Abstract
Purpose
Comprehensive multidisciplinary weight management programs encompassing various conservative measures have shown only modest weight loss results in obese children and adolescents; therefore, bariatric surgery for this population has become a matter of discussion. This study aimed to present our experience with and outcomes for laparoscopic sleeve gastrectomy (LSG) and laparoscopic Roux-en-Y gastric bypass (LRYGB) in morbidly obese Korean adolescents.
Materials and Methods
The prospectively established database of all patients undergoing bariatric surgery at Soonchunhyang University Seoul Hospital, Korea between January 2011 and January 2013 was retrospectively reviewed. Adolescents aged 14 to 20 years were included in the present analyses.
Results
Twenty-two adolescents underwent bariatric surgery during the study period; 14 underwent LSG and 8, LRYGB. Of these, 17 were female and 5 were male. The mean age was 19 years. Their mean body weight and body mass index (BMI) before surgery were 115 kg and 40.1 kg/m2. The only postoperative complication was intraluminal bleeding in 1 patient, which was managed conservatively. The mean BMI decreased to 29.1 kg/m2 after a mean follow-up of 10 months. The percent excess weight loss (%EWL) at 1, 3, 6, and 12 months postoperatively were 19.6, 39.9, 52.6, and 74.2%, respectively. Only 1 patient showed %EWL less than 30% at 12 months after surgery. All patients with diabetes and sleep apnea were cured of their disease, and other comorbidities also improved or resolved after surgery.
Obesity has become one of the most important public health problems worldwide, in not only adults but also children and adolescents.1 Obesity in childhood is closely associated with several conditions including hypertension, dyslipidemia, and insulin resistance/glucose intolerance that comprise metabolic syndrome, a precursor to type 2 diabetes and cardiovascular diseases.2,3 The development of obesity in childhood and adolescence serves as a predictor of subsequent obesity in adulthood and carries an increased risk of adult morbidity and mortality.4,5 Childhood obesity has also been related to a variety of health problems such as obstructive sleep apnea, orthopedic problems, polycystic ovarian syndrome, and non-alcoholic fatty liver disease and to psychosocial problems that can have a marked influence on quality of life.
Although prevention is the long-term solution to this crucial health problem, efforts toward prevention are not always successful. Moreover, various conservative measures including lifestyle modification and medical treatment result in only modest weight reduction in the long term. Therefore, interest in bariatric surgery for morbidly obese adolescents has been increasing. Previous clinical trials demonstrated that bariatric surgery may be the most effective treatment available for sustained long-term weight loss and resolution of obesity-related illnesses in the adult population.6 However, it is still controversial whether this rather drastic approach can be safely used in children and adolescents. There is a considerable variation among the recommendations and guidelines for surgical approaches for the management of morbid obesity and obesity-related comorbidities. The long-term effectiveness of bariatric surgery in this young population remains questionable as well.
Here, we report our initial experience with bariatric surgery performed in morbidly obese adolescents in Korea. We analyzed surgical outcomes, including weight loss and comorbidity status, during short-term follow-up and aimed to evaluate the feasibility and efficacy of bariatric surgery in Korean adolescents.
The medical records of all consecutive adolescent patients 20 years old or younger who underwent bariatric surgery at Soonchunhyang University Seoul Hospital in Korea between January 2011 and January 2013 were retrospectively reviewed. Baseline, operative, and follow-up data from a prospectively established database were thoroughly reviewed and summarized.
Patients were selected according to the National Institutes of Health consensus guidelines for bariatric surgery. As such, adolescents with a body mass index (BMI) greater than 35 kg/m2 with serious obesity-related comorbidities (e.g., diabetes, sleep apnea, hypertension, or obesity related-arthropathy) or with a BMI of 40 kg/m2 or greater were considered for bariatric surgery. Patients and their parents received interdisciplinary education about potential surgical and nonsurgical options, possible outcomes, possible complications, and necessary postoperative lifestyle changes. All patients underwent comprehensive psychological and nutritional evaluations before surgery. Informed consent was obtained from parents with assent from the patient for those younger than 18 years of age or directly from patients for those older than 18 years of age.
All patients underwent either sleeve gastrectomy or Roux-en-Y gastric bypass. All the procedures were performed laparoscopically by a single experienced surgeon, who had performed more than 300 laparoscopic bariatric surgeries before the start of this series. The decision to perform laparoscopic sleeve gastrectomy (LSG) versus laparoscopic Roux-en-Y gastric bypass (LRYGB) was made on an individual basis by the surgeon, in discussion with the patient. All patients were counseled on the specific risks associated with each procedure. The possibility of developing nutritional deficiency following LRYGB was well discussed. Patients choosing LSG were informed of the risks of inadequate weight loss and the possibility that revisional surgery might be required.
