This article has been
cited by other articles in ScienceCentral.
Abstract
Purpose
Obstructive jaundice in patients with hepatocellular carcinoma (HCC) is uncommon (0.5-13%). Unlike other causes of obstructive jaundice, the role of endoscopic intervention in obstructive jaundice complicated by HCC has not been clearly defined. The aim of this study was to evaluate the clinical characteristics of obstructive jaundice caused by HCC and predictive factors for successful endoscopic intervention.
Materials and Methods
From 1999 to 2009, 54 patients with HCC who underwent endoscopic intervention to relieve obstructive jaundice were included. We defined endoscopic intervention as a clinical success when the obstructive jaundice was relieved within 4 weeks.
Results
Clinical success was achieved in 23 patients (42.6%). Patients in the clinical success group showed better Child-Pugh liver function (C-P grade A or B/C; 17/6 vs. 8/20), lower total bilirubin levels (8.1±5.3 mg/dL vs. 23.1±10.4 mg/dL) prior to the treatment, and no history of alcohol consumption. The only factor predictive of clinical success by multivariate analysis was low total bilirubin level at the time of endoscopic intervention, regardless of history of alcohol consumption [odds ratio 1.223 (95% confidence interval, 1.071-1.396), p=0.003]. The cut-off value of pre-endoscopic treatment total bilirubin level was 12.8 mg/dL for predicting the clinical prognosis. Median survival after endoscopic intervention in the clinical success group was notably longer than that in the clinical failure group (5.6 months vs. 1.5 months, p≤0.001).
Conclusion
Before endoscopic intervention, liver function, especially total bilirubin level, should be checked to achieve the best clinical outcome. Endoscopic intervention can be helpful to relieve jaundice in well selected patients with HCC.
Keywords: Hepatocellular carcinoma, obstructive jaundice, endoscopic retrograde cholangiopancreatography, palliative treatment
INTRODUCTION
Jaundice is a common presentation of hepatocellular carcinoma (HCC) and occurs in 5-44% of patients. However, obstructive jaundice is quite uncommon in HCC with an incidence of 0.5-13%.
1 The synonyms for obstructive jaundice in HCC are icteric type hepatoma or cholestatic type HCC.
2 Obstructive jaundice in HCC can be caused by tumor thrombus in the bile duct, hemobilia, and extrinsic tumor compression of the extrahepatic biliary tree.
In Korea, the death rate of HCC has been reported at 21.8/100000 in 2011 by the National Cancer Information Center; HCC has the second highest cancer mortality next to lung cancer. The prognosis for patients with hepatocellular jaundice in HCC is dismal. On the other hand, the prognosis for patients with obstructive jaundice caused by extra-hepatic duct obstruction is better.
2,
3 The mean survival of patients with obstructive jaundice caused by HCC treated with simple biliary drainages varies from 2.5 to 4.5 months, and when treated with combined palliative therapies, it ranges from 8 to 13.4 months.
1 Therefore, in cases of obstructive jaundice complicated by HCC, active endoscopic intervention, including endoscopic retrograde cholangiopancreatography (ERCP), could improve the prognosis.
However, the role of endoscopic intervention in HCC is not yet clearly defined. It is important to predict the outcomes of invasive interventions in patients with HCC, who have a bleeding tendency and other various conditions that can increase the rate of treatment-related complications. The aim of this study was to analyze the clinical characteristics of patients with obstructive jaundice caused by HCC who underwent endoscopic intervention and to identify predictors of successful outcomes.
MATERIALS AND METHODS
We included 54 patients with HCC who were treated from 1999 to 2009 with ERCP for obstructive jaundice at Severance Hospital, Yonsei University College of Medicine, in Seoul, Korea. The median age of the patients was 56.3 years (range: 38 to 78 years). Forty-seven patients (87%) were male. The diagnosis of HCC was based on either typical imaging findings on abdominal CT, liver MRI, or hepatic angiography, combined with elevated tumor markers such as α-fetoprotein (AFP); vitamin K absence or antagonist II (PIVKA-II); or pathologic confirmation.
