Abstract
Purpose
Presence of a cephalomedullary nail (CMN) in the medullary canal has been thought as advantageous in the control of femoral neck shortening (FNS) and lag screw sliding in trochanteric fracture compared to extramedullary fixation system. However, researches on the factors that influence the degree of FNS after cephalomedullary nailing are lacking.
Materials and Methods
We observed 95 patients (mean age, 75±2.8 years) with trochanteric fractures who were treated with a CMN, and evaluated the relationship between FNS and patient factors including age, gender, fracture type (AO/OTA), bone mineral density, medullary canal diameter, canal occupancy ratio (COR=nail size/canal diameter), and tip-apex distance using initial, immediate postoperative, and follow-up radiography.
Results
Univariate regression analyses revealed that the degree of FNS was significantly correlated with fracture type (A1 versus A3, p<0.001), medullary canal diameter (p<0.001), and COR (p<0.001). Multiple regression analyses revealed that FNS was strongly correlated with fracture type (p<0.001) and COR (p<0.001).
Introduction of a sliding hip screw (SHS) and cephalomedullary nail (CMN) dramatically reduces the incidence of fixation failure in trochanteric fractures.1 Lag screw sliding allows impaction at the fracture site and enhanced stability, enabling early mobilization. Unfortunately, however, excessive sliding of the proximal fragments sometimes occurs in both CMN and SHS systems causing thigh pain and femoral neck shortening (FNS). Excessive sliding has also been thought as one of important causes of fixation failure such as cut out of the femoral head by a lag screw.2,3 Preservation of hip axis length after fracture treatment is an important factor in functional recovery after bone union in patients with hip fractures.4 In femoral neck fractures, neck shortening has been shown to correlate with functional deterioration after bone union.5,6,7
Cephalomedullary nailing became more popular in treating unstable trochanteric fractures in these days.8,9 Presence of a CMN in the medullary canal has been thought as advantageous in the control of lag screw sliding and FNS compared to extramedullary fixation system in trochanteric fracture. However, researches on the factors that influence the degree of FNS after cephalomedullary nailing are lacking. In this study, we analyzed the factors that influence lag screw sliding distance and FNS in patients who underwent cephalomedullary nailing after sustaining trochanteric fractures.
From January 2006 to December 2010, 565 patients sustained trochanteric fractures (AO/OTA classification 31-A1 to A3) and were treated at two institutions with ITST nails (ITST™, Zimmer®, Warsaw, IN, USA). We selected 116 patients between the ages of 70 and 80 years old to minimize the age related factors such as medullary canal diameter and bone mineral density (BMD). Of these patients, 95 were followed for more than 1 year after surgery or revision surgery.
Surgery was performed with the patient in the supine position on the fracture table under general or spinal anesthesia. When possible, we aligned the medial cortices of fractured fragments in the antero-posterior image and the anterior cortices in the axial radiological image before the incision. When closed reduction failed, a long hemostatic forceps or pointed bone forceps was used to hold the fragments in reduced position after incision. A nail entry site was created on the medial edge of the tip of the greater trochanter. A CMN was inserted into the reamed medullary canal after trochanteric reaming. The diameter of the CMN was determined during preoperative planning according to the diameter of the medullary canal. Specifically, we measured the inner diameter of the proximal femur 2 cm below the distal border of the lesser trochanter in the Picture Archiving and Communication System (PACS) using a magnification bar. We used a nail 1 mm smaller than the measured value. In patients whose medullary canal diameter was over 13 mm, we used a 12-mm diameter CMN, the largest available nail in hospitals. If the medullary canal was too narrow to accept a 10-mm nail (the smallest available nail in the hospitals), we reamed the proximal femur with the medullary reamer, up to 11 mm. Reaming of the proximal femur was performed only if it was necessary to accept the nail. The end of the lag screw was positioned at the center of the femoral head in the antero-posterior and axial images. Distal locking was performed with one or two screws. Rehabilitation started at the first postoperative day. Sitting and continuous passive motion of the knee and hip joints were allowed. The majority of patients were encouraged to partially bear their weight within 1 week after surgery with walking aids depending on the patient's condition.
