Abstract
Purpose
To investigate the clinical effects of a single high dose intravenous immunoglobulin (IVIG) combined with initial dexamethasone as a primary treatment on Kawasaki disease (KD).
Materials and Methods
Between January 2008 and December 2010, we reviewed the medical records of 216 patients with complete KD patients that were admitted to a single medical center. 106 patients were treated with a single high dose of IVIG (2 g/kg) alone and 110 patients received IVIG and dexamethasone (0.3 mg/kg per day for three days).
Results
The combined IVIG plus dexamethasone patient group had a significantly shorter febrile period and duration of hospital stay (1.4±0.7 days vs. 2.0±1.2 days, p<0.001; 5.8±1.7 days vs. 6.9±2.5 days, p<0.001, respectively) than the IVIG alone group. The combined IVIG plus dexamethasone group required IVIG retreatment significantly less than the IVIG only group (12.7% vs. 32%, p=0.003). After completion of the initial IVIG, C-reactive protein levels in the combined IVIG plus dexamethasone group were significantly lower than those in the IVIG only group (2.7±4.0 mg/dL vs. 4.6±8.7 mg/dL, p=0.03). In the combined IVIG plus dexamethasone group, the incidence of coronary artery lesions tended to be lower without worse outcomes at admission after initial infusion of IVIG and in follow-up at two months; however, the differences were not significant (8.2% vs. 11.3%, p=0.22; 0.9% vs. 2.8%, p=0.29).
Kawasaki disease (KD) is a form of acute vasculitis that occurs during childhood with clinical features of fever, rash, oral mucositis, conjunctival injection, change of extremities and cervical lymphadenopathy. As a serious complication in Kawasaki disease, coronary aneurymal alteration leads to acquired coronary heart disease in children. Coronary artery lesions (CAL) develop in approximately 15% to 25% of untreated cases and standard therapy with intravenous immunoglobulin (IVIG) has been reported to be effective in reducing the incidence of CAL in KD patients.1 However, 11% to 23% of KD patients still have a persistent fever or recurrent fever after completion of IVIG.2 These patients, who are non-responsive to the initial treatment regimen, are recommended a retreatment with IVIG and additional regimens, such as methylprednisolone pulse therapy, infliximab and cyclophosphamide.1,3,4,5,6
Since Kato, et al.6 reported that corticosteroids increase the risk of CAL, corticosteroid therapy for treatment of KD has been limited. Recently, steroid therapy with pulsed methylprednisolone was introduced to children whose fever is not alleviated despite more than two infusions of IVIG in refractory KD. Corticosteroids reduce fever and prevent the progression of coronary artery complications as a result of KD and suggest the possibility of a steroid regimen combined with IVIG as an initial therapy in KD.7,8,9 Dexamethasone with long-acting anti-inflammatory activity is more potent than methylprednisolone and is clinically used in pulsed steroid therapy. In a previous study, it improved pre-extubation pulmonary edema and cerebral vasogenic edema in brain tumor and meningitis.10 In vitro, it experimentally inhibits three relevant cell-types, monocytes, T lymphocytes, and human coronary arterial endothelial cells, all of which play a role in vasculitis and tissue edema, along with coronary complications, observed in KD patients.11 We studied the clinical effects of high-dose IVIG combined with initial dexamethasone as a primary treatment for KD.
From January 2008 to December 2010, we enrolled patients at Ajou University Hospital. We retrospectively reviewed the medical records and laboratory data of KD patients. KD was diagnosed according to the criteria as defined by the American Heart Association. All patients exhibited at least five of the following features: fever lasting longer than 5 days (axillary or ear temperature exceeding 38.0℃); non-exudative conjunctival injection; changes in the oropharynx, including mucosal erythema, dry cracked red lips, and strawberry tongue; changes in the extremities, including palmar and plantar erythema, edema of the hands and feet, and periungual desquamation; generalized polymorphorous rash; and cervical lymphadenopathy.1 The duration of fever was significantly related to increased risk and progression of CAL. Exclusion criteria included a previous diagnosis of KD, presence of a previous CAL, incomplete KD with fewer than four features of KD, and initial consultation after a febrile duration longer than 10 days, as these conditions may have an effect on clinical results and CAL outcomes. This study was approved by the Institutional Review Board of Ajou University Hospital.
