Abstract
Purpose
This study aimed to assess the role of thiopurine S-methyltransferase (TPMT) and 6-thioguanine nucleotide (6-TGN) as predictors of clinical response and side effects to azathioprine (AZA), and estimate the optimal AZA dose in Korean pediatric inflammatory bowel disease (IBD) patients.
Materials and Methods
One hundred and nine pediatric IBD patients in whom AZA treatment was required were enrolled. Thiopurine metabolites were monitored since September 2010. Among them, 83 patients who had prescribed AZA for at least 3 months prior to September 2010 were enrolled and followed until October 2011 to evaluate optimal AZA dose, adverse effects and disease activity before and after thiopurine metabolite monitoring.
Results
The result of the TPMT genotype was that 102 patients were *1/*1 (wild type), four were *1/*3C, one was *1/*6, one was *1/*16 (heterozygote) and one was *3C/*3C (homozygote). Adverse effects happened in 31 patients pre-metabolite monitoring and in only nine patients post-metabolite monitoring. AZA dose was 1.4±0.31 mg/kg/day before monitoring and 1.1±0.46 mg/kg/day after monitoring (p<0.001). However, there were no statistical differences in disease activity during metabolite monitoring period (p=0.34). Adverse effects noticeably decreased although reduction of the AZA dose since monitoring.
Inflammatory bowel disease (IBD), which includes Crohn's disease (CD) and ulcerative colitis (UC), is characterized by chronic relapsing inflammation of the gastrointestinal tract. Azathioprine (AZA) is the most common drug used to maintain clinical remission in CD and UC.1,2 This drug is also important as a steroid-sparing agent in steroid-dependent and chronically active IBD. However, the dose of AZA has to be reduced or the therapy has to be discontinued in 9-28% of patients because of drug-induced toxicity.3 Bone marrow suppression, gastrointestinal disturbances, hepatotoxicity, pancreatitis, fever, and rash are among the most frequent reasons for AZA reduction/cessation in some patients.4 Although there are some adverse reactions that clinicians should be aware of, monitoring 6-thioguanine nucleotide (6-TGN) and 6-methylmercaptopurine (6-MMP) levels enables safe and long-term remission in IBD patients.5,6
Thiopurine S-methyltransferase (TPMT) is the key enzyme in the metabolic pathway of thiopurine compounds. Patients with low enzyme activity have elevated 6-TGN levels and an increased risk of bone marrow suppression when treated with standard doses of AZA.7,8 Patients with high enzyme activity are either resistant to AZA due to shunting of thiopurine drugs down the 6-MMP pathway9,10,11 or require a high dose to achieve efficacy, but have an increased risk of hepatotoxicity due to high 6-MMP levels.12,13 About 10% of the patients are intermediate activity group due to heterozygosity of the TPMT, and 0.3% of the patients have undetectable TPMT activity as an homozygote.9 The wild type is TPMT*1, and TPMT*3A is the most common mutant allele (85%) in Caucasians9 and TPMT*3C is the most prevalent mutant allele in Africans and Asians.12,13,14
The aim of this study was to evaluate the role of 6-TGN and TPMT as predictors of adverse effects and clinical resp-onse to AZA, using a well-powered study of pediatric patients with IBD. We also tried to determine the optimal dose of AZA maintaining remission in the Korean pediatric IBD patients.
Among pediatric patients who were diagnosed with CD or UC in accordance with the European Society for Pediatric Gastroenterology, Hepatology and Nutrition-Porto criteria15 at the Samsung Medical Center from March 2004 to October 2011, we enrolled 109 patients who required AZA to maintain remission. There were 87 CD patients and 22 UC patients ranging in age from 3 to 21 years. Before using AZA, the TPMT genotype was analyzed. The patients had been prescribed a consistent dose of AZA for at least 3 months prior to the study. A retrospective chart analysis was conducted by physician notes, laboratory studies, radiology reports, endoscopy records, and histology reports. This study was approved by our Institutional Review Board.
Analysis of TPMT genotype was available throughout the study period, and thiopurine metabolite monitoring has been available since September 2010. One hundred and nine IBD patients have been monitored for thiopurine metabolites since September 2010. Of them, 83 cohorts who had received a consistent dose of AZA for at least 3 months prior to September 2010 were selected and followed until October 2011 for the assessment of adverse drug reactions (ADR), disease activity and optimal AZA dose to maintain remission at pre- and post-thiopurine metabolite monitoring period. The appraisal of ADR, disease activity and AZA dose in 83 patients was performed and compared between just before the beginning of thiopurine metabolite monitoring (September 2010) and when 6-TGN level attained an optimal therapeutic range of approximately 235-450 pmol/8×108 red blood cells (RBC).16,17