Obstructive jaundice was diagnosed by the typical sign of biliary tree obstruction (narrowing and dilatation at distal and proximal parts of the biliary tract) on imaging studies and biochemical abnormalities, such as elevated total and direct bilirubin. Mechanisms of obstructive jaundice in HCC were divided into three groups: type 1 obstruction due to an intraluminal obstruction of the bile duct caused by a tumor thrombus or floating tumor fragments; type 2 caused by hemobilia; and type 3 due to extraluminal tumor or nodal compression.
1,
4 Locations of biliary obstruction were classified according to the extent of tumor thrombi or obstruction. Location of obstruction was mainly diagnosed by ERCP. The locations of obstruction were divided into six groups: the type I location of obstruction was an obstruction of a unilateral intrahepatic duct (IHD) with a biliary tumor thrombi or tumor compression, without contralateral IHD involvement. The type II location of obstruction involved a unilateral IHD with hilar area involvement. Type III obstruction was defined by obstruction of a bilateral IHD with hilar involvement. Type IV obstruction involved only extrahepatic ducts (EHD). Type V location of biliary obstruction comprised multifocal involvement of both the IHD and EHD, and Type VI obstruction was defined as solitary hilar or common hepatic duct (CHD) involvement.
Endoscopic intervention was performed by insertion of a biliary plastic stent or metal stent, endoscopic nasobiliary drainage (ENBD), or sphincterotomy (EST) alone. The method of intervention was decided upon by the endoscopists at the time of intervention. We primarily tried to insert a biliary stent for treatment of HCC patients with obstructive jaundice. However, stent insertion was not available in some cases with severe bile duct stenosis, etc. In such cases, other endoscopic interventions, such as ENBD or EST, were selected.
Biliary stent insertion was performed with plastic or metal stents. Plastic stents showed relatively shorter patency than that of metal stents. Therefore, inoperable cancer patients with obstructive jaundice preferred to have metal stents inserted than plastic stents. In this study, although this result did not show statistical significance, metal stents were inserted in cases with intraluminal tumor infiltration. On the other hand, plastic stents tended to be used in patients with obstructive jaundice caused by hemobilia or extraluminal compression.
The patients were divided into two groups based on the success or failure to relieve obstructive jaundice. Clinical success was defined as a bilirubin level that decreased to normal bilirubin status or more than half the bilirubin level compared to that in the time of ERCP within 4 weeks after endoscopic intervention.
Statistical analysis
Continuous data were expressed as mean±SD or medians, and categorical data were expressed as the number of patients with a specified condition or clinical variable. The detection of significant differences was performed using Student's t-test for continuous variables and the chi-square test for categorical variables. Logistic regression was carried out via multivariate analysis. These tests were also used to determine whether each variable considered was a significant predictor of clinical outcomes (success or failure). For predicting clinical outcomes, a cut-off value for pre-endoscopic treatment total bilirubin level was determined using receiver operating characteristic (ROC) curves and area under the ROC curve analysis. Median overall survival was estimated using Kaplan-Meier analysis. All analyses were performed using SPSS software (ver. 12.0, Chicago, IL, USA). All p-values <0.05 were considered significant.
RESULTS
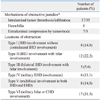
The clinical characteristics of the patients are summarized in
Table 1. Viral hepatitis B or C was the predominant underlying cause of liver disease (n=48, 88.9%), and most of the patients had cirrhosis (n=47, 87%). Hepatic function was evaluated with Child-Pugh classification and the numbers of patients with Child-Pugh class A, B, and C were 7 (13%), 21 (39%), and 26 (48%), respectively. At the time of ERCP, the mean total bilirubin was 15.5 mg/dL, mean serum alkaline phosphatase was 280.2 IU/L, and mean gamma-glutamyl transferase was 272.4 IU/L (
Table 1).