One hundred and ten patients out of 216 patients were treated intravenously with 0.3 mg/kg of dexamethasone per day (0.1 mg/kg, 3 times a day) for three consecutive days, beginning on the same day as the initial IVIG infusion (2 g/kg) as a primary treatment of acute KD, and comprised the combined IVIG plus dexamethasone (IVIG+DEX) group. The 0.3 mg/kg per day dose of dexamethasone used in this study has equivalent anti-inflammatory potency to 2 mg/kg per day of prednisolone used in a previous study.9,10 Additionally, oral acetylsalicylic acid (80 mg/kg per day) was started together with IVIG and dexamethasone. A group of 106 control KD patients received standard therapy with a single high-dose infusion of IVIG (2 g/kg) only plus oral aspirin (80 mg/kg per day). Non-responsiveness to initial therapy is defined as persistent or recrudescent fever longer than 48 hours after completion of the initial IVIG infusion. Non-responsive patients received an additional IVIG (1 g/kg/dose, 1-2 doses) with oral aspirin. Laboratory investigations were performed at admission before treatment and at 1 week after initial IVIG infusion, as well as at 2 weeks and 2 months later in two groups. CAL was defined when the luminal diameter exceeded 3.0 mm in a child under the age of 5 years or 4.0 mm in a child aged 5 years or older, when the internal diameter of a segment was at least 1.5 times that of an adjacent segment, or when the luminal contour was clearly irregular.1 A two-dimensional echocardiogram was conducted 2 days after completion of the initial IVIG therapy and again at 2 weeks and 2 months thereafter. The examination of the adverse effects of dexamethasone in the IVIG plus DEX group were examined with blood pressure and an echocardiogram for the analysis of thrombosis or ectasia in the coronary arteries.
The results are presented as mean±standard deviation. For comparison of the two groups, the numeric values were analyzed using the independent samples t-test for unpaired values. Categorical data were assessed by the chi-squared test. A p value <0.05 was considered statistically significant. The statistical analyses were conducted using the SPSS statistical package, version 12.0 (SPSS Inc., Chicago, IL, USA).
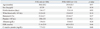
The demographic and laboratory data for both the experimental and control groups before treatment are summarized in Table 1. There were no significant differences in age (30.6±20.2 months vs. 29.9±20.5 months, mean±standard deviation; p=0.97 by the t-test), sex distribution (boy/girl, 67/39 vs. 72/39; p=0.54 by the chi-squared test) and febrile duration on admission (5.4±1.7 days vs. 5.3±1.0 days, mean±SD; p=0.95 by the t-test) between the control IVIG only group and the IVIG plus DEX groups. The groups were well balanced with respect to demographic and clinical characteristics. The laboratory data of the two groups on admission were not significantly different with regards to white blood cell counts, hematocrit, platelet counts, albumin, erythrocyte sedimentation rate, and C-reactive protein (Table 1). All patients were monitored for at least two months (range, 2 to 38 months). No serious adverse effects such as hypertension or thromboses were reported in any of the KD patients, including those in the IVIG plus DEX group.
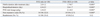
The average febrile duration after the initial treatment in the IVIG plus DEX group was significantly shorter than that in the IVIG only group (1.7±0.7 vs. 2.0±1.2, mean±SD; p<0.001 by the t-test). The mean duration of hospital stay in the IVIG plus DEX group was also significantly shorter than that in the IVIG only group (5.8±1.7 days vs. 6.9±2.5 days, mean±SD; p<0.001). The mean total dosage of IVIG on admission in the IVIG plus DEX group was remarkably lower than that in the IVIG only group (2.1±0.3 g/kg vs. 2.4±0.5 g/kg, mean±SD; p<0.001). Non-responsive rate to the initial therapy was 22.2% (48/216) for the entire patient population; 14 patients were in the IVIG plus DEX group and 34 patients belonged to the IVIG only group. The percentage of non-responsive patients was lower in the IVIG+DEX group than that in the IVIG only group (12.7% vs. 32%; p=0.003 by the chi-squared test). Patients in the IVIG plus DEX group showed more rapid clinical improvement and required less immunoglobulin treatment. Some patients after initial therapy were readmitted for recurrent fever and other features consistent with KD. The rate of readmission in the IVIG plus DEX group was lower than that in the IVIG only group; however, the difference was not significant (5.4% vs. 10.4%; p=0.12 by the chi-squared test) (Table 2).
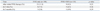
On the serial echocardiograms after treatment, the incidence of CAL in the IVIG plus DEX group was less frequent than the control group 2 days after completion of initial IVIG therapy, at two weeks, and at two months (8.2% vs. 11.3%, p=0.22; 4.5% vs. 7.5%, p=0.26; 0.9% vs. 2.8%, p=0.29) (Table 3). These differences were not significant between the two groups. Most findings regarding CAL improved at two months after the initial treatment, and persistent CAL was infrequent as it was observed in only 4 patients (4/216, 1.9%) in our study. There was no giant coronary aneurysm defined as an internal diameter >8 mm. CAL of one patient in the IVIG plus DEX group presented with a dilatation of the left coronary artery (diameter 6 mm). Three patients in the IVIG only group had a medium to large sized dilatation of the right and left coronary arteries (each diameter 4.3 mm, 5 mm, 7 mm). CAL in two patients with diameters of 4.3 mm and 5 mm, regressed within 18 months of illness. The absolute number of CAL's reported for the IVIG plus DEX group was less than that reported in the control group. An annual echocardiogram was conducted for patients with large aneurysms without development of CAL. None of the patients had adverse effects with regards to thrombosis in the coronary artery on echocardiogram. For the non-responsive cases, the incidence of CAL was not different between the two groups, however, each group had only a small number of cases, 1 case in the IVIG plus DEX group and 2 cases in the IVIG only group.