LRYGB was performed via three 5-mm and two 12-mm ports. A small gastric pouch with approximately 30 mL volume was created along the lesser curvature by using laparoscopic linear staplers. A 40-cm biliopancreatic limb and a 100-cm alimentary limb were constructed. The Roux limb was positioned in an antecolic fashion. Gastrojejunostomy was constructed with the linear stapler and anastomotic leakage was assessed intraoperatively via air or methylene blue-stained saline injection into the gastric pouch. All mesenteric defects were closed with non-absorbable suture materials.
LSG was performed by using five trocar incisions and the otherwise standard technique that has been described previously.7 Gastric resection was performed with laparoscopic linear staplers, creating a staple line parallel to the lesser curvature of the stomach under 34-Fr bougie dilator guidance. The staple line was selectively reinforced with either the interrupted method or the continuous oversewing method, especially where bleeding persisted or staples were overlapped.
Patients initiated oral intake in the morning of the first postoperative day and were discharged once they had achieved adequate oral intake, their pain was under control, and they were ambulating without difficulty. The postoperative nutritional regimen consisted of a liquid or soft diet for the first 3 weeks, with gradual increases in food texture thereafter. Patients returned to the outpatient clinic 2 weeks after surgery, and then every 3 months for the first postoperative year to monitor weight loss, appetite, dysphagia or food intolerance, eating behavior, comorbidity status, and the presence of any complications. Follow-up was then decreased to every 12 months after the first year. Telephone interviews were also used to monitor patients who could not visit the outpatient clinic.
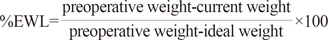
The degree of weight loss was assessed with percent excess weight loss (%EWL), which was calculated from the following formula:8
The diagnosis of type 2 diabetes was made according to the criteria established by the American Diabetes Association [fasting blood glucose (FBS) ≥126 mg/dL or HbA1c level ≥6.5%] or when the patient was on antidiabetic medication for the condition. The criteria for diabetic remission was defined as FBS <126 mg/dL and HbA1c level <6.5% without the use of any antidiabetic medications (oral hyperglycemic agents or insulin) after surgery.9 We defined dyslipidemia as the presence of one or more abnormalities in serum triglycerides (≥130 mg/dL), low-density lipoprotein cholesterol (≥130 mg/dL) or high-density lipoprotein cholesterol (<40 mg/dL) levels, or current lipid lowering medication.10 The remission of hypertension was defined as normal blood pressure values without medication.
All statistical analyses were performed by using SPSS version 18 for Windows (SPSS Inc., Chicago, IL, USA). Medians and ranges of the variables were calculated and compared between the two different procedures. The chi-square test or Fisher's exact test was applied to analyze categorical variables, and the Mann-Whitney U test was used for continuous variables. All tests were two-tailed and a p-value <0.05 was considered significant.
Twenty-two patients aged between 14 and 20 years underwent bariatric surgery at our institution for the treatment of morbid obesity and combined comorbidities. The demographic characteristics of the patients are described in detail in Table 1. The study cohort consisted of 5 males and 17 females. The mean age of the enrolled patients was 19 years (range, 14-20). Their mean body weight and BMI before surgery were 115 kg (range, 93-150) and 40.1 kg/m2 (range 33.4-55.6). Fourteen patients underwent sleeve gastrectomy, while the other eight patients underwent Roux-en-Y gastric bypass surgery. All operations were performed laparoscopically and none were converted to laparotomy. No patients experienced intraoperative complications. Most patients were discharged from hospital within 1 day after surgery without any adverse events. One patient was presented with immediate postoperative intraluminal bleeding after LRYGB, which spontaneously discontinued after a few days of close observation. She required 2 units of packed red blood cells and was discharged on the fourth postoperative day after the absence of continued bleeding was confirmed. The mean follow-up period was 10 months (range, 3-36 months). There were no hospital readmissions and/or deaths during the follow-up period. Seven patients (4 following LSG, 3 following LRYGB) required empirical proton-pump inhibitors to manage heartburn or epigastric soreness. Three patients developed symptomatic nephrolithiasis.
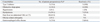
