Abstract
Purpose
Assessing the immunogenicity of a single dose of hepatitis A virus (HAV) vaccines is important because some people receive only a single dose. However, previous studies have shown variable results and have not examined the effects of demographic characteristics other than gender. This study was performed to examine the immunogenicity of a single dose of HAV vaccine according to the vaccine type and demographic characteristics in young adults.
Materials and Methods
Seronegative medical school students were randomly allocated to receive either Havrix or Epaxal.
Results
After approximately 11 months, the seroconversion rate in 451 participants was 80.7%. In men, the Havrix group showed a significantly higher seroconversion rate (81.9%) than the Epaxal group (69.2%), whereas both vaccine groups showed similarly high immunogenicity in women (Havrix: 90.1%, Epaxal: 92.9%; P for interaction=0.062). According to the results of a multivariate analysis, Epaxal showed significantly lower immunogenicity than Havrix only in men. Age, obesity, drinking, smoking, and follow-up time did not significantly affect seroconversion in either gender.
Recently, hepatitis A virus (HAV) infection has become an important public health problem in countries such as Korea that have seen improvements in their socioeconomic status.1 The HAV vaccine is recognized as the most effective method for controlling HAV infection, and 2 doses of the HAV vaccine have been recommended 6-18 months apart.2 The high, long-term immune response acquired after 2 doses of HAV vaccine has been consistently reported.3-5 However, many travelers and some people at high risk receive only a single dose of the vaccine without a booster.6 Information from the physician on the immunogenicity of a single dose of the HAV vaccine to the patient receiving his/her first dose is helpful for encouraging booster vaccination. However, various seroconversion rates, ranging from approximately 80% to 100% at 12 months after the first dose in adults have been reported previously.7-10 In addition, the effects of demographic characteristics other than gender on HAV immunogenicity have not been examined.
This study was carried out to examine the immunogenicity of a single dose of HAV vaccines according to the vaccine type (Havrix or Epaxal) and demographic characteristics of Korean young adults who constitute a high-risk group for HAV infection.
Two types of inactivated HAV vaccines (Havrix and Epaxal) were used. Havrix is one of the several aluminum-absorbed vaccines, whereas Epaxal is the only aluminum-free virosomal HAV vaccine available.8 Havrix contains 1440 ELISA units of antigenic strain HM175 adsorbed to an aluminum hydroxide adjuvant.5 Epaxal contains more than 12 IU of antigenic strain RG-SB that is attached to the surface of the influenza virosome.8 All vaccines were purchased at the local pharmacy, stored at 2-8℃, and injected intramuscularly into the deltoid muscle of the participants.
Study population was freshman or sophomore students of the 8 medical schools which were located in the cities across the nation-2 schools at Daejeon and 1 school each at Daegu, Wonju, Iksan, Cheonan, Gangneung, and Busan. Among the 726 students of the target population, 582 (80.2%) agreed to participate in the study. They were serologically tested for the HAV antibody and asked to fill out the questionnaire to provide information about demographic characteristics and previous vaccination history. After excluding those participants who were seropositive for HAV (anti-HAV antibody level ≥20 IU/mL, n=77) or were previously immunized with an HAV vaccine (n=62), 483 of the 582 participants were randomly allocated to receive a single dose of either Havrix or Epaxal. The vaccinees were followed up for 7-12 months, and the median follow-up period was 11 months.
Approximately 11 months after the primary dose, blood samples from 454 out of 483 participants (94.0%) could be collected for the measurement of serum anti-HAV antibody titers. After excluding 3 participants who were independently vaccinated with a secondary dose, a total of 451 participants were included in the data analysis.
Among the 483 vaccinees, 29 (6.0%) dropped out of the study. Fifteen of these participants were vaccinated with Havrix and 14 were vaccinated with Epaxal. Mean age and age range of the 19 non-respondents were similar (19.9 and 18-23 years, respectively) to that of the 451 respondents (19.3 and 17-23 years, respectively). The proportion of men among the non-respondents (82.8%) was higher than that among the respondents (66.5%).
Total serum anti-HAV antibody titers were analyzed by chemiluminescent immunoassay using the ADVIA centaur (Siemens; Munich, Germany) at enrollment and the follow-up examination. Because the equipment was fixed with 20 IU/mL as a cutoff value, we considered an anti-HAV antibody titer lower than 20 IU/mL as seronegative. Previous studies have set 10 or 20 IU/mL as the cutoff value.7-11
We categorized obesity status according to the participants' body mass index (BMI), as defined by the International Obesity Task Force for Asian adults12: underweight, BMI <18.5 kg/m2; normal weight, BMI ≥18.5 kg/m2 and <23 kg/m2; overweight, BMI ≥23 kg/m2 and <25 kg/m2; and obese, BMI ≥25 kg/m2. We measured the degree of alcohol use according to the Alcohol Use Disorders Identification Test (AUDIT)-K, which is the Korean version of the test. We categorized the grade of alcohol use based on the participants' AUDIT-K scores, as recommended by the World Health Organization: low, AUDIT-K score 0-7; medium, AUDIT-K score 8-15; high, AUDIT-K score 16-19; and very high, AUDIT-K score 20-40.13 For analysis, we established none or low-grade alcohol use group by combining nondrinkers and drinkers with a low grade of alcohol use.
Differences in the seroconversion rates between the groups were tested using the chi-square test, and trends were analyzed using the chi-square test for trend. Multiple analysis using logistic regression was performed to evaluate the factors affecting seroconversion.
The Institutional Review Boards of the 8 participating medical schools approved the study protocol. Written informed consent was obtained from every participant. This study was designed and executed independently of the vaccine manufacturers.