After completion of the initial IVIG treatment, the average level of C-reactive protein (CRP) in the IVIG plus DEX group was significantly lower than that in the IVIG only group (2.7±0.04 mg/dL vs. 4.6±0.06 mg/dL, mean±standard error; p=0.03). The magnitude of decrease in the CRP levels in the IVIG plus DEX group was larger than that in the IVIG only group at 1 week after completion of the initial IVIG. Both of the mean CRP levels decreased to the same level as the normal range observed at two months (Fig. 1A). The serial platelet count in the IVIG plus DEX group was elevated early and decreased to levels lower than those obtained for the IVIG only group. The platelet counts at two weeks and two months were decreased significantly more in the IVIG plus DEX group than those in the IVIG only group (435±13.8 ×103/uL vs. 517±14.8 ×103/uL, mean±SE; p<0.001, 322±6.9 ×103/uL vs. 361±8.5 ×103/uL, mean±SE; p<0.001) (Fig. 1B). At two months, the mean erythrocyte sedimentation rate (ESR) in the IVIG plus DEX group also decreased significantly, compared to the IVIG only group (6.7±0.7 mm/hr, vs. 9.6±1.2 mm/hr, mean±SE; p=0.04) (Fig. 1C). Also, in non-responsive patients, platelet counts at 2 months in the IVIG plus DEX groups were significantly lower than those in the IVIG only group (316±81 ×103/uL vs. 369±80 ×103/uL, mean±SD; p=0.04). ESR in the IVIG plus DEX group was also lower significantly than that in the IVIG only group (5.0±3.7 mm/hr vs. 11.6±1.4 mm/hr, mean±SD; p=0.02) for non-responsive patients.
Standard therapy with IVIG and aspirin for the treatment of KD has significantly reduced the incidence of coronary artery abnormalities since Furusho, et al.12 reported the beneficial effects of high-dose IVIG treatment for KD. Nonetheless, when a high-dose of IVIG is administered, approxima-tely 5% of children with KD experience transient coronary artery dilatation and 1% of them develop large aneurysms. Approximately 15% of KD patients exhibit persistent or recurrent fever after IVIG completion, which puts then at an increased risk of CAL.13,14,15 Recent studies have recommended novel treatments for non-responsive patients including repeated doses of IVIG, intravenous pulse methylprednisolone, plasma exchange, ulinastatin, abciximab, infliximab, and cyclosphamide.1,16,17 However, the effectiveness and adverse potentially adverse effects of several of these treatment options are uncertain due to the limited number of participants in the studies.
Corticosteroids are a strong anti-inflammatory agent used for the treatment of vasculitis, and have been mentioned to be of potential use in treatment of KD by many clinicians including Dr. Kawasaki. Before the first report of IVIG efficacy in KD, corticosteroid therapy was used as the initial treatment for KD. There were several reports regarding the use of corticosteroids in KD due to its potential to ameliorate blood vessel damage by suppressing inflammatory effectors that lead to endothelial cell injury and weakening of the vessel wall.18,19 Nevertheless, in the pre-IVIG era, many clinicians thought that steroid therapy might be harmful, as steroid might cause coronary thrombosis and aneurismal change in KD. An early study by Kato, et al.6 suggested a high incidence of coronary artery aneurysms in KD patients treated with prednisolone alone (11 of 17 patients), and as a result, steroids were thought to be harmful. In the post-IVIG era, corticosteroid therapy was used with or after the additional IVIG regimen as a rescue therapy in refractory KD. The pulsed steroid therapy in KD patients who presented with recrudescent fever was associated with an improvement of fever and CAL progression. In the study by Dahlem, et al.20 pulsed intravenous methylprednisolone was effective in relieving persistent fever and large pericardial effusions unresponsive to multiple treatments with IVIG. Additionally, Dale, et al.21 reported that oral prednisolone (2 mg/kg/day, for 14 days) and aspirin were effective for severe complications in KD patients treated with initial IVIG therapy (2 g/kg). Previously, Hashino, et al.5 demonstrated the efficacy and safety of additional pulsed steroid therapy after multiple IVIG infusions in shortening febrile duration and lowering medical costs. As well, Wright, et al.3 reported the effectiveness of intravenous pulse methylprednisolone as a rescue therapy for non-responsive KD patients in comparison to standard IVIG therapy. The results from recent research have led to recommendations of an additional steroid regimen of intravenous pulse methylprednisolone (30 mg/kg/day, for 3 days) for KD patients, as additional infusions with IVIG have proven ineffective in relieving persistent fever and acute inflammation.3,5