Fracture subgrouping was performed using AO/OTA classification. BMD was measured on the normal side of the hip joint using dual-energy X-ray absorptiometry (DXA; Discovery™, Hologic®, MA, USA) in 79 patients (83.2%) after surgery. Femoral neck T-scores were selected to represent patient BMD. The clinical absence of pain, presence of a callus shadow that passed through the fracture line in three cortices, and closure of the fracture line were used to determine bone union. Radiological measurements were analyzed using the PACS.
Standard anteroposterior (AP) radiographs of the hip were obtained with both legs positioned to an internal rotation of 15°. Lateral radiographs were taken with the opposite hip flexed and abducted. The canal occupancy ratio (COR) was calculated by dividing the CMN size by the femoral canal diameter. FNS after union was measured using the method described by Weil, et al.,7 at the time of the final follow-up exam. Briefly, the contralateral femur was overlaid on the shortened femur in the final AP radiogram. FNS was calculated using vectorial addition of changes in the x-axis (shortening in the abductor arm) and in the y-axis (shortening in the vertical plane). The sliding distance of the lag screw was measured from the antero-posterior radiological images taken immediately after surgery and at the time of the final follow-up examination, using the method of Watanabe, et al. 10 The tip-apex distance (TAD) was measured from the postoperative radiographs. The reduction was categorized as good, acceptable, or poor using the method of Baumgaertner, et al.11
We used SAS version 9.1 (SAS Institute Inc., Cary, NC, USA) for statistical analyses. Univariate and multiple regression analyses were performed to assess the individual patient effects on FNS. A stepwise multiple linear regression analysis was performed with backward elimination to select an appropriate model. A p-value greater than 0.10 was used for removal. A p-value by two tailed test less than 0.05 was considered significant for all analyses.
The average period of follow-up was 15 months (range, 12 to 44 months). Among the 95 patients, 11 were male and 84 were female. The average age was 75.1 years old (range, 70 to 80 years of age). Regarding the reduction,11 49 fractures (51.6%) were judged to be good, 43 fractures (45.3%) acceptable, and 3 fractures (3.2%) were poor. Bone union was observed within 14.5 weeks on average (range, 12 to 19 weeks). Fixation failure occurred in 3 patients. These included a femoral head fracture caused by a lag screw after a second fall (31-A2.1; lag screw sliding, 15.6 mm), cut-out of a lag screw after varus collapse (31-A1.2; lag screw sliding, 3.3 mm), and a superior migration of a lag screw (31-A2.2; lag screw sliding, 4.8 mm).
The diameter of the femoral medullary canal measured 2 cm distal to the lesser trochanter was 13.4 mm on average (range, 10.2 to 21.6 mm). The average hip T-score of the intact femur was -2.7 (range: -0.8 to -4.9). The average TAD was 16.9 mm (range, 9.6 to 20.2 mm). The average COR was 0.87 (range, 0.56 to 0.99). According to the AO/OTA fracture classification, there were 37 cases of A1, 55 cases of A2, and 3 cases of A3.
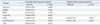
The mean sliding distance was 3.11 mm (range, 0.50 to 16.80 mm); 2.55 mm (range, 0.5 to 8.1 mm) in A1, 3.02 (range, 0.7 to 12.1 mm) in A2, and 11.67 mm (range 8.4 to 16.8 mm) in A3. A3 type fractures demonstrated more screw sliding than A1 or A2 type fractures (p=0.004, p=0.006). Univariate regression analysis was performed to test the association of sliding distance to gender, age at the time of surgery, BMD, medullary canal diameter, COR, TAD, and AO/OTA classification. AO/OTA type (A1 versus A3; R2=0.6241, β=9.121, p<0.001), medullary canal diameter (R2=0.174, β=0.412, p<0.001), and COR (R2= 0.104, β=2.046, p=0.004) were significantly correlated with lag screw sliding distance. Multiple regression analyses (R2= 0.522) illustrated that COR (β=-9.410, p<0.001) and AO/OTA type (A1 versus A3; β=7.803, p<0.001) were more strongly correlated (Table 1).
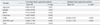
The mean FNS was 4.49 mm (range, 1.7 to 17.8 mm); 3.90 (range, 1.90 to 9.50 mm) in A1, 4.41 mm (range, 1.70 to 13.50 mm) in A2, and 13.27 mm (range, 10.20 to 17.80 mm) in A3. Univariate regression analysis was performed to test the association of FNS to gender, age at the time of surgery, BMD, medullary canal diameter, COR, TAD, and AO/OTA classification. AO/OTA type (A1 versus A3; R2=0.340, β=9.064, p<0.001), medullary canal diameter (R2=0.207, β=0.447, p<0.001), and COR (R2= 0.212, β= -11.052, p<0.001) (Fig. 1) were significantly correlated with FNS. Multiple regression analyses (R2= 0.523) illustrated that COR (β=-8.918, p<0.001) and AO/OTA type (A1 versus A3; β=8.113, p<0.001) were more strongly correlated (Table 2).