All results were obtained from the data on the 451 participants who were followed up and not independently vaccinated with a secondary dose. Most participants were 17-22 years of age (98.7%); male (66.5%); of normal weight (65.2%); nonsmokers (93.1%); and none, low-, or medium-grade alcohol users (83.2%). A total of 225 and 226 participants were administered Havrix and Epaxal, respectively, and half of the participants (48.3%) were followed-up for 7-10 months after the vaccination. Approximately 11 months after the single-dose vaccination, the overall seroconversion rate was 80.7%. Among the demographic and vaccine-related factors, gender, obesity, grade of alcohol use, and vaccine type were found to significantly affect the seroconversion rate. Women (91.4%) and participants in the Havrix group (84.9%) showed higher seroconversion rates than men (75.3%) and those in the Epaxal group (76.6%), respectively. As the grade of obesity and alcohol use increased, the seroconversion rates diminished (Table 1).
We examined whether interactions existed between covariates by using multiple analysis in which age, gender, obesity, drinking, smoking, vaccine type, and follow-up time were covariates, and found an interaction of borderline significance (p=0.062) only between the gender and vaccine type. Men in the Havrix group showed a significantly higher seroconversion rate (81.9%) than those in the Epaxal group (69.2%). However, women in both vaccine groups showed similarly high seroconversion rates (Havrix: 90.1%, Epaxal: 92.9%). Men showed lower seroconversion rates than women for both vaccines, but the gender-related difference was statistically significant only for the Epaxal group (Fig. 1).
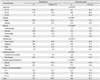
Based on these results, multiple analysis including age, obesity, drinking, smoking, vaccine type, and follow-up time as covariates was performed again after stratification with gender. Epaxal showed significantly lower immunogenicity than Havrix only in men. Age, obesity, drinking, smoking, and follow-up time did not significantly affect the HAV seroconversion (Table 2).
Using a conservative total serum anti-HAV antibody titer cutoff value of 20 IU/mL, the seroconversion rate of young adults in this study was only 80.7% approximately 11 months after single-dose HAV vaccination. This result is consistent with those of 3 previous studies that also used 20 IU/mL as the cutoff value and showed seroconversion rates, ranging from nearly 80% to 99% at 12 months after single-dose HAV vaccination in adults.7,10,11 These results indicate the need for two-dose HAV vaccination not only for long-term maintenance but also for the acquisition of the seroprotection.
In the present study, men showed lower seroconversion rates than women for both vaccines. This result is consistent with the findings from previous Havrix and Epaxal studies.6,7,9-11,14 This gender-related difference in immunogenicity may have resulted from the confounding effect of body weight.10 In addition, a study that examined the effect of body weight without considering gender shows that higher body weight or BMI is associated with lower immunogenicity in adults.15 However, our study which is the first to concurrently examine the effects of both gender and BMI showed that only gender was associated with immunogenicity.
Importantly, Epaxal showed particularly low immunogenicity only in men in our study (p value for interaction between gender and vaccine type=0.062). A previous study that concurrently examined the immunogenicity of 2 vaccines reported that both men and Epaxal were associated with lower immunogenicity without interaction.10 Given that the interaction observed with our data has never been reported before, further evaluations are needed. If Epaxal consistently shows lower immunogenicity, particularly in men in future studies, Havrix rather than Epaxal should be recommended for male subjects.
Low immunogenicity has been found to be associated with older age, male gender, smoking, obesity, and alcohol abuse for hepatitis B virus vaccines.16 However, with the exception of gender, the association of demographic characteristics with HAV vaccine immunogenicity has not been studied. In the present study, age, obesity, drinking, and smoking did not significantly affect HAV seroconversion, as shown by multiple analysis. However, the significance of older age (23-28 years) and very high-grade alcohol use could not be determined because of the small sample sizes of the subgroups. In Korea, young adults are the main recipients of HAV vaccines to prevent HAV outbreak, and they are also the most vulnerable to alcohol abuse.17 Therefore, further evaluation of the association between alcohol use and HAV immunogenicity is needed.
In the present study, 6.0% (n=29) of participants dropped out of the study approximately 11 months after vaccination. The distribution for age was similar in participants who were followed up. However, the proportion of men in the non-respondents (82.8%) was higher than that in the respondents (66.5%). Since the men showed a lower seroconversion rate than women in this study, the seroconversion rate of all the participants would have been lower than the result obtained (80.7%), if the 29 participants who dropped out after vaccination were also followed up. However, we think that participants who dropped out may not have had a significant effect on the total seroconversion rate because the proportion of dropout was low (6.0%). Additionally, we think that the dropout would not have diminished the internal validity of the findings regarding the association of seroconversion with vaccine type and demographic characteristics, which is the main result of our study.
In summary, the seroconversion rate was found to be only 80.7% in young adults, approximately 11 months after single-dose HAV vaccination; this rate was particularly low in men who were administered Epaxal. Therefore, when evaluating the immunogenicity of HAV vaccines, the demographic characteristics of the participants need to be considered. In particular, studies comparing the immunogenicity of different vaccines should control the gender effect by sampling or statistical adjustment. In addition, further studies with various settings are needed to confirm whether the interaction between vaccine type and gender is consistent.
Figures and Tables
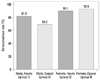 | Fig. 1Effect of gender and vaccine type on seroconversion rates. p value for the difference between groups 1 and 2=0.012, p value for the difference between groups 3 and 4=0.552, p value for the difference between groups 1 and 3=0.105, p value for the difference between groups 2 and 4 <0.001, and p value for the interaction between gender and vaccine type adjusted by age, gender, obesity, drinking, smoking, vaccine type, and follow-up time=0.062. |
Table 2
Multiple Logistic Regression Analysis* for the Characteristics of Participants and Seroconversion Rates Stratified by Gender