The steroid treatment combined with IVIG was introduced recently as a primary therapy for KD. Shinohara, et al.22 reported that a regimen of prednisolone and immunoglobulin (200-400 mg/kg/d for 5 days) with aspirin is associated with shorter febrile duration and a decreased incidence of CAL when used as a primary therapy for acute KD. Sundel, et al.9 suggested that the initial methylprednisolone therapy with IVIG as a primary therapy in KD led to faster resolution of fever, rapid improvement in inflammatory markers, and shorter length of hospitalization. Laboratory measurements, such as serum CRP, and clinical markers of the disease, such as a febrile duration, also improved more quickly in patients treated with IVIG and corticosteroids than those treated with IVIG alone.23,24 In a meta-analysis by Wooditch and Aronoff25 eight studies encompassing 862 children with KD in whom combined corticosteroid therapy with aspirin and IVIG were the initial treatment, were assessed. This form of initial treatment significantly reduced the incidence of coronary artery aneurysms. In sequential studies of oral prednisolone plus IVIG therapy as a primary regimen in KD patients, Inoue, et al.26 reported that this treatment regimen improved the overall clinical course and outcomes of CAL without any adverse effects in acute KD. However, the rate of recurrence in the group treated with a combination of oral prednisolone plus IVIG was increased compared to the standard IVIG treated group (4.4% vs. 2.2%, p=0.682). In another study of a large number of KD patients [IVIG group (n=896) and IVIG plus prednisolone group (n=110)], the IVIG plus prednisolone treatment was associated with improved clinical and coronary outcomes in patients at a high risk of failure to respond to the IVIG treatment.24
Dexamethasone, as a fluoridated glucocorticoid, has been clinically used for pulse steroid therapy with favorable results. It is a long acting drug, with a half-life of 36-72 hours, and exerts negligible mineralocorticoid effects, almost without salt retention. Compared to methylprednisolone, used pulse steroid regimen, dexamethasone is less expensive and 6.7 times more potent with small equipotent volume.27,28 Dexamethasone lowers primarily vasogenic edema in brain tumors and meningitis by decreasing the capillary permeability of the blood brain barrier.10 With regards to the pathogenesis of KD, vascular leakage with systemic edema is an important pathologic finding in severe KD. The corticosteroid dexamethasone attenuates the cytokine reactions that play a role in the pathogenesis of KD.23 Patients with CAL were found to have increased levels of cytokines, compared to those with normal coronary arteries.23 These cytokines may mediate vascular damage and lead to CAL in KD.29 In an experimental study, high-dose IVIG inhibited the activation of monocytes, macrophages, and coronary arterial endothelial cells, whereas dexamethasone inhibited these cells, in addition to T cells, in vitro.11 Jibiki, et al.8 introduced a combined regimen of intravenous dexamethasone with heparin and multiple infusions of IVIG (400 mg/kg/day for five days) for primary therapy in KD. The combined dexamethasone and IVIG were safe and accelerated the resolution of systemic inflammation. In our study, the group treated with a combination of dexamethasone and a single high-dose infusion of IVIG (2 g/kg) demonstrated a more favorable clinical course with decreased febrile duration and length of hospital stay. The combined dexamethasone therapy decreased the need for additional IVIG treatments and lowered non-responsive rates to initial treatment. These results were supported by serial results of clinical inflammatory markers, such as CRP and ESR. The levels for both CRP and ESR decreased more sharply and normalized faster in the combination therapy group than the IVIG only group. In regards to coronary outcomes, CALs were not worse in the combined therapy group than the IVIG only group. Our results on coronary outcomes are in direct contrast to the pre-IVIG era reports of increased risks of coronary aneurysm in KD patients treated with corticosteroid.
Our study had a few limitations including small number of patients in the combined dexamethasone and IVIG group that did not show better coronary outcomes. Recent trends regarding treatment choices for patients that do not respond to IVIG treatment for KD have included additional infusions of one or two more doses of IVIG, secondary pulsed steroid therapy with intravenous methylprednisolone 30 mg/kg/day for three days, and finally treatment with a tumor necrotizing factor-α blocker, such as infliximab. However, the therapeutic superiority thereof has been not been proven.30 Although the number of cases was very small, there were fewer non-responsive cases in the combined dexamethasone therapy than in the IVIG only group. Nevertheless, our results suggest combined dexamethasone therapy may decrease fever sooner and require less additional therapy such as infliximab whose effects on refractory KD still remain uncertain. As another limitation of our study, the levels of selected cytokines were not analyzed in relation to the combined steroid therapy in KD. We suggest that levels of inflammatory cytokines could support the efficacy of the combined steroid therapy. Further studies with a large number of patients will be required to definitively demonstrate the effectiveness of combined dexamethasone as an initial therapy in KD.
Figures and Tables
 | Fig. 1Changes in laboratory findings between the IVIG only group and IVIG plus dexamethasone group (DEX+IVIG): (A) for mean C-reactive protein (CRP), (B) for mean platelet count, and (C) for mean erythrocyte sedimentation rate (ESR). *p<0.05, IVIG only group vs. DEX+IVIG group. DEX, dexamethasone; IVIG, intravenous immunoglobulin. |
References
1. Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, American Heart Association. Pediatrics. 2004; 114:1708–1733.