AZA treatment was initiated at a dose of approximately 1.0 mg/kg per day and then increased to approximately 1.5 mg/kg per day in order to maintain remission during maintenance therapy. Patients were required to visit the outpatient clinic at least once a month before remission of the disease, and once every 2 to 3 months after remission was obtained. Laboratory tests were conducted in order to monitor disease activity and adverse drug reactions at each visit. Routine blood examinations including complete blood cell counts, erythrocyte sedimentation rate, albumin, transaminase, amylase, lipase and C-reactive protein were carried out. Disease activity was evaluated using the pediatric UC activity index (PUCAI)18 and the pediatric CD activity index (PCDAI).19 In both activity indices, scores of less than 10 points are considered to be in remission, while scores above 10 points are considered indicative of active disease.
Whole blood specimens were collected into EDTA tubes, and genomic DNA was isolated from peripheral blood leukocytes using the Wizard Genomic DNA Purification kit according to the manufacturer's instructions (Promega, Madison, WI, USA).
All nine exons of the TPMT gene were amplified on a model 9700 thermal cycler (Applied Biosystems, Foster City, CA, USA) using oligonucleotide primers and conditions as previously described with some modifications.20,21 Direct sequencing was performed using ABI Big Dye Terminator kit v1.1 (Applied Biosystems) according to the manufacturer's instructions. To identify sequence variations, patient sequences were compared with respective reference sequences using the Sequencher software (Gene Codes Corporation, Ann Arbor, MI, USA).
Measurements of the RBC 6-TGN and 6-MMP levels were performed on the Waters 2795 Alliance high-performance liquid chromatography system and a Quatro Micro API tandem mass spectrometer (Waters, Manchester, UK).22 Six calibrators and two control materials (mixture with 6-TGN and 6-MMP stock solutions and RBCs from pooled whole blood after removal of plasma and buffy coat) were used in each analysis. Within-run and between-run imprecision for thiopurine metabolites were below 10%. The limit of quantification was 5 ng/mL for 6-TGN and 50 ng/mL for 6-MMP.
All collected variables were subjected to descriptive analysis. Results are expressed as mean±standard deviation or range for numerical variables and as percentages for qualitative variables. A Student t-test or Mann-Whitney U test was used to compare numerical variables between groups and the χ2 test or Fisher exact test was used to investigate the relationship between the variables. A p-value <0.05 was considered statistically significant.
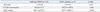
A total of 109 patients were studied. All patients were treated with AZA; the mean dose of AZA was 1.2±0.38 mg/kg/day. The demographic and clinical characteristics of patients enrolled in this study are shown in Table 1.
The mean 6-TGN concentration of the entire study population was 328.3±105.0 pmol/8×108 RBC. The mean 6-TGN concentration was 299.7±77.1 pmol/8×108 RBC in patients with active disease (n=24), and 336.3±110.7 pmol/8×108 RBC among patients in remission (n=85). There were no statistical differences in 6-TGN levels between patients with active disease and patients in remission (p=0.73).
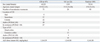
Definitions of ADR in this study are shown in Table 2. ADR occurred in 38 patients (34.8%). Among these patients, gastric intolerance occurred in two patients (1.8%), rash in two (1.8%), leukopenia in 24 (22.0%) and hair loss in 10 (9.2%) (Table 2). Only three of 24 leukopenia events could be explained by TPMT mutation. The mean AZA dose was 1.1±0.53 mg/kg/day in patients developing ADR, which was not significantly different from that (1.2±0.35 mg/kg/day) of the patients who did not develop ADR (p=0.45).
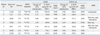
The distribution of the TPMT genotype was as follows: 102 patients had *1/*1 (wild type), one had *3C/*3C (homozygote, NM_000367.2: c.719A>G; p.Tyr240Cys), four had *1/*3C, one had *1/*6, and one had *1/*16 (heterozygote). There were no statistical differences in initial AZA dose between the group of wild type TPMT and TPMT mutation. However, the 6-TGN concentration was 416.8±271.7 pmol/8×108 RBC in patients with wild type TPMT and 1822.9±1493.9 pmol/8×108 RBC in TPMT mutation (p=0.001). There were also statistical differences in white blood cell counts among two groups (p=0.028) (Table 3). The patient with *3C/*3C mutation required low dose of AZA, 0.18 mg/kg/day to maintain an optimal therapeutic range. Three of four patients with *1/*3C mutation had ADR such as leukopenia, rash and hair loss. However, two patients with *1/*6 and *1/*16 mutation did not present any ADR (Table 4).