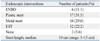
The mechanisms of obstructive jaundice, locations of biliary obstruction, and modalities of endoscopic interventions are summarized in
Table 2 and
3. The mechanisms of obstructive jaundices in HCC were as follows: intraluminal tumor thrombosis (n=17), cancer infiltration (n=35), hemobilia (n=6), compression by tumor mass (n=7) or lymph node (n=3), or a combination of the above. Among them, type 1 obstructive jaundice (intraluminal tumor obstruction) was most common. Each type of obstructive jaundice may have been combined with other types in some cases. For the location of obstructions, the most common level of biliary obstruction involved hilar lesions or common hepatic ducts (type VI). Endoscopic interventions included ENBD (n=6), plastic stent (n=17), metal stent (n=16), and EST (n=12). Stent insertion was preferentially considered in endoscopic intervention. However, stent could not be inserted in some cases. We tried to perform ENBD for cases that showed bile duct stricture caused by cancer, huge abscess, or ampullary adenoma.
Even less, ENBD insertion could not be possible in specific cases with bile duct stenosis by post-transcatheter arterial chemoembolization (TACE) glue damage or atrophy. Finally, EST was done in those cases.
Among the methods for relieving jaundice, the insertion of biliary stents, both metal and plastic, were most common (n=33, 61.1%). There were no severe procedure-related complications, such as perforation or death. Stent dysfunction developed in 8 patients during the follow-up period. Stent obstruction was observed in 4 patients caused by tumor growth and thrombi. These 4 patients were treated by stent changes in 2 cases, stent-in-stent insertion in 1 case, and stent dilatation by ballooning in 1 case. Stent migration occurred in 1 patient. The causes of stent dysfunction in the other 3 patients were biloma leakage, bleeding at previous endoscopic sphincteroscopy site, and infection due to huge abscess.
HCC is a hypervascular tumor; therefore, stent obstruction can easily be caused by intraluminal tumor thrombus or infiltration (type 1 obstructive jaundice). Three of 4 patients with stent obstruction showed type 1 obstructive jaundice due to intraluminal thrombus or tumor infiltration. The other one patient had type 3 jaundice (i.e., extraluminal lymph node compression). One patient with stent migration also showed type 1 jaundice.
There were no significant differences in age, sex, causes of hepatitis, the presence of cirrhosis, and treatment modalities of HCC between clinical success and failure groups. HCC patients that achieved clinical success were treated with TACE, chemotherapy, radiotherapy, or radiofrequency ablation.
The two groups did not differ in the mechanisms of obstructive jaundice, locations of biliary obstruction, and modalities of endoscopic interventions. However, mean total bilirubin was significantly higher (23.1±10.4 mg/dL vs. 8.1±5.3 mg/dL,
p≤0.001) and albumin was significantly lower (2.8±0.4 g/dL vs. 3.1±0.4 g/dL,
p=0.013) in clinical failure group than in the clinical success group. Furthermore, the cut-off value of pre-treatment total bilirubin level for predicting the clinical prognosis after endoscopic intervention was 12.8 mg/dL. The area under the ROC curve was 0.904 [95% confidence interval (CI), 0.819-0.989]. Sensitivity and specificity were 85.7% and 91.3%, respectively. Accordingly, patients with a bilirubin level below 12.8 mg/dL before endoscopic intervention should show better clinical outcomes. Also, the number of patients with better liver function was larger in the clinical success group (Child-Pugh grade A or B/C; 17/6 vs. 8/20,
p=0.001). Additionally, alcoholic patients with HCC compared to non-alcoholic patients were also higher in the clinical failure group (n=20 vs. n=9,
p=0.010) (
Table 4). We also analyzed predictive factors by multivariate analysis. The only influencing factor was total bilirubin level at the time of endoscopic intervention, regardless of history of alcohol consumption [odds ratio 1.223 (95% CI, 1.071-1.396),
p=0.003].
