sedation for ESD is usually carried out as a safe and cost-effective method. Therefore, the optimal depth of sedation is important not only to improve facility efficiency and patient cooperation, but also to avoid procedure-related complications such as perforation caused by sudden body movements.4,5,6
Sedation for ESD using propofol has been shown to provide better sedation effectiveness, safety, and improved recovery profile, compared to midazolam.7,8,9 Additionally, the combined use of analgesics is recommended for ESD to relieve pain. Adding opioids has been reported to improve the quality of sedation and reduce the propofol dosage and interventions required during the endoscopic procedures.4,10,11 However, due to the narrow therapeutic range and the synergistic effect of the drugs, especially in complex and prolonged endoscopic procedures, the combined use of propofol and opioids may lead to oversedation, resulting in a high risk of cardiopulmonary complications.10,12 Therefore, the precise monitoring of the level of sedation is warranted in order to minimize the risks of cardiopulmonary compromise during the moderate-to-deep sedation required for ESD procedures.4
The bispectral index (BIS) monitor is a non-invasive tool that objectively evaluates the depth of sedation, and can be contrasted with conventional observational assessments during therapeutic endoscopic procedures that are based on somatic responses.8,13,14,15,16,17 BIS monitoring of moderate-to-deep sedation using propofol during ESD procedures was associated with a high satisfaction level of patients and endoscopists.14 In patients undergoing endoscopic retrograde cholangiopancreatography (ERCP), BIS monitoring of propofol-induced deep sedation has been reported to reduce the mean propofol dose and recovery times.16,17 However, studies evaluating the clinical usefulness of BIS monitoring for gastrointestinal endoscopy have shown inconsistent results with regards to the dose of sedatives, satisfaction scores, and the risk of complications.14,15,16,17,18,19 Furthermore, the evidence is limited regarding the effects of BIS monitoring on the clinical benefit of the stable maintenance of optimal sedation during ESD procedures using propofol infusion with opioids. Therefore, in this prospective randomized controlled trial, we evaluated whether BIS monitoring for target sedation using continuous propofol infusion along with remifentanil could reduce the number of patients requiring rescue propofol, as well as the incidence of sedation- and/or procedure-related complications.
The study received Institutional Review Board approval (ref. 4-2011-0347) and was registered at http://clinicaltrials.gov (registration number NCT01921283). After obtaining written informed consent from each patient, we studied 180 patients who were scheduled for elective ESD. The inclusion criteria were adult patients aged 20-80 with American Society of Anesthesiologists classifications of 1-3. The exclusion criteria were as follows: a body mass index (BMI) >35 kg/m2, severe hepatic (liver transaminase >100 IU/L) or renal (serum creatinine level >2 mg/dL) insufficiency, mental incompetence, a history of allergy to the study drugs, use of antidepressants or anticonvulsants, unstable angina, symptomatic congestive heart failure, symptomatic chronic obstructive pulmonary disease, baseline oxygen saturation <90% on room air, and baseline systolic blood pressure <80 mm Hg.
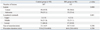
Patients were randomly assigned to either the control group (n=90) or the BIS group (n=90) by the opening of a sealed allocation envelope. Our goal of sedation was to achieve sedation between moderate (patient responds properly to verbal or light tactile stimulation) and deep (patient respond to painful stimuli; airway support may be required) levels.4 All sedation was managed by an anesthesiologist who had more than four years of general anesthesia experience before study enrollment. The target level of sedation was monitored by the Modified Observer's Assessment of Alertness and Sedation (MOAA/S) scale (Table 1) in the control group and using BIS values in the BIS group. In the control group, our target level of sedation corresponds to a score of 1-2 on the MOAA/S (i.e., patient responds only after squeezing the trapezius; responds only after mild prodding or shaking), which was routinely evaluated at 1 minute after propofol administration, just before endoscopy insertion, submucosal inflation by epinephrine (1:100000) and submucosal dissection, and when patients did not cooperate. In the BIS group, the sedation level was assessed based on a BIS score of 68-75.20 All patients were given supplemental oxygen of 2 L/min by a nasal cannula throughout the procedure.
All patients were continuously monitored for heart rate (HR), peripheral oxygen saturation (SpO2), and electrocardiographic changes. Blood pressure (BP) was assessed automatically at 5-minute intervals and all vital signs were recorded at 5-minute intervals. In all patients, a single use, disposable, low impedance BIS sensor consisting of four electrodes was attached to the middle and right forehead. However, only patients allocated in the BIS group were monitored by Bispectral Index (BIS VISTA Monitoring System; Aspect Medical Systems Inc., Norwood, MA, USA), which was placed behind endoscopists. Endoscopists and patients were blinded to the assigned group throughout the study. All procedures were performed with a standard single channel endoscope in the left lateral decubitus position. The procedure involved marking, mucosal incision, and submucosal dissection with simultaneous hemostasis.