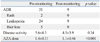
Sixty-seven CD patients and 16 UC patients were selected for assessing ADR, disease activity (PCDAI or PUCAI) and AZA dose before and after thiopurine metabolite monitoring. ADR happened in 31 patients pre-metabolite monitoring and in only nine patients post-metabolite monitoring. AZA dose was 1.4±0.31 mg/kg/day before monitoring and 1.1±0.46 mg/kg/day after monitoring (p<0.001). However, there were no statistical differences in disease activity during metabolite monitoring period (p=0.34) (Table 5).
Thiopurine has been commonly used for the maintenance of remission or for treating chronic active lesions in IBD. The use of AZA in adult patients with IBD has been well documented in the literature and also recently reported in pediatric studies.23,24,25 Present, et al.23 demonstrated that 67% of adult patients significantly decreased or terminated their steroid therapy 3-6 months after the introduction of oral immunomodulators. Similar results have been demonstrated in pediatric patients.26,27,28
One of the potentially severe side effects in AZA therapy is myelosuppression. AZA-induced bone marrow suppression has been attributed to the low enzyme activity caused by TPMT genetic polymorphism.29,30 Genetic polymorphism results in greater conversion of AZA to 6-TGN likely due to myelotoxicity.3,17 Consequently, the monitoring of 6-TGN levels has been known to be useful for managing IBD patients treating with AZA, since it may confirm the optimal AZA dose to maximize efficacy while minimizing the risk of side effect.5,31 The aim of this study was to investigate the influence of TPMT genotype and 6-TGN concentrations on the development of adverse effects during AZA treatment in children and adolescents with IBD.
TPMT can be examined for based on phenotype or genotype tests. TPMT genotyping is the method for detecting single nucleotide polymorphism responsible for TPMT inactivation. There is a good correlation between TPMT activity and genotyping.32 The population can be divided into three groups founded on TPMT genetic polymorphism: wild type TPMT with high methylation activity (88%), heterozygosity with intermediate activity (11%) and homozygosity for deficient TPMT alleles with a low activity (0.3%).33 Until now, 27 TPMT alleles which are *2,*3A,*3B,*3C,*3D, and *4 to *25 responsible for possible deficient activity have been detected.34
In Asian populations, including Koreans, the frequencies of TPMT mutation are lower than those reported for Western countries.35,36,37,38,39,40 While the heterozygous *2 or *3A mutations are rare, *3C mutation is most frequent and myelotoxicity develops more frequently in East Asia.41,42,43,44 The reason why Asian patients are troubled with bone marrow suppression during AZA administration is still unclear. One possible theory is the difference in TPMT genetic polymorphisms between Asian and Caucasian populations. Kim, et al.45 from Korea suggested that it could be reasonable to obtain TPMT genotypes before starting AZA treatment for predicting the development of leukopenia.
A TPMT genotyping study of 400 Korean subjects suggested that TPMT *1/*1 (wild type) was 97.8% (391/400).35 TPMT *1/*3C was found to be the most frequent polymorphism in the Korean population (1.8%). TPMT *2, *3A, and *3B were not found in the study population. Two Korean subjects were genotyped as TPMT *1/*6 (0.5%). Another TPMT study of 147 Japanese IBD patients suggested that wild type for TPMT was 98.0% (144/147) and TPMT *1/*3C was 2.0% (3/147) similar to Korean study.40 To our knowledge, our study is the first work to detect TPMT *3C/*3C and *1/*16 mutations and to evaluate 6-TGN concentrations and dosing of optimal AZA in Korean pediatric IBD patients. In our study, TPMT polymorphism was proven in seven patients. The patients with TPMT polymorphism required a low dose of AZA to attain an optimal therapeutic range of 6-TGN. TPMT *3C/*3C and *1/*3C mutation was highly associated with a risk of ADR as it is known. However, TPMT *1/*6 and *1/*16 mutations were not related with ADR. There is no doubt that TPMT testing is necessary before initiation of AZA to identify individuals who are homozygote recessive or have extremely low TPMT activity.46 However, TPMT testing doesn't predict all cases of ADR such as leukopenia. Mutations of TPMT have been associated with leukopenia,3,13,47,48,49 although other studies have reported that leukopenia is independent of TPMT polymorphisms.50,51,52 Because only 3 of 24 leukopenia events could be explained by TPMT mutation, the association between TPMT polymorphisms and ADR was probably heterogeneous. However, we suggest that the correlation exists between TPMT polymorphism and the development of ADR because 4 of 7 patients with TPMT polymorphism presented ADR.