CI, confidence interval; N, number of participants; n/a, not applicable.
*Multiple logistic regression model including age, obesity, drinking, smoking, vaccine type, and follow-up time as covariates.
†The odds ratio (OR) is undefined because there was no seronegative participant in the relevant subgroups.
‡This analysis is not applicable because none of the female participants were smokers.
ACKNOWLEDGEMENTS
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2011-0025889).
Notes
References
1. Lee D, Cho YA, Park Y, Hwang JH, Kim JW, Kim NY, et al. Hepatitis a in Korea: epidemiological shift and call for vaccine strategy. Intervirology. 2008; 51:70–74.

2. WHO position paper on hepatitis A vaccines-June 2012. Wkly Epidemiol Rec. 2012; 87:261–276.
3. Hammitt LL, Bulkow L, Hennessy TW, Zanis C, Snowball M, Williams JL, et al. Persistence of antibody to hepatitis A virus 10 years after vaccination among children and adults. J Infect Dis. 2008; 198:1776–1782.

4. López EL, Contrini MM, Mistchenko A, Debbag R. Long-term immunity after two doses of inactivated hepatitis A vaccine, in Argentinean children. Pediatr Infect Dis J. 2010; 29:568–570.

5. Van Herck K, Jacquet JM, Van Damme P. Antibody persistence and immune memory in healthy adults following vaccination with a two-dose inactivated hepatitis A vaccine: long-term follow-up at 15 years. J Med Virol. 2011; 83:1885–1891.

6. Landry P, Tremblay S, Darioli R, Genton B. Inactivated hepatitis A vaccine booster given >/=24 months after the primary dose. Vaccine. 2000; 19:399–402.

7. D'Acremont V, Herzog C, Genton B. Immunogenicity and safety of a virosomal hepatitis A vaccine (Epaxal) in the elderly. J Travel Med. 2006; 13:78–83.
8. Bovier PA, Farinelli T, Loutan L. Interchangeability and tolerability of a virosomal and an aluminum-adsorbed hepatitis A vaccine. Vaccine. 2005; 23:2424–2429.

9. Ambrosch F, Finkel B, Herzog C, Koren A, Kollaritsch H. Rapid antibody response after vaccination with a virosomal hepatitis a vaccine. Infection. 2004; 32:149–152.

10. Holzer BR, Hatz C, Schmidt-Sissolak D, Glück R, Althaus B, Egger M. Immunogenicity and adverse effects of inactivated virosome versus alum-adsorbed hepatitis A vaccine: a randomized controlled trial. Vaccine. 1996; 14:982–986.

11. Bovier PA, Althaus B, Glueck R, Chippaux A, Loutan L. Tolerance and immunogenicity of the simultaneous administration of virosome hepatitis A and yellow fever vaccines. J Travel Med. 1999; 6:228–233.

12. Force IOT. The Asia-Pacific perspective: Redefining obesity and its treatment IOTF, Health Communications Australia Pty Ltd. Brisbane: World Health Organization/International Association for the Study of Obesity;2000.
13. Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT: The Alcohol Use Disorders Identification Test. Guidelines for Use in Primary Care. 2nd ed. Geneva: World Health Organization;2001.
14. Maiwald H, Jilg W, Bock HL, Löscher T, Sonnenburg F. Long-term persistence of anti-HAV antibodies following active immunization with hepatitis A vaccine. Vaccine. 1997; 15:346–348.

15. Reuman PD, Kubilis P, Hurni W, Brown L, Nalin D. The effect of age and weight on the response to formalin inactivated, alum-adjuvanted hepatitis A vaccine in healthy adults. Vaccine. 1997; 15:1157–1161.

17. Jeon GS, Lee HY. Associated Factors of Binge Drinking and Problem Drinking among Korean Men and Women. Korean J Health Educ Promot. 2010; 27:91–103.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download