All patients were premedicated with butylscopolamine (Buscopan®; Handok Pharm. Co., Cheongju, Korea) and received propofol and remifentanil using total body weight for sedation and analgesia. Sedation was initiated with 0.8 mg/kg of propofol and 30 mg of lidocaine; thereafter, 3 mg/kg/hr of propofol and 3 µg/kg/hr of remifentanil were started using an infusion pump and maintenance doses of propofol were titrated by 0.5 mg/kg/hr in a stepwise manner according to the target level of sedation; to simulate the current situation in Korea, a target-controlled infusion system was not used. In patients with BMI >25 kg/m2, sedation doses were calculated based on body weight for a BMI of 25. If procedural interference occurred, 0.4 mg/kg of propofol (rescue propofol) could be given as a bolus by the attending anesthesiologist in either group. Procedural interference was defined as a temporary pause in the procedure or need to physically restrain the patients due to sudden body movements or insufficient cooperation. Propofol and remifentanil infusion were continued until the removal of the endoscope.
After the procedure, patients were transferred to the endoscopy unit recovery room for post-procedure monitoring. An Aldrete recovery scoring system was used to determine the appropriateness (a score of 8 out of 10) for discharge from the recovery room judged by the postanesthesia care unit nursing staff who were not involved in the study. Satisfaction among the physicians and patients with the sedation and the procedure was recorded using an 11-point scale (0-10) after the end of the procedure and before discharge from the endoscopy unit recovery room, respectively. All patients also completed a questionnaire about pain and/or discomfort using a visual analog scale (VAS), ranging from 0 mm (no pain) to 100 mm (worst pain imaginable) (Fig. 1), and recall of the procedure before discharge from the endoscopy unit recovery room.
Cardiopulmonary events such as bradycardia (HR <45 beats/min), hypotension (systolic BP <80 mm Hg), and desaturation (SpO2 <90% of any duration) were recorded during the ESD procedure and recovery room care. When an adverse event occurred, the following measures were undertaken: atropine 0.01 mg/kg IV for bradycardia, the reduction of the maintenance dose of propofol and 0.9% saline 300 mL loading with/without 4 mg of ephedrine for hypotension. If desaturation <90% developed, supplemental oxygen flow was increased until the saturation reached 95%. If desaturation <90% continued despite increased supplemental oxygen flow, the procedure and sedation were interrupted to secure the airway. Complications including gastric bleeding, perforation, and aspiration pneumonia were observed during the hospital stay. Incidents of bleeding, defined as intra- and post-procedural bleeding requiring packed red blood cell transfusion or endoscopic intervention, perforation showing direct endoscopic observation of mesenteric fat or free air on an abdominal radiograph or computed tomography scan, and aspiration pneumonia showing pneumonic consolidation on chest radiograph were recorded until the patient's discharge from the hospital.
All data are expressed as means±standard deviations, numbers (percentages), or medians (upper and lower quartiles), as appropriate. Data between the groups were compared using the χ2 test, Fisher exact test, independent t-test, or the Mann-Whitney U test, as appropriate. To assess data normality, the Kolmogorov-Smirnov test was performed on the data set. In the preliminary trial of 36 patients, the number of patients requiring rescue propofol was 9 and 5 in the control group and the BIS group, respectively. We accepted that a 50% reduction in the proportion of patients with rescue propofol intervention represented a clinically significant benefit. According to a preliminary study, 85 patients would be required in each group with a power of 0.9 and a type I error of 0.05. Factoring in a drop-out rate of -5%, we calculated that 90 patients would be required for each group. All statistical analyses were performed with the SPSS 18.0 (SPSS Inc., Chicago, IL, USA) program. A p value <0.05 was considered statistically significant.
This study included a total of 220 lesions in 180 patients who underwent the ESD procedure for gastric adenoma or early gastric cancer from May 2011 to February 2012. The baseline characteristics were similar between the groups (Table 2). The mean age was 62.5 years and the age range was 38-80 years.
There were no significant differences in the time from the end of endoscopy until eye opening, the time from endoscopy until leaving the recovery room, the total dose and mean maintenance rate of propofol, and the total dose of remifentanil between the two groups (Table 3). The number of patients who needed rescue propofol during the procedure was significantly higher in the control group than the BIS group (47.8% vs. 30%). The frequency of sudden body movements did not differ between the control group and the BIS group (31.1% vs. 22.2%). There were no significant differences in the satisfaction scores of the physicians and patients between the two groups. There were 54 (60%) patients in the control group and 58 (64.4%) patients in the BIS group who experienced discomfort after awakening in the endoscopy unit recovery room; their VAS scores were 29±17 and 27±12 in the control and BIS group, respectively. There were no differences in the locations of the lesions and the resection sizes (Table 4). Hemodynamic variables including HR and mean BP did not differ between the two groups (Fig. 2).