AZA is an inactive prodrug that is metabolized to produce the nucleotide metabolites, 6-TGN, 6-MMP, and 6-thiouracil. Among these metabolites, 6-TGN seems to be one of the active metabolites accountable for therapeutic efficacy. In diverse studies, significant correlations have been found between 6-TGN concentration and clinical response in IBD and a therapeutic range of 6-TGN concentration is 235-450 pmol/8×108 RBC.6,53,54,55 A 6-TGN concentration of >235 pmol/8×108 RBC is associated with clinical response.6,53 The cutoff concentration above 450 pmol/8×108 RBC is based on an increased risk of side effects (myelotoxicity55 and nodular regenerative hyperplasia of the liver56) without an increase in efficacy. Patients with erythrocyte 6-MMP concentrations above 5700 pmol/8×108 RBC are at increased risk of hepatotoxicity and are unlikely to respond to treatment by increasing the drug dose.53,57,58 These patients are possibly preferentially metabolizing AZA through TPMT to form 6-MMP and may profit from reducing thiopurine dose by 50-75%, as well as careful monitoring of hematological parameters.59
Osterman, et al.60 and Sandborn, et al.61 documented that the doses of AZA in maintenance therapy to treat IBD were 2-3 mg/kg/day, and that 6-TGN concentrations above 235 pmol/8×108 RBC were confirmed in most IBD patients with this dose. A study of Japanese children with IBD showed that similar 6-TGN concentrations should be targeted to maintain remission, although the amounts of AZA required to achieve the targeted 6-TGN concentration were lower than those used in Western countries.62,63 In Korea, lower doses of AZA (approximately 1.5-2 mg/kg AZA per day) are empirically used for the treatment of IBD patients.64,65 However, there has been no data on the dose of AZA that is needed to reach appropriate 6-TGN level in Korean children and adolescents with IBD.
In agreement with previous investigations,5,55,60,66 our study showed that the mean 6-TGN concentration was higher in patients with clinical remission (336.3±110.7 pmol/8×108 RBC) than with active disease (299.7±77.1 pmol/8×108 RBC). However, there were no statistical differences. In the present study, since thiopurine metabolite monitoring, ADR has markedly decreased and AZA dose reduced to 1.1±0.46 mg/kg/day with maintaining remission. Only 8 of 38 ADR events were associated with TPMT polymorphism; and the rest of the ADR events occurred in wild type of TPMT. Therefore, surveillance of ADR through thiopurine metabolite monitoring is possibly important to the patients, with not only TPMT polymorphism but also wild type of TPMT.
As we described above, our results indicated that 6-TGN concentration was higher than we expected in pediatric IBD patients, even though they were treated with low-dose of AZA. These results are similar to those of a study conducted in the Far East, however, different from studies reported in Western countries.60,61,62,66 One explanation for this might be an ethnic difference.
Our study had several limitations, including the small number of patients and the retrospective design. In Korea, the incidence and prevalence of IBD are still low compared with those in Western countries.67 Considering these circumstances, we recruited not a few number of pediatric patients with IBD in Korea. Monitoring 6-TGN concentrations is helpful in developing a therapeutic strategy for pediatric and adolescent IBD patients. Although TPMT genotype and thiopurine metabolite monitoring could not completely explain the thiopurine-induced ADR, it could be helpful to examine TPMT genotypes before administering AZA and to measure 6-TGN concentrations during prescribing AZA in IBD patients. Clinicians should be cautious about the possibility of higher 6-TGN concentrations in Korean pediatric IBD patients, even if they are being treated with general AZA dose.
Figures and Tables
Table 3
Comparison of AZA Dose, 6-TGN Concentration and White Blood Cell Counts between the Group of Wild Type TPMT and TPMT Mutation
ACKNOWLEDGEMENTS
This study was supported by the Samsung Biomedical Research Institute grant, no. SBRI C-A6-229-3.
References
1. Sandborn W, Sutherland L, Pearson D, May G, Modigliani R, Prantera C. Azathioprine or 6-mercaptopurine for inducing remission of Crohn's disease. Cochrane Database Syst Rev. 2000; CD000545.
2. Hibi T, Ogata H. Novel pathophysiological concepts of inflammatory bowel disease. J Gastroenterol. 2006; 41:10–16.