Most patients had one or more obesity-related comorbidities preoperatively. The types and frequencies of comorbidities are summarized in Table 2. Dyslipidemia (13/22, 59.1%) diagnosed biochemically and fatty liver disease (10/22, 45.5%) noted on preoperative evaluation by performing ultrasonography or abdominal computed tomography were the most common of these. Three patients (18.2%) had type 2 diabetes, and one of them was newly diagnosed during the preoperative evaluation. Hypertension was present in two patients (9.1%), and both were taking antihypertensive medications. Four patients (18.2%) were on treatment with continuous positive airway pressure for obstructive sleep apnea. Gastroesophageal reflux was confirmed in three patients (13.6%) by performing endoscopy or barium upper gastrointestinal radiography. Additionally, the majority of female patients (12/17, 70.6%) were suffering from menstrual irregularity with the diagnosis of polycystic ovarian disease and four patients (18.2%) had concurrent psychosocial problems, such as depression.
The resolution of comorbidities after surgery was observed in a majority of the patients after a mean follow-up of 10 months (Table 2). All patients with diabetes were cured of their disease and those with sleep apnea were relieved from the symptoms. Other comorbidities such as hypertension, dyslipidemia and gastroesophageal reflux had also improved or resolved after surgery in more than half of the patients for whom data were available. Three out of four patients taking antidepressants also discontinued their medication during the follow-up period.
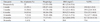
The median BMI decreased from 40.1 to 29.1 kg/m2 at a mean follow-up of 10 months. The postoperative BMI and %EWL at each follow-up time point are shown in detail in Table 3. By 6 months postoperatively, 10 of 14 patients (71.4%) with available body weight data had achieved 50% or more EWL. The median %EWL at this time point was 52.6% (range, 33.2-94.0). Only 1 of 7 patients showed %EWL less than 30% at 12 months after surgery; a 20-year old female patient had mental retardation and had undergone LSG.
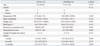
The enrolled patients were further divided into 2 subgroups according to operative procedure (LSG vs. LRYGB) and their surgical outcomes were compared (Table 4). Preoperative demographic characteristics and anthropometric measures in both groups were similar. The operating time was significantly longer in the LRYGB group than in the LSG group, with a difference of approximately 30 minutes (127 min vs. 100 min). The %EWL at 1, 6, and 12 months after surgery did not show a statistically significant difference between both groups.
In Korea, the overall prevalence of obesity in children and adolescents significantly increased from 5.8% in 1997 to 9.7% in 2005.11 Although the prevalence of obesity in Korean adolescents is still far lower than that in American adolescents, 12 it is true that the number of Korean children suffering from morbid obesity is rapidly increasing. This issue has become a growing national concern as a public health problem, especially in view of the possible obesity-related comorbidities.
Childhood obesity is closely related to subsequent obesity, morbidity, and mortality in adulthood,4,5 which in turn results in prolonged impairment of quality of life. Various traditional methods of weight loss have been tried in an attempt to achieve sustained weight loss and the resolution of comorbidities in children. Although intensive behavioral interventions and pharmacologic treatment can be effective in managing weight in obese children and adolescents, the effect is only modest and often fails to satisfy long-term goals.13 Bariatric surgery in childhood, therefore, has gradually drawn attention, and an increasing number of investigators have demonstrated the safety and effectiveness of bariatric surgery for children and adolescents by reporting successful surgical outcomes. However, most of the clinical data available on the efficacy and complications of the surgical intervention in adolescents are based on several small case series, usually from Western populations. Therefore, we intended to report our initial experience of weight loss surgery performed in morbidly obese Korean adolescents. To our knowledge, this is the first study to review the outcomes of bariatric surgery in Korean adolescents.
We adopted LRYGB and LSG for our patient cohort amongst various bariatric procedures; the choice of procedure was made on an individual basis by the surgeon in discussion with the patient and his or her parents. In the present study, patients achieved EWL of 62.8% at a mean follow-up duration of 10 months. One patient showed only 27.7% EWL at 1 year postoperatively following LSG, and the reason seems to be poor compliance with perioperative management due to her mental retardation. This patient was referred to surgery primarily because of severe obstructive sleep apnea, and the symptom eventually resolved after LSG despite her unsatisfactory weight loss. There are currently no standards for defining weight loss success or failure after bariatric surgery. Generally, a cut-off value for EWL of 50% or more has been used to define success14 and EWL of 25% or less is often considered failure.15 However, some researchers consider that %EWL is not the optimal indicator for monitoring weight loss in children, as height increase, which directly influences ideal body weight during follow-up, is not reflected in this indicator.16,17 The age of the patients included in the present study ranged from 14 to 20 years, with a median age of 19, and the majority of the