Controlled lag screw sliding and fracture site impaction are fundamental concepts in treating intertrochanteric fractures as well as femoral neck fracture. However, excessive sliding of lag screw and resultant short femoral neck sometimes ends up with unfavorable functional recovery. In this study, we identified that lag screw sliding distance and FNS were determined by many uncontrollable factors by the surgeons and the presence of CMN alone couldn't effectively control them, especially in low COR and 31-A3 type fractures. The sliding distance in the SHS system depends on many factors including inclination angle of the lag screw,12 fracture type,13 reduction status,11 and bone quality.14 The CMN system theoretically has been regarded as having several advantages over SHS system such as a shorter lever arm, the ability to more efficiently deliver weight through the calcar femorale, and nail placement inside the medullary canal that abuts the neck fragment.15 However, studies assessing the sliding distance and final FNS after CMN are limited. We reviewed 11 randomized clinical trials comparing SHSs and CMNs in trochanteric fractures.16,17,18,19,20,21,22,23,24,25,26,27 There were little mention regarding the differences in lag screw sliding between two systems and only one study by Hardy, et al.,21 showed a statistically significant decrease in sliding of the lag screw with CMN compared to SHS.
Excessive sliding, FNS and thigh pain due to protrusion of the lag screw also occurs in the CMN system and are an unsolved problem. We showed herein, with univariate linear regression, that the diameter of the medullary canals, COR, and AO/OTA type were significantly correlated with FNS. The sliding distance of the lag screw revealed similar results as FNS. The increase in medullary canal diameter is closely related to aging. In a preliminary study (unpublished data), we analyzed lag screw sliding distance in 119 patients who were implanted and fixed with a 12 mm CMN which was the largest nail available in the hospital. We recognized that aging was well correlated with canal diameter and COR were prominent factors in lag screw sliding. For this reason, we selected patients aged 70- to 80-years-old to minimize the effects of aging. It is very importance due to following reasons. First, if the canal diameter is large, a relatively smaller nail may not be able to effectively support the proximal fragment because of toggling motion at the fracture site during gait cycle. Second, ageing causes an increase in canal diameter and a decrease in cortical thickness of the proximal femur.28 Third, it is unrealistic to manufacture and supply a full-set of nails (length and size) due to cost effectiveness.
A limitation to the study is the retrospective design. Three of the most difficult factors to control are aging, surgical skill of the surgeons and correct measurement of FNS and sliding distance of the lag screw due to rotation. To minimize the effect of aging, we limited the patient age to 70-80 years old in this study. The two institutes which collected the patient data in this study were referral hospitals. Only a single orthopedic surgeon who experienced CM nailing for more than 200 cases in each hospital was designated and performed the operations to minimize the technical errors. As a result, reduction status was acceptable at 96.9% or higher and TAD was well controlled under 20 mm in most of the case. The rate of fixation failure was low as 3.2% and decreased to 2.1% when we discarded the case of cut-out caused by a second fall during rehabilitation. Effect of limb rotation in calculating FNS was minimized by using the method described in the literatures.6,7
In conclusion, we analyzed 95 cases of CM nailing and confirmed that the presence of a CMN in the medullary canal alone could not effectively prevent FNS in patients with low COR and A3 type fracture. This study added important information in treating trochanteric fracture with a CMN. However, low fixation failure rate and insertion of 10 mm CM nail after reaming in patients with extremely narrow canal might have influenced our results. Therefore, further studies with prospective, large number of patients are needed to assess the factors affecting femoral neck shortening and lag screw sliding.
Figures and Tables
 | Fig. 1COR versus femoral neck shortening is shown on a scatterplot. The lower the ratio, the more shortening of the femoral neck. Black dots indicate cases of A3 type fractures. COR, canal occupancy ratio. |
References
1. Kyle RF, Cabanela ME, Russell TA, Swiontkowski MF, Winquist RA, Zuckerman JD, et al. Fractures of the proximal part of the femur. Instr Course Lect. 1995; 44:227–253.
2. Davis TR, Sher JL, Horsman A, Simpson M, Porter BB, Checketts RG. Intertrochanteric femoral fractures. Mechanical failure after internal fixation. J Bone Joint Surg Br. 1990; 72:26–31.