3. Hindorf U, Lindqvist M, Peterson C, Söderkvist P, Ström M, Hjortswang H, et al. Pharmacogenetics during standardised initiation of thiopurine treatment in inflammatory bowel disease. Gut. 2006; 55:1423–1431.

4. Gearry RB, Barclay ML, Burt MJ, Collett JA, Chapman BA. Thiopurine drug adverse effects in a population of New Zealand patients with inflammatory bowel disease. Pharmacoepidemiol Drug Saf. 2004; 13:563–567.

5. Goldenberg BA, Rawsthorne P, Bernstein CN. The utility of 6-thioguanine metabolite levels in managing patients with inflammatory bowel disease. Am J Gastroenterol. 2004; 99:1744–1748.

6. Cuffari C, Hunt S, Bayless T. Utilisation of erythrocyte 6-thioguanine metabolite levels to optimise azathioprine therapy in patients with inflammatory bowel disease. Gut. 2001; 48:642–646.

7. Lennard L, Van Loon JA, Lilleyman JS, Weinshilboum RM. Thiopurine pharmacogenetics in leukemia: correlation of erythrocyte thiopurine methyltransferase activity and 6-thioguanine nucleotide concentrations. Clin Pharmacol Ther. 1987; 41:18–25.

8. Lennard L, Van Loon JA, Weinshilboum RM. Pharmacogenetics of acute azathioprine toxicity: relationship to thiopurine methyltransferase genetic polymorphism. Clin Pharmacol Ther. 1989; 46:149–154.

9. Yates CR, Krynetski EY, Loennechen T, Fessing MY, Tai HL, Pui CH, et al. Molecular diagnosis of thiopurine S-methyltransferase deficiency: genetic basis for azathioprine and mercaptopurine intolerance. Ann Intern Med. 1997; 126:608–614.

10. Cuffari C, Dassopoulos T, Turnbough L, Thompson RE, Bayless TM. Thiopurine methyltransferase activity influences clinical response to azathioprine in inflammatory bowel disease. Clin Gastroenterol Hepatol. 2004; 2:410–417.

11. Lennard L, Lilleyman JS, Van Loon J, Weinshilboum RM. Genetic variation in response to 6-mercaptopurine for childhood acute lymphoblastic leukaemia. Lancet. 1990; 336:225–229.

12. Winter JW, Gaffney D, Shapiro D, Spooner RJ, Marinaki AM, Sanderson JD, et al. Assessment of thiopurine methyltransferase enzyme activity is superior to genotype in predicting myelosuppression following azathioprine therapy in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2007; 25:1069–1077.

13. Ishioka S, Hiyama K, Sato H, Yamanishi Y, McLeod HL, Kumagai K, et al. Thiopurine methyltransferase genotype and the toxicity of azathioprine in Japanese. Intern Med. 1999; 38:944–947.

14. Cao Q, Zhu Q, Shang Y, Gao M, Si J. Thiopurine methyltransferase gene polymorphisms in Chinese patients with inflammatory bowel disease. Digestion. 2009; 79:58–63.

15. IBD Working Group of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition. Inflammatory bowel disease in children and adolescents: recommendations for diagnosis--the Porto criteria. J Pediatr Gastroenterol Nutr. 2005; 41:1–7.
16. Derijks LJ, Gilissen LP, Hooymans PM, Hommes DW. Review article: thiopurines in inflammatory bowel disease. Aliment Pharmacol Ther. 2006; 24:715–729.