enrolled patients were over 15 years old. At this age, most have passed their growth spurt and completed the bulk of their physical growth, which suggests that the impact of the height difference on final outcomes is largely moot in this patient cohort. Intraluminal bleeding was the only postoperative complication noted and it spontaneously halted during conservative observation. Interestingly, a relatively large number of patients (7/22, 31.8%) complained of heartburn or epigastric soreness during postoperative follow-up, implying the presence of reflux or marginal ulcer, and they were managed symptomatically with proton-pump inhibitors. Gastroesophageal reflux disease and marginal ulcer are already well-known as the most common postoperative complications after LSG and LRYGB, respectively. Since few studies of adolescent bariatric surgery have reported on such clinical symptoms, it is impossible to compare our results with others. Otherwise, this study shows similar short-term results with previous studies of adolescent bariatric surgery, although the long-term outcomes remain to be seen. LRYGB seems to be slightly superior to LSG in terms of %EWL, although it was not statistically significant due to the small number of enrolled patients. Longer follow-up may elaborate the further difference between the procedures.
In addition to the emphasis on weight, the resolution of the obesity-related comorbid conditions should be an important metric by which the success of bariatric surgery is evaluated. This is even more important in the Korean population, because Asians have a higher risk of comorbid diseases at a lower BMI than do Western populations.18 Furthermore, Korean adolescents seems to be more vulnerable to certain factors of the metabolic syndrome when compared to American adolescents.12,19 In the present study, the baseline BMI is relatively low compared to that reported in previous studies, with a median BMI of 40.1 kg/m2, but the prevalence of comorbid conditions seems to be comparable.20 It appears that, in our patient cohort, bariatric surgery was indicated for adolescent patients with relatively low BMI because of their comorbid conditions; this is consistent with the aforementioned characteristic of Asian populations. In this initial experience, the majority of obesity-related comorbidities, especially diabetes and obstructive sleep apnea, improved or resolved after surgery. No consensus has been reached as yet regarding the appropriate BMI cut-offs for adolescent bariatric surgery candidacy. Recommendations point out that the criteria should be tailored for individual patients considering their needs and maturity level. It seems that the distinct characteristics of the Asian adolescent population needs to be considered when establishing proper guidelines for adolescent bariatric surgery in Asians, just as different indications have been adopted for morbidly obese adults in the Asian population.21
A recent publication revealed that the bariatric procedure rate for adolescent patients in the United States has plateaued between 2003 and 2009, contrary to the expectation that it would have rapidly increased along with the worsening childhood obesity epidemic.22 The major concerns with regard to performing bariatric surgery in pediatric patients are the physiologic implications of this rather drastic approach in this age group, a potential to induce metabolic and growth consequences, and a lack of information about long-term efficacy.23 Little is known about the long-term safety of adolescent bariatric surgery, because these procedures have only recently been applied to this population. Unfortunately, this study could not elucidate any possible outcomes regarding the impact of physical maturation or long-lasting nutritional effect due to its short-term follow up period. Further studies with long-term follow-up will answer many emerging questions regarding the role of bariatric surgery in adolescents.
There are many limitations to the present study. This study is based on a retrospective review, and this may have introduced bias in analysis of the outcomes. The results from two different surgical procedures are combined together for the outcome analyses. The number of enrolled patients is so small that it is difficult to detect statistically significant differences between procedures. The diagnosis for obesity-related comorbidities is generally based on clinical findings rather than the application of strict diagnostic criteria and the follow-up data for those comorbidities were often missing, which may have introduced bias. Furthermore, there were several patients who were unreachable even by telephone interview and their outcomes were not known after short-term follow-up. Furthermore, the follow-up period was relatively short, less than 1 year on average, and the long-term results need to be seen in the future.
In conclusion, successful weight loss occurred with minimal complications after both LSG and LRYGB in morbidly obese Korean adolescents, leading to significant resolution of the obesity-related comorbidities. Further studies are necessary to elucidate the long-term safety and efficacy of bariatric surgery in morbidly obese adolescents.
Figures and Tables
References
1. Kimm SY, Obarzanek E. Childhood obesity: a new pandemic of the new millennium. Pediatrics. 2002; 110:1003–1007.