3. Gotfried Y. The lateral trochanteric wall: a key element in the reconstruction of unstable pertrochanteric hip fractures. Clin Orthop Relat Res. 2004; 82–86.
4. Zlowodzki M, Ayieni O, Petrisor BA, Bhandari M. Femoral neck shortening after fracture fixation with multiple cancellous screws: incidence and effect on function. J Trauma. 2008; 64:163–169.

5. Boraiah S, Paul O, Hammoud S, Gardner MJ, Helfet DL, Lorich DG. Predictable healing of femoral neck fractures treated with intraoperative compression and length-stable implants. J Trauma. 2010; 69:142–147.

6. Song HK, Lee JJ, Oh HC, Yang KH. Clinical implication of subgrouping in valgus femoral neck fractures: comparison of 31-B1.1 with 31-B1.2 fractures using the OTA/AO classification. J Orthop Trauma. 2013; 27:677–682.
7. Weil YA, Khoury A, Zuaiter I, Safran O, Liebergall M, Mosheiff R. Femoral neck shortening and varus collapse after navigated fixation of intracapsular femoral neck fractures. J Orthop Trauma. 2012; 26:19–23.

8. Anglen JO, Weinstein JN. American Board of Orthopaedic Surgery Research Committee. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Joint Surg Am. 2008; 90:700–707.

9. Lee YK, Yoon BH, Nho JH, Kim KC, Ha YC, Koo KH. National trends of surgical treatment for intertrochanteric fractures in Korea. J Korean Med Sci. 2013; 28:1407–1408.

10. Watanabe Y, Minami G, Takeshita H, Fujii T, Takai S, Hirasawa Y. Migration of the lag screw within the femoral head: a comparison of the intramedullary hip screw and the Gamma Asia-Pacific nail. J Orthop Trauma. 2002; 16:104–107.

11. Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995; 77:1058–1064.

12. Meislin RJ, Zuckerman JD, Kummer FJ, Frankel VH. A biomechanical analysis of the sliding hip screw: the question of plate angle. J Orthop Trauma. 1990; 4:130–136.
13. Steinberg GG, Desai SS, Kornwitz NA, Sullivan TJ. The intertrochanteric hip fracture. A retrospective analysis. Orthopedics. 1988; 11:265–273.

14. Barrios C, Broström LA, Stark A, Walheim G. Healing complications after internal fixation of trochanteric hip fractures: the prognostic value of osteoporosis. J Orthop Trauma. 1993; 7:438–442.

15. Hornby R, Evans JG, Vardon V. Operative or conservative treatment for trochanteric fractures of the femur. A randomised epidemiological trial in elderly patients. J Bone Joint Surg Br. 1989; 71:619–623.

16. Ahrengart L, Törnkvist H, Fornander P, Thorngren KG, Pasanen L, Wahlström P, et al. A randomized study of the compression hip screw and Gamma nail in 426 fractures. Clin Orthop Relat Res. 2002; 209–222.

17. Barton TM, Gleeson R, Topliss C, Greenwood R, Harries WJ, Chesser TJ. A comparison of the long gamma nail with the sliding hip screw for the treatment of AO/OTA 31-A2 fractures of the proximal part of the femur: a prospective randomized trial. J Bone Joint Surg Am. 2010; 92:792–798.

18. Baumgaertner MR, Curtin SL, Lindskog DM. Intramedullary versus extramedullary fixation for the treatment of intertrochanteric hip fractures. Clin Orthop Relat Res. 1998; 87–94.

19. Bridle SH, Patel AD, Bircher M, Calvert PT. Fixation of intertrochanteric fractures of the femur. A randomised prospective comparison of the gamma nail and the dynamic hip screw. J Bone Joint Surg Br. 1991; 73:330–334.

20. Crawford CH, Malkani AL, Cordray S, Roberts CS, Sligar W. The trochanteric nail versus the sliding hip screw for intertrochanteric hip fractures: a review of 93 cases. J Trauma. 2006; 60:325–328.

21. Hardy DC, Descamps PY, Krallis P, Fabeck L, Smets P, Bertens CL, et al. Use of an intramedullary hip-screw compared with a compression hip-screw with a plate for intertrochanteric femoral fractures. A prospective, randomized study of one hundred patients. J Bone Joint Surg Am. 1998; 80:618–630.

22. Hoffmann R, Schmidmaier G, Schulz R, Schütz M, Südkamp NP. [Classic nail versus DHS. A prospective randomised study of fixation of trochanteric femur fractures]. Unfallchirurg. 1999; 102:182–190.

23. Leung KS, So WS, Shen WY, Hui PW. Gamma nails and dynamic hip screws for peritrochanteric fractures. A randomised prospective study in elderly patients. J Bone Joint Surg Br. 1992; 74:345–351.

24. O'Brien PJ, Meek RN, Blachut PA, Broekhuyse HM, Sabharwal S. Fixation of intertrochanteric hip fractures: gamma nail versus dynamic hip screw. A randomized, prospective study. Can J Surg. 1995; 38:516–520.
25. Parker MJ, Handoll HH. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev. 2010; CD000093.

26. Radford PJ, Needoff M, Webb JK. A prospective randomised comparison of the dynamic hip screw and the gamma locking nail. J Bone Joint Surg Br. 1993; 75:789–793.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download