17. Gearry RB, Barclay ML. Azathioprine and 6-mercaptopurine pharmacogenetics and metabolite monitoring in inflammatory bowel disease. J Gastroenterol Hepatol. 2005; 20:1149–1157.

18. Turner D, Otley AR, Mack D, Hyams J, de Bruijne J, Uusoue K, et al. Development, validation, and evaluation of a pediatric ulcerative colitis activity index: a prospective multicenter study. Gastroenterology. 2007; 133:423–432.

19. Hyams J, Markowitz J, Otley A, Rosh J, Mack D, Bousvaros A, et al. Evaluation of the pediatric crohn disease activity index: a prospective multicenter experience. J Pediatr Gastroenterol Nutr. 2005; 41:416–421.

20. Dorababu P, Nagesh N, Linga VG, Gundeti S, Kutala VK, Reddanna P, et al. Epistatic interactions between thiopurine methyltransferase (TPMT) and inosine triphosphate pyrophosphatase (ITPA) variations determine 6-mercaptopurine toxicity in Indian children with acute lymphoblastic leukemia. Eur J Clin Pharmacol. 2012; 68:379–387.

21. Zabala-Fernández W, Barreiro-de Acosta M, Echarri A, Carpio D, Lorenzo A, Castro J, et al. A pharmacogenetics study of TPMT and ITPA genes detects a relationship with side effects and clinical response in patients with inflammatory bowel disease receiving Azathioprine. J Gastrointestin Liver Dis. 2011; 20:247–253.
22. Dervieux T, Meyer G, Barham R, Matsutani M, Barry M, Boulieu R, et al. Liquid chromatography-tandem mass spectrometry analysis of erythrocyte thiopurine nucleotides and effect of thiopurine methyltransferase gene variants on these metabolites in patients receiving azathioprine/6-mercaptopurine therapy. Clin Chem. 2005; 51:2074–2084.

23. Present DH, Korelitz BI, Wisch N, Glass JL, Sachar DB, Pasternack BS. Treatment of Crohn's disease with 6-mercaptopurine. A long-term, randomized, double-blind study. N Engl J Med. 1980; 302:981–987.
24. Present DH, Meltzer SJ, Krumholz MP, Wolke A, Korelitz BI. 6-Mercaptopurine in the management of inflammatory bowel disease: short- and long-term toxicity. Ann Intern Med. 1989; 111:641–649.

25. Hanauer SB, Baert F. Medical therapy of inflammatory bowel disease. Med Clin North Am. 1994; 78:1413–1426.

26. Kirschner BS. Safety of azathioprine and 6-mercaptopurine in pediatric patients with inflammatory bowel disease. Gastroenterology. 1998; 115:813–821.

27. Markowitz J, Grancher K, Mandel F, Daum F. Subcommittee on Immunosuppressive Use of the Pediatric IBD Collaborative Research Forum. Immunosuppressive therapy in pediatric inflammatory bowel disease: results of a survey of the North American Society for Pediatric Gastroenterology and Nutrition. Am J Gastroenterol. 1993; 88:44–48.
28. Kader HA, Mascarenhas MR, Piccoli DA, Stouffer NO, Baldassano RN. Experiences with 6-mercaptopurine and azathioprine therapy in pediatric patients with severe ulcerative colitis. J Pediatr Gastroenterol Nutr. 1999; 28:54–58.

29. Derijks LJ, Gilissen LP, Engels LG, Bos LP, Bus PJ, Lohman JJ, et al. Pharmacokinetics of 6-thioguanine in patients with inflammatory bowel disease. Ther Drug Monit. 2006; 28:45–50.

30. Haglund S, Taipalensuu J, Peterson C, Almer S. IMPDH activity in thiopurine-treated patients with inflammatory bowel disease - relation to TPMT activity and metabolite concentrations. Br J Clin Pharmacol. 2008; 65:69–77.

31. Gilissen LP, Derijks LJ, Bos LP, Bus PJ, Hooymans PM, Engels LG. Therapeutic drug monitoring in patients with inflammatory bowel disease and established azathioprine therapy. Clin Drug Investig. 2004; 24:479–486.

32. Schaeffeler E, Fischer C, Brockmeier D, Wernet D, Moerike K, Eichelbaum M, et al. Comprehensive analysis of thiopurine S-methyltransferase phenotype-genotype correlation in a large population of German-Caucasians and identification of novel TPMT variants. Pharmacogenetics. 2004; 14:407–417.