Trends in total bilirubin level for the two groups within 4 weeks after endoscopic intervention are shown in
Fig. 1. The median time from diagnosis of HCC to endoscopic intervention was 9.4 months. The median survival after endoscopic intervention was significantly longer in the clinical success group than in the clinical failure group (5.6 months vs. 1.5 months,
p≤0.001). The overall median survival time from diagnosis of HCC was 19.4 months (95% CI, 7.2-31.6 months). The median survival days from ERCP among patients in the clinical failure group was only 1.5 months; most of them experienced disease progression and decline in hepatic function.
DISCUSSION
Jaundice in HCC usually develops in later stages of the disease, and can be caused by diffuse cancer infiltration, invasion of the biliary ducts, progressive liver failure, and severe cirrhosis.
5 Among various causes of jaundice, obstructive jaundice caused by HCC is rare.
3 Obstructive jaundice in HCC was first reported in 1947 by Mallory, et al.
6 In that case, the obstructive jaundice was due to invasion by HCC of the cystic duct, followed by hemobilia from tumor thrombi.
As obstructive jaundice can be relieved by active intervention, unlike hepatocellular jaundice, it is clinically important to be aware that bile duct obstruction can be a cause of jaundice in HCC, and distinguishing obstructive jaundice from non-obstructive jaundice should be performed.
The goals of management in patients with HCC associated obstructive jaundice are biliary decompression, and, if possible, removal of tumor debris.
7 This can be done surgically or endoscopically. The choice of method is based on the nature and location of the main tumor mass, severity of the symptoms, associated neoplastic strictures, and the patient's overall status.
8 However, operative treatment is beneficial only in patients with extrahepatic intraluminal biliary obstruction.
9 Therefore, in patients with advanced diseases, endoscopic interventions might be safer and more satisfactory, as a form of palliative treatment.
7
Obstructive jaundice can be further specified according to the mechanisms and locations of obstruction. First, mechanisms of biliary obstruction in HCC were divided into three types by Lai and Lau
1 These types included tumor invasion of a branch of the biliary tree; distal migration to the common bile duct by necrotic free floating fragments that separate from a biliary tumor thrombus; and hemobilia caused by bleeding from a tumor that causes the bile duct to fill with blood clots that can obstruct bile duct system.
10,
11,
12 It is possible that the mechanisms of obstructive jaundice might affect the outcomes of endoscopic intervention. However, in our study, the mechanisms of biliary obstruction did not affect the results of intervention: we have to point out that there were multiple mechanisms for obstructive jaundice in HCC, and sometimes it is hard to say which mechanism was dominant.
One must also consider which endoscopic interventional method should be used. According to our results, stenting did not always seem to be the best interventional method in HCC. Some HCC patients with obstructive jaundice treated with stent insertion showed inadequate relief of jaundice according to their underlying hepatic function. Therefore, stenting may not be of help for some patients with poor liver function. In such cases, stent insertion is not the best treatment for relieving jaundice. Brown and Covey
13 suggested that stent placement is less effective in jaundice caused by intraductal tumor, because tumors can infiltrate into the stent, resulting in occlusion. Accordingly, we recommend choosing interventional methods on a case-by-case basis, taking into consideration the patient's clinical condition.
By considering predictive factors, patients who are more likely to benefit from endoscopic intervention may be selected. We found that the factors influencing successful endoscopic management include hepatic function at the time of the endoscopic procedure and a history of alcohol consumption. Furthermore, median survival after endoscopic intervention in the clinical success group was notably longer than that in the clinical failure group. This implies that the factors that predict the success of endoscopic management, defined here as a relief of obstruction, also can predict median survival after the procedure. Many physicians are reluctant to treat patients with HCC that have jaundice. However, in well selected cases, endoscopic intervention not only can resolve obstructive jaundice, but also prolong the survival of patients.
We concluded that endoscopic intervention can be an effective way to relieve obstructive jaundice in patients with HCC and can lead to the improvement of quality of life and even survival therein. Liver function and a history of alco-hol consumption should be checked to select patients most likely to benefit endoscopic interventions. Further prospective studies with larger population will be needed to objectively compare different methods of intervention. In the future, development of guidelines for endoscopic treatment in HCC patients with obstructive jaundice will be needed.







 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download