2. Han RK, Silverman ED, Newman A, McCrindle BW. Management and outcome of persistent or recurrent fever after initial intravenous gamma globulin therapy in acute Kawasaki disease. Arch Pediatr Adolesc Med. 2000; 154:694–699.

3. Wright DA, Newburger JW, Baker A, Sundel RP. Treatment of immune globulin-resistant Kawasaki disease with pulsed doses of corticosteroids. J Pediatr. 1996; 128:146–149.

4. Blaisdell LL, Hayman JA, Moran AM. Infliximab treatment for pediatric refractory Kawasaki disease. Pediatr Cardiol. 2011; 32:1023–1027.

5. Hashino K, Ishii M, Iemura M, Akagi T, Kato H. Re-treatment for immune globulin-resistant Kawasaki disease: a comparative study of additional immune globulin and steroid pulse therapy. Pediatr Int. 2001; 43:211–217.

6. Kato H, Koike S, Yokoyama T. Kawasaki disease: effect of treatment on coronary artery involvement. Pediatrics. 1979; 63:175–179.

7. Kijima Y, Kamiya T, Suzuki A, Hirose O, Manabe H. A trial procedure to prevent aneurysm formation of the coronary arteries by steroid pulse therapy in Kawasaki disease. Jpn Circ J. 1982; 46:1239–1242.

8. Jibiki T, Terai M, Kurosaki T, Nakajima H, Suzuki K, Inomata H, et al. Efficacy of intravenous immune globulin therapy combined with dexamethasone for the initial treatment of acute Kawasaki disease. Eur J Pediatr. 2004; 163:229–233.

9. Sundel RP, Baker AL, Fulton DR, Newburger JW. Corticosteroids in the initial treatment of Kawasaki disease: report of a randomized trial. J Pediatr. 2003; 142:611–616.