2. Weiss R, Dziura J, Burgert TS, Tamborlane WV, Taksali SE, Yeckel CW, et al. Obesity and the metabolic syndrome in children and adolescents. N Engl J Med. 2004; 350:2362–2374.

3. Kiess W, Galler A, Reich A, Müller G, Kapellen T, Deutscher J, et al. Clinical aspects of obesity in childhood and adolescence. Obes Rev. 2001; 2:29–36.

4. Guo SS, Wu W, Chumlea WC, Roche AF. Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr. 2002; 76:653–658.

5. Must A, Jacques PF, Dallal GE, Bajema CJ, Dietz WH. Long-term morbidity and mortality of overweight adolescents. A follow-up of the Harvard Growth Study of 1922 to 1935. N Engl J Med. 1992; 327:1350–1355.

6. Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013; 273:219–234.

7. No JH, Kim Z, Kim YJ, Cho SW, Choi DH, Hur KY, et al. Initial experience of laparoscopic sleeve gastrectomy in morbidly obese patients. J Korean Surg Soc. 2010; 79:460–466.

9. Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003; 26:Suppl 1. S5–S20.
10. National Cholesterol Education Program (NCEP): highlights of the report of the Expert Panel on Blood Cholesterol Levels in Children and Adolescents. Pediatrics. 1992; 89:495–501.
11. Oh K, Jang MJ, Lee NY, Moon JS, Lee CG, Yoo MH, et al. Prevalence and trends in obesity among Korean children and adolescents in 1997 and 2005. Korean J Pediatr. 2008; 51:950–955.

12. Park J, Hilmers DC, Mendoza JA, Stuff JE, Liu Y, Nicklas TA. Prevalence of metabolic syndrome and obesity in adolescents aged 12 to 19 years: comparison between the United States and Korea. J Korean Med Sci. 2010; 25:75–82.

13. Whitlock EP, O'Connor EA, Williams SB, Beil TL, Lutz KW. Effectiveness of weight management interventions in children: a targeted systematic review for the USPSTF. Pediatrics. 2010; 125:e396–e418.

14. O'Brien PE, Sawyer SM, Laurie C, Brown WA, Skinner S, Veit F, et al. Laparoscopic adjustable gastric banding in severely obese adolescents: a randomized trial. JAMA. 2010; 303:519–526.
15. Angrisani L, Favretti F, Furbetta F, Paganelli M, Basso N, Doldi SB, et al. Obese teenagers treated by Lap-Band System: the Italian experience. Surgery. 2005; 138:877–881.

16. Cole TJ, Faith MS, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutr. 2005; 59:419–425.

17. Alqahtani AR, Antonisamy B, Alamri H, Elahmedi M, Zimmerman VA. Laparoscopic sleeve gastrectomy in 108 obese children and adolescents aged 5 to 21 years. Ann Surg. 2012; 256:266–273.

18. WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004; 363:157–163.
19. Lim S, Jang HC, Park KS, Cho SI, Lee MG, Joung H, et al. Changes in metabolic syndrome in American and Korean youth, 1997-2008. Pediatrics. 2013; 131:e214–e222.

20. Treadwell JR, Sun F, Schoelles K. Systematic review and meta-analysis of bariatric surgery for pediatric obesity. Ann Surg. 2008; 248:763–776.

21. Kasama K, Mui W, Lee WJ, Lakdawala M, Naitoh T, Seki Y, et al. IFSO-APC consensus statements 2011. Obes Surg. 2012; 22:677–684.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download