There was no significant difference between the two groups with regard to the incidence of complications and recall of the procedure (Table 5). Overall cardiopulmonary events during sedation and recovery room care were observed in 22 patients (24%) in the control group and in 22 patients (24%) in the BIS group (p=1.00). Oxygen desaturation and hypotension during sedation occurred in 14 patients (8%) and 27 patients (15%), respectively. Patients who experienced desaturation more than 60 seconds were one in the control group and three in the BIS group (p=0.621). There was no case of desaturation needing intubation or ventilation. There was also no case of sustained hypotension after propofol titration and saline loading in either group. The overall complications, including perforation, gastric bleeding, and aspiration pneumonia, were observed in 13 patients (14%) in the control group and in 7 patients (8%) in the BIS group (p=0.16). Perforation related to ESD occurred in 3% of patients after ESD; all perforations were managed with fasting and observation. Only one patient experienced both perforation and gastric bleeding. None of these patients underwent additional surgery due to perforation and gastric bleeding. There was no ESD-related mortality throughout the study period.
In this prospective randomized controlled trial to investigate the efficacy of BIS as a monitor of sedation in ESD, we found that BIS monitoring as the primary target for sedation using a combination of propofol and remifentanil led to a reduction in the number of patients requiring rescue propofol. However, this finding, suggesting more stable maintenance within the range of the target depth of sedation by BIS monitoring than by MOAA/S, was not associated with clinical benefits in terms of the incidence of sedation- and/or procedure-related complications and the total dose of propofol administered.
During ESD procedures, the stable maintenance of optimal levels of sedation is mandatory to minimize the risk of perforation and other procedure-related complications caused by uncontrolled body movement.4 Recently, propofol-induced moderate-to-deep sedation for ESD has been reported to be as safe and effective as benzodiazepine with better recovery profiles.7,8,9 Adding analgesics is also recommended for ESD to relieve pain and to improve the quality of sedation.4,10,11,21 Combined continuous propofol infusion and opioid administration has been reported to improve ESD performance, with benefits such as en bloc resection and complete resection, compared to intermittent midazolam/propofol injection methods.21 However, considering that sedation level is a continuum, the moderate-to-deep or deep sedation required for ESD procedures may increase the patient's risk of complications caused by excessive sedation, as deep sedation is highly associated with inadequate ventilation or airway obstruction.4,7,8,9,14 Additionally, continuous propofol infusion with opioids for moderate-to-deep sedation, lengthy procedure times >2 hr, the male gender, and age >75 years have been reported to be independent risk factors for pneumonia after ESD.22 According to the guidelines for sedation and/or analgesia by non-anesthesiologists, the accurate titration of drugs and close communication between the patient and the physician are recommended to achieve a high quality of mild-to-moderate sedation for diagnostic or therapeutic procedures.23,24 However, in cases requiring more than moderate depths of sedation for ESD, monitoring mainly relies on the direct observation of the patients' behaviors or responses to voice and physical stimuli through the MOAA/S. Therefore, the use of BIS for quantifying the effects of hypnotic drugs has been studied for the continuous monitoring of propofol sedation for therapeutic endoscopic procedures.14,16,17 However, studies evaluating the efficacy of BIS monitoring for propofol sedation in gastrointestinal endoscopy have shown inconsistent results.14,16,17,18,19 While BIS is clinically used as a measure of the depth of sedation, the BIS algorithm actually reflects the brain's response to both the effects of the hypnotic drugs and noxious stimuli. Thus, proper interpretation of BIS needs to consider the drugs used, the administration methods of the drugs, and levels of noxious stimuli.25,26