33. Weinshilboum RM, Sladek SL. Mercaptopurine pharmacogenetics: monogenic inheritance of erythrocyte thiopurine methyltransferase activity. Am J Hum Genet. 1980; 32:651–662.
34. Derijks LJ, Wong DR. Pharmacogenetics of thiopurines in inflammatory bowel disease. Curr Pharm Des. 2010; 16:145–154.

35. Lee SS, Kim WY, Jang YJ, Shin JG. Duplex pyrosequencing of the TPMT*3C and TPM*T6 alleles in Korean and Vietnamese populations. Clin Chim Acta. 2008; 398:82–85.

36. Hiratsuka M, Inoue T, Omori F, Agatsuma Y, Mizugaki M. Genetic analysis of thiopurine methyltransferase polymorphism in a Japanese population. Mutat Res. 2000; 448:91–95.

37. Chang JG, Lee LS, Chen CM, Shih MC, Wu MC, Tsai FJ, et al. Molecular analysis of thiopurine S-methyltransferase alleles in South-east Asian populations. Pharmacogenetics. 2002; 12:191–195.

38. Kham SK, Soh CK, Liu TC, Chan YH, Ariffin H, Tan PL, et al. Thiopurine S-methyltransferase activity in three major Asian populations: a population-based study in Singapore. Eur J Clin Pharmacol. 2008; 64:373–379.

39. Kham SK, Tan PL, Tay AH, Heng CK, Yeoh AE, Quah TC. Thiopurine methyltransferase polymorphisms in a multiracial asian population and children with acute lymphoblastic leukemia. J Pediatr Hematol Oncol. 2002; 24:353–359.

40. Takatsu N, Matsui T, Murakami Y, Ishihara H, Hisabe T, Nagahama T, et al. Adverse reactions to azathioprine cannot be predicted by thiopurine S-methyltransferase genotype in Japanese patients with inflammatory bowel disease. J Gastroenterol Hepatol. 2009; 24:1258–1264.

41. Collie-Duguid ES, Pritchard SC, Powrie RH, Sludden J, Collier DA, Li T, et al. The frequency and distribution of thiopurine methyltransferase alleles in Caucasian and Asian populations. Pharmacogenetics. 1999; 9:37–42.

42. Kumagai K, Hiyama K, Ishioka S, Sato H, Yamanishi Y, McLeod HL, et al. Allelotype frequency of the thiopurine methyltransferase (TPMT) gene in Japanese. Pharmacogenetics. 2001; 11:275–278.

43. Jun JB, Cho DY, Kang C, Bae SC. Thiopurine S-methyltransferase polymorphisms and the relationship between the mutant alleles and the adverse effects in systemic lupus erythematosus patients taking azathioprine. Clin Exp Rheumatol. 2005; 23:873–876.
44. Otterness D, Szumlanski C, Lennard L, Klemetsdal B, Aarbakke J, Park-Hah JO, et al. Human thiopurine methyltransferase pharmacogenetics: gene sequence polymorphisms. Clin Pharmacol Ther. 1997; 62:60–73.

45. Kim JH, Cheon JH, Hong SS, Eun CS, Byeon JS, Hong SY, et al. Influences of thiopurine methyltransferase genotype and activity on thiopurine-induced leukopenia in Korean patients with inflammatory bowel disease: a retrospective cohort study. J Clin Gastroenterol. 2010; 44:e242–e248.
46. Benkov K, Lu Y, Patel A, Rahhal R, Russell G, Teitelbaum J, et al. Role of thiopurine metabolite testing and thiopurine methyltransferase determination in pediatric IBD. J Pediatr Gastroenterol Nutr. 2013; 56:333–340.

47. Hibi T, Naganuma M, Kitahora T, Kinjyo F, Shimoyama T. Low-dose azathioprine is effective and safe for maintenance of remission in patients with ulcerative colitis. J Gastroenterol. 2003; 38:740–746.

48. Gisbert JP, Niño P, Rodrigo L, Cara C, Guijarro LG. Thiopurine methyltransferase (TPMT) activity and adverse effects of azathioprine in inflammatory bowel disease: long-term follow-up study of 394 patients. Am J Gastroenterol. 2006; 101:2769–2776.

