Abstract
Purpose
The aim of this study was to evaluate the effects of perioperative psychological and music interventions in elderly patients undergoing elective surgery on anxiety, post-operative pain, and changes in heart rate variability (HRV) to ascertain if perioperative psychological and music interventions can affect overall anxiety levels.
Materials and Methods
Fourty elderly patients undergoing elective surgery were randomized to two groups; one group received psychological and music intervention, and the other was the control. The intervention group underwent psychological intervention and listening to music for 30 min before surgery.
Results
The mean change in HRV as determined by low frequency (LF) power measurements. After the intervention, the ratio of mean LF to high frequency (HF) power decreased significantly in the intervention group compared to before the intervention (p<0.05). In the control group, mean LF measurements and the ratio of LF:HF did not change significantly. In the intervention group, mean HF power was significantly higher after the procedure than before (p<0.01). Moreover, the mean self-rating anxiety score of the intervention group decreased after the procedure compared to before (p<0.05). The mean visual analogue score of the intervention group 6 hours after surgery was significantly lower than that of the control group (p<0.01).
Perioperative psychological pressure may lead to the reduce of pain threshold, and may affect the immune function and stability of the circulatory system.1 As part of the physiological process of aging, degeneration of the autonomic nervous system occurs gradually, leading to gradual decrease in the ability to adapt and regulate the cardiovascular-stress response. The inability of the autonomic nervous system to effectively regulate the cardiac rhythm leads to higher rates of cardiac dysfunction, myocardial infarction, and other cardiac emergencies in the elderly.2,3,4
Although some studies report that physiological and music intervention is effective in reducing anxiety levels,5,6,7,8 few studies have examined the effects of physiological and music intervention on perioperative safety in elderly patients. For example, psychological intervention and direct communication with patients by anesthetists and nurses before surgery was found to effectively reduce patient anxiety and improve patient satisfaction.7 In another study, the intervention group watched a short film depicting the patient's in-hospital journey and concluded that preoperative multimedia information reduces patient anxiety before undergoing anaesthesia.5 In addition, use of an anaesthesia mask and parental distraction prior to surgery are effective at reducing anxiety in children.8 This previous research suggests that music intervention can reduce anxiety perioperatively, but its effect in elderly patients on heart rate variability (HRV) has not been fully investigated.
HRV refers to successive fluctuating RR intervals (instantaneous heart rate), which is a reflection of the regulation of heart rhythm by the central nervous system. The short-term HRV spectrum indicates that the HRV power spectrum can be used to monitor cardiac vagal modulation levels. Low frequency (LF) power increases when sympathetic activity is enhanced, and the ratio of LF to high frequency (HF) power can act as a quantitative indicator of the cardiac vagal-sympathetic balance.9
Psychological and music intervention are safe, non-invasive methods that patients are more likely to accept.6,7 In this experiment, we performed safe and objective testing to evaluate whether psychological and music intervention can enhance the stability of cardiac vagal-sympathetic balance and increase the safety of surgery in elderly patients with these perioperative interventions.
After the Ethical Commitee at Shengjing Hospital approved this study and all patients received informed consent, 40 elderly patients who underwent elective gynecological or lower limb orthopedic surgery were enrolled from June 2011 to September 2011. The study participants ranged in age from 65 to 80 years, had an American Society of Anesthesiologists physical status score of 2 or 3, and a body mass index <40 kg/m2. Inclusion criteria included normal heart, pulmonary, liver, and kidney function on preoperative examination; no history of endocrine or central nervous system disease or drug allergies; and absence of severe anemia, malnutrition, hypoproteinemia, and water-electrolyte/acid-base imbalance disorders. All patients fasted for 12 hours and were advised not to drink fluids for 4 hours before surgery.
This trial was registered in the Chinese Clinical Trial Registry System on May 30, 2012 (registration number ChiCTR-TRC-12002208).