To our knowledge, this is the first study to investigate the efficacy of BIS monitoring during anesthesiologist-directed propofol and remifentanil sedation for ESD procedures. In the current study, BIS monitoring as the primary target for sedation by the continuous infusion of both propofol and remifentanil reduced the number of patients requiring rescue propofol. Rescue propofol was administered for patient safety as a bolus injection in cases of procedural interference due to sudden body movement or insufficient patient cooperation by the attending anesthesiologist. Our results suggest that BIS monitoring was more nimble than MOAA/S monitoring in titrating the maintenance rate of propofol according to the response to different noxious stimuli, but was not related to reduction in procedure-related complications such as bleeding and perforation. In previous endoscopic studies regarding BIS monitoring of propofol sedation, BIS monitoring has shown clinical benefits such as improved satisfaction levels of patients and physicians after ESD,14 reduced mean propofol dose in ERCP,17 and shorter recovery times after ERCP.16 Although the clinical efficacy of BIS monitoring in decreasing rescue propofol did not lead to a reduction in total dose of propofol, studies from other groups have demonstrated no advantage for BIS monitoring in terms of propofol dose.14,16 Direct comparison of our results with previous studies is rather difficult because of differences in types of procedures, physicians managing propofol, and various target levels of sedation, such as moderate-to-deep sedation (MOAA/S scores 2-3 or BIS value 76-85)14 and deep sedation (BIS values >55 or <55 were permitted),16 and deep sedation (MOAA/S scores 0 or BIS value 40-60).17 For propofol sedation in gastrointestinal endoscopy, propofol should be administered by an anesthesiologist,17 or endoscopists or nursing staff14,16 who receive special training in sedation and resuscitation techniques for safety of patients in most countries. In the current study, the experienced anesthesiologists might have more quickly recognized restless movements in patients and thus influence the results so that the satisfaction scores of both patients and physicians did not differ between the two groups. In contrast to studies where propofol was administered by repeated bolus injection,16,18 we used continuous infusion method for a steady plasma level and consequently maintained a stable target depth of sedation, which may result in rapid recovery in both groups.
As well, we chose to use remifentanil in combination with propofol to improve the quality of sedation and thus ESD performance through the attenuation of responses to noxious stimuli.10,21,27 The analgesic properties of propofol for countering acute pain remain controversial and thus remifentanil, with its fast onset and short duration, may be a suitable analgesic adjunct in ESD patients. Adding remifentanil reduces the needed concentration of propofol to ablate responses to noxious stimuli because the interaction between propofol and remifentanil is synergistic. In the current study, adding remifentanil partially blocked the response to pain and thus might contribute to the prevention of procedure-related complications in either group. In consideration of the pharmacodynamic interaction between propofol and remifentanil in hypnosis and BIS, it was found that while propofol was equipotent in its effect on BIS with/without remifentanil, remifentanil had little direct effect on BIS but influenced BIS through the potentiation of the hypnotic effect of propofol.25 Regardless of the addition of remifentanil, BIS has been reported to be reliable for assessing the patient's level on the Observer's Assessment of Alertness/Sedation Scale.28
This study has several limitations. First, the attending anesthesiologist was not blind to the use of BIS monitoring during ESD, a condition that was not possible in our study design. Second, we did not plan to evaluate the time lag between the signal collection and BIS display, which varies depending on the smoothing and processing of the artifact-free signal.29 However, this time lag in the BIS group would not have a large effect on the results because the attending anesthesiologist recognized the changing trend of the BIS values and maintained the patient's anesthesia within the target values of BIS. Third, although the sample size was calculated to validate the proportion of patients requiring rescue propofol, the power to assess the incidence of sedation- and/or procedure-related complications was not sufficient. Finally, we administered propofol and remifentanil using an infusion pump according to the patient's weight. However, these drugs should optimally be administered using target-controlled infusion systems considering several factors affecting the pharmacokinetics-pharmacodynamics of propofol and remifentanil, such as the age, weight, height, and underlying disease, especially in lengthy procedures.30 Therefore, further study is needed to evaluate the efficacy of BIS monitoring considering these limitations.
In conclusion, BIS-guided propofol infusion combined with remifentanil reduced the number of patients requiring rescue propofol in ESD procedures. However, this finding did not lead to a reduction in the total dose of propofol or the rate of complications, and thus, BIS monitoring is of limited use in the guidance of sedation in the setting of continuous propofol infusion with remifentanil managed by an anesthesiologist.
Figures and Tables
 | Fig. 2Hemodynamic data including heart rate (A) and mean blood pressure (B) during the procedures. Data are expressed as mean±SD. No differences between the groups. BIS, bispectral index. |
References
1. Imagawa A, Okada H, Kawahara Y, Takenaka R, Kato J, Kawamoto H, et al. Endoscopic submucosal dissection for early gastric cancer: results and degrees of technical difficulty as well as success. Endoscopy. 2006; 38:987–990.