10. Rosenberg GA. Brain Edema and Disorders of Cerebrospinal Fluid Circulation. In : Bradley WG, Daroff RB, Fenichel GM, Jankovic J, editors. Neurology in Clinical Practice. 2nd ed. Boston: Butterworth-Heinemann Limited;2000. p. 1545–1549.
11. Makata H, Ichiyama T, Uchi R, Takekawa T, Matsubara T, Furukawa S. Anti-inflammatory effect of intravenous immunoglobulin in comparison with dexamethasone in vitro: implication for treatment of Kawasaki disease. Naunyn Schmiedebergs Arch Pharmacol. 2006; 373:325–332.

12. Furusho K, Kamiya T, Nakano H, Kiyosawa N, Shinomiya K, Hayashidera T, et al. High-dose intravenous gammaglobulin for Kawasaki disease. Lancet. 1984; 2:1055–1058.

13. Dajani AS, Taubert KA, Gerber MA, Shulman ST, Ferrieri P, Freed M, et al. Diagnosis and therapy of Kawasaki disease in children. Circulation. 1993; 87:1776–1780.

14. Newburger JW, Takahashi M, Beiser AS, Burns JC, Bastian J, Chung KJ, et al. A single intravenous infusion of gamma globulin as compared with four infusions in the treatment of acute Kawasaki syndrome. N Engl J Med. 1991; 324:1633–1639.

15. Sato N, Sugimura T, Akagi T, Yamakawa R, Hashino K, Eto G, et al. Selective high dose gamma-globulin treatment in Kawasaki disease: assessment of clinical aspects and cost effectiveness. Pediatr Int. 1999; 41:1–7.

16. Weiss JE, Eberhard BA, Chowdhury D, Gottlieb BS. Infliximab as a novel therapy for refractory Kawasaki disease. J Rheumatol. 2004; 31:808–810.
17. Furukawa T, Kishiro M, Akimoto K, Nagata S, Shimizu T, Yamashiro Y. Effects of steroid pulse therapy on immunoglobulin-resistant Kawasaki disease. Arch Dis Child. 2008; 93:142–146.

18. Burns JC. Revisiting steroids in the primary treatment of acute Kawasaki disease. J Pediatr. 2006; 149:291–292.

19. Shulman ST. Is there a role for corticosteroids in Kawasaki disease? J Pediatr. 2003; 142:601–603.

20. Dahlem PG, von Rosenstiel IA, Lam J, Kuijpers TW. Pulse methylprednisolone therapy for impending cardiac tamponade in immunoglobulin-resistant Kawasaki disease. Intensive Care Med. 1999; 25:1137–1139.

21. Dale RC, Saleem MA, Daw S, Dillon MJ. Treatment of severe complicated Kawasaki disease with oral prednisolone and aspirin. J Pediatr. 2000; 137:723–726.

22. Shinohara M, Sone K, Tomomasa T, Morikawa A. Corticosteroids in the treatment of the acute phase of Kawasaki disease. J Pediatr. 1999; 135:465–469.

23. Okada Y, Shinohara M, Kobayashi T, Inoue Y, Tomomasa T, Kobayashi T, et al. Effect of corticosteroids in addition to intravenous gamma globulin therapy on serum cytokine levels in the acute phase of Kawasaki disease in children. J Pediatr. 2003; 143:363–367.

24. Kobayashi T, Inoue Y, Otani T, Morikawa A, Kobayashi T, Takeuchi K, et al. Risk stratification in the decision to include prednisolone with intravenous immunoglobulin in primary therapy of Kawasaki disease. Pediatr Infect Dis J. 2009; 28:498–502.

25. Wooditch AC, Aronoff SC. Effect of initial corticosteroid therapy on coronary artery aneurysm formation in Kawasaki disease: a meta-analysis of 862 children. Pediatrics. 2005; 116:989–995.

26. Inoue Y, Okada Y, Shinohara M, Kobayashi T, Kobayashi T, Tomomasa T, et al. A multicenter prospective randomized trial of corticosteroids in primary therapy for Kawasaki disease: clinical course and coronary artery outcome. J Pediatr. 2006; 149:336–341.

28. Schimmer BP, Parker KL. Adrenocorticotropic hormones; adrenocortical steroids and their synthetic analog; inhibitors of the synthesis and actions of adrenocortical hormone. In : Brunton L, Lazo J, Parker K, editors. Goodman & Gilman's The Pharmacological Basis of Therapeutics. 11th ed. New York: McGraw-Hill Professional;2006. p. 1587–1612.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download