49. Zelinkova Z, Derijks LJ, Stokkers PC, Vogels EW, van Kampen AH, Curvers WL, et al. Inosine triphosphate pyrophosphatase and thiopurine s-methyltransferase genotypes relationship to azathioprine-induced myelosuppression. Clin Gastroenterol Hepatol. 2006; 4:44–49.

50. Colombel JF, Ferrari N, Debuysere H, Marteau P, Gendre JP, Bonaz B, et al. Genotypic analysis of thiopurine S-methyltransferase in patients with Crohn's disease and severe myelosuppression during azathioprine therapy. Gastroenterology. 2000; 118:1025–1030.

51. Schwab M, Schäffeler E, Marx C, Fischer C, Lang T, Behrens C, et al. Azathioprine therapy and adverse drug reactions in patients with inflammatory bowel disease: impact of thiopurine S-methyltransferase polymorphism. Pharmacogenetics. 2002; 12:429–436.
52. Palmieri O, Latiano A, Bossa F, Vecchi M, D'Incà R, Guagnozzi D, et al. Sequential evaluation of thiopurine methyltransferase, inosine triphosphate pyrophosphatase, and HPRT1 genes polymorphisms to explain thiopurines' toxicity and efficacy. Aliment Pharmacol Ther. 2007; 26:737–745.

53. Dubinsky MC, Lamothe S, Yang HY, Targan SR, Sinnett D, Théorêt Y, et al. Pharmacogenomics and metabolite measurement for 6-mercaptopurine therapy in inflammatory bowel disease. Gastroenterology. 2000; 118:705–713.

54. Ooi CY, Bohane TD, Lee D, Naidoo D, Day AS. Thiopurine metabolite monitoring in paediatric inflammatory bowel disease. Aliment Pharmacol Ther. 2007; 25:941–947.

55. Wright S, Sanders DS, Lobo AJ, Lennard L. Clinical significance of azathioprine active metabolite concentrations in inflammatory bowel disease. Gut. 2004; 53:1123–1128.

56. Dubinsky MC. Optimizing immunomodulator therapy for inflammatory bowel disease. Curr Gastroenterol Rep. 2003; 5:506–511.

57. Dubinsky MC, Yang H, Hassard PV, Seidman EG, Kam LY, Abreu MT, et al. 6-MP metabolite profiles provide a biochemical explanation for 6-MP resistance in patients with inflammatory bowel disease. Gastroenterology. 2002; 122:904–915.

58. Derijks LJ, Gilissen LP, Engels LG, Bos LP, Bus PJ, Lohman JJ, et al. Pharmacokinetics of 6-mercaptopurine in patients with inflammatory bowel disease: implications for therapy. Ther Drug Monit. 2004; 26:311–318.

59. Haines ML, Ajlouni Y, Irving PM, Sparrow MP, Rose R, Gearry RB, et al. Clinical usefulness of therapeutic drug monitoring of thiopurines in patients with inadequately controlled inflammatory bowel disease. Inflamm Bowel Dis. 2011; 17:1301–1307.

60. Osterman MT, Kundu R, Lichtenstein GR, Lewis JD. Association of 6-thioguanine nucleotide levels and inflammatory bowel disease activity: a meta-analysis. Gastroenterology. 2006; 130:1047–1053.

62. Ohtsuka Y, Arai K, Aoyagi Y, Fujii T, Yamakawa Y, Ohtani K, et al. Monitoring 6-thioguanine nucleotide concentrations in Japanese children and adolescents with inflammatory bowel disease. J Gastroenterol Hepatol. 2010; 25:1626–1630.

63. Komiyama T, Yajima T, Kubota R, Iwao Y, Sakuraba A, Funakoshi S, et al. Lower doses of 6-mercaptopurine/azathioprine bring enough clinical efficacy and therapeutic concentration of erythrocyte 6-mercaptopurine metabolite in Japanese IBD patients. J Crohns Colitis. 2008; 2:315–321.

64. Lee HJ, Yang SK, Kim KJ, Choe JW, Yoon SM, Ye BD, et al. The safety and efficacy of azathioprine and 6-mercaptopurine in the treatment of Korean patients with Crohn's disease. Intest Res. 2009; 7:22–31.
65. Kim JH, Cheon JH, Kim TI, Kim WH. A Survey of Actual Clinical Practice Patterns in the Treatment of Inflammatory Bowel Disease in Korea. Intest Res. 2009; 7:79–85.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download