2. Sugimoto T, Okamoto M, Mitsuno Y, Kondo S, Ogura K, Ohmae T, et al. Endoscopic submucosal dissection is an effective and safe therapy for early gastric neoplasms: a multicenter feasible study. J Clin Gastroenterol. 2012; 46:124–129.

3. Oda I, Gotoda T, Hamanaka H, Eguchi T, Saito Y, Matsuda T, et al. Endoscopic submucosal dissection for early gastric cancer: technical feasibility, operation time and complications from a large consecutive series. Dig Endosc. 2005; 17:54–58.

4. Sasaki T, Tanabe S, Ishido K, Azuma M, Katada C, Higuchi K, et al. Recommended sedation and intraprocedural monitoring for gastric endoscopic submucosal dissection. Dig Endosc. 2013; 25:Suppl 1. 79–85.

5. Lee CK, Lee SH, Chung IK, Lee TH, Park SH, Kim EO, et al. Balanced propofol sedation for therapeutic GI endoscopic procedures: a prospective, randomized study. Gastrointest Endosc. 2011; 73:206–214.

6. Shah B, Cohen LB. The changing faces of endoscopic sedation. Expert Rev Gastroenterol Hepatol. 2010; 4:417–422.

7. Kiriyama S, Gotoda T, Sano H, Oda I, Nishimoto F, Hirashima T, et al. Safe and effective sedation in endoscopic submucosal dissection for early gastric cancer: a randomized comparison between propofol continuous infusion and intermittent midazolam injection. J Gastroenterol. 2010; 45:831–837.

8. Sasaki T, Tanabe S, Azuma M, Sato A, Naruke A, Ishido K, et al. Propofol sedation with bispectral index monitoring is useful for endoscopic submucosal dissection: a randomized prospective phase II clinical trial. Endoscopy. 2012; 44:584–589.

9. Yamagata T, Hirasawa D, Fujita N, Suzuki T, Obana T, Sugawara T, et al. Efficacy of propofol sedation for endoscopic submucosal dissection (ESD): assessment with prospective data collection. Intern Med. 2011; 50:1455–1460.

10. Mazanikov M, Udd M, Kylänpää L, Lindström O, Aho P, Halttunen J, et al. Patient-controlled sedation with propofol and remifentanil for ERCP: a randomized, controlled study. Gastrointest Endosc. 2011; 73:260–266.

11. Hsieh YH, Chou AL, Lai YY, Chen BS, Sia SL, Chen IC, et al. Propofol alone versus propofol in combination with meperidine for sedation during colonoscopy. J Clin Gastroenterol. 2009; 43:753–757.

12. Kulling D, Fantin AC, Biro P, Bauerfeind P, Fried M. Safer colonoscopy with patient-controlled analgesia and sedation with propofol and alfentanil. Gastrointest Endosc. 2001; 54:1–7.

13. Bell JK, Laasch HU, Wilbraham L, England RE, Morris JA, Martin DF. Bispectral index monitoring for conscious sedation in intervention: better, safer, faster. Clin Radiol. 2004; 59:1106–1113.

14. Imagawa A, Fujiki S, Kawahara Y, Matsushita H, Ota S, Tomoda T, et al. Satisfaction with bispectral index monitoring of propofol-mediated sedation during endoscopic submucosal dissection: a prospective, randomized study. Endoscopy. 2008; 40:905–909.

15. Kang KJ, Min BH, Lee MJ, Lim HS, Kim JY, Lee JH, et al. Efficacy of Bispectral Index Monitoring for Midazolam and Meperidine Induced Sedation during Endoscopic Submucosal Dissection: A Prospective, Randomized Controlled Study. Gut Liver. 2011; 5:160–164.

16. von Delius S, Salletmaier H, Meining A, Wagenpfeil S, Saur D, Bajbouj M, et al. Bispectral index monitoring of midazolam and propofol sedation during endoscopic retrograde cholangiopancreatography: a randomized clinical trial (the EndoBIS study). Endoscopy. 2012; 44:258–264.

17. Paspatis GA, Chainaki I, Manolaraki MM, Vardas E, Theodoropoulou A, Tribonias G, et al. Efficacy of bispectral index monitoring as an adjunct to propofol deep sedation for ERCP: a randomized controlled trial. Endoscopy. 2009; 41:1046–1051.

18. Drake LM, Chen SC, Rex DK. Efficacy of bispectral monitoring as an adjunct to nurse-administered propofol sedation for colonoscopy: a randomized controlled trial. Am J Gastroenterol. 2006; 101:2003–2007.

19. von Delius S, Thies P, Rieder T, Wagenpfeil S, Herberich E, Karagianni A, et al. Auditory evoked potentials compared with bispectral index for monitoring of midazolam and propofol sedation during colonoscopy. Am J Gastroenterol. 2009; 104:318–325.

20. Johansen JW. Update on bispectral index monitoring. Best Pract Res Clin Anaesthesiol. 2006; 20:81–99.

21. Park CH, Min JH, Yoo YC, Kim H, Joh DH, Jo JH, et al. Sedation methods can determine performance of endoscopic submucosal dissection in patients with gastric neoplasia. Surg Endosc. 2013; 27:2760–2767.

22. Park CH, Kim H, Kang YA, Cho IR, Kim B, Heo SJ, et al. Risk factors and prognosis of pulmonary complications after endoscopic submucosal dissection for gastric neoplasia. Dig Dis Sci. 2013; 58:540–546.

23. Knape JT, Adriaensen H, van Aken H, Blunnie WP, Carlsson C, Dupont M, et al. Guidelines for sedation and/or analgesia by non-anaesthesiology doctors. Eur J Anaesthesiol. 2007; 24:563–567.

24. American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-Anesthesiologists. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002; 96:1004–1017.
25. Bouillon TW, Bruhn J, Radulescu L, Andresen C, Shafer TJ, Cohane C, et al. Pharmacodynamic interaction between propofol and remifentanil regarding hypnosis, tolerance of laryngoscopy, bispectral index, and electroencephalographic approximate entropy. Anesthesiology. 2004; 100:1353–1372.

26. Dahaba AA. Different conditions that could result in the bispectral index indicating an incorrect hypnotic state. Anesth Analg. 2005; 101:765–773.

27. Bürkle H, Dunbar S, Van Aken H. Remifentanil: a novel, short-acting, mu-opioid. Anesth Analg. 1996; 83:646–651.
28. Struys MM, Vereecke H, Moerman A, Jensen EW, Verhaeghen D, De Neve N, et al. Ability of the bispectral index, autoregressive modelling with exogenous input-derived auditory evoked potentials, and predicted propofol concentrations to measure patient responsiveness during anesthesia with propofol and remifentanil. Anesthesiology. 2003; 99:802–812.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download