The sample size was calculated using a statistical power analysis program G*Power10 for both groups considering a 5% level of significance, 80% power, 0.92 effect size, and the effect size was calculated using the means and standard deviations of an earlier experiment. The sample size calculation indicated 20 individuals were required for each group.
Patients were randomized into the psychological and music interventions group or the control group. Randomization was performed using a computer generated random number table.
Spinal-epidural anesthesia was performed at the L2-3 interspace with a maximum sensory level of T8. Ephedrine (10 mg) was injected if the blood pressure dropped to less than 90 mm Hg or lower than 30% of the basal blood pressure. The intervention group of patients continued listening to music after anesthesia was administered. Both groups of patients were instructed to inform the staff if they experienced discomfort.
All patients underwent routine preoperative visits.
Patients and their families were informed about the status and severity of their illness. The surgical experience was described while the patient was in a relaxed, comfortable atmosphere, using appropriate words. Patients were taught effective methods for controlling anxiety, including abdominal breathing. Patients were also told that technically advanced anesthesia provides complete pain control during surgery. To decrease the development of tension and fear, patients were administered appropriate sedating agents to ensure adequate sleep the night before surgery. Patients in the intervention group listened to soft music in quiet surroundings for 30 min before undergoing surgery. They were instructed to close their eyes and relax their body. The control group patients underwent routine preoperative visits where their status and severity of illness, surgery, and anesthesia were described in detail. Patients in the control group were also administered appropriate sedating agents to ensure adequate sleep the night before surgery. Before surgery, patients in the control group were also instructed to close their eyes and relax their body in quiet surroundings for 30 min, but without music.
Intraoperative psychological intervention was administered to patients in the intervention group undergoing nerve block anesthesia, which allows the patient to be awake or partially awake during the surgical procedure. Any adverse stimuli may lead to the development of tension and fear in the patient; therefore, nurses and anesthesiologists can talk with patients to distract them from the procedure. Patients listened to soft music during the surgery and were directly asked if they are uncomfortable or felt pain. In the case a patient was experience discomfort, the appropriate agents were administered for relief. The operating room was quiet and free of upsetting sounds, including discussion of the patient's condition, so a comfortable environment was maintained throughout the surgery. In the control group, only patients who expressed discomfort were provided medical treatments and doctors/nurses did not speak about the patient's status in the surgery room.
Anesthetists visited patients in the intervention group twice after surgery and listened to any feelings or concerns among patients or their families, answered any questions, and instructed them on postoperative care and treatment. In the control group, anesthetists listened to patients and their families and answered their questions during the first visit. At the second visit, anesthetists described postoperative care and collected additional data.
Patients in both groups completed the Self-Rating Anxiety questionnaire11,12 at their preoperative visit and again right before surgery. The Zung Self-Rating Anxiety Scale (SAS) was used to assess anxiety, which contains 20 items.11,12 Each item is scored on a self-rating scale from 1 to 4, and scores are added and multiplied by 1.25 to obtain a standard score (T score). A T score >50 is considered to indicate anxiety, and the higher the score the more severe the anxiety.
Patients in both groups underwent HRV frequency-domain analysis using Holter monitoring before the preoperative interview and again before surgery. Two different, trained staff performed the interventions and monitored HRV; the staff who collect HRV outcomes was blinded to the study. Frequency domain analysis was performed by a TLC4000 holographic dynamic electrocardiogram analysis system (Contec Medical Systems, Beijing, China). The total power, LF power, HF power, and LF/HF ratio were determined.
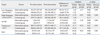
Patient characteristics are shown in Table 1.
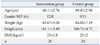
No significant differences for the mean values of total power, LF, HF, or the LF/HF ratio before the intervention were found between the 2 groups of patients. For the intervention group, the mean LF and LF/HF ratio decreased significantly (p<0.05 for both) after the procedure compared to before the procedure, and the mean HF power level was significantly higher after the procedure than before the procedure (p<0.01). In the control group, the differences in mean values for LF, HF, total power, and LF/HF ratios of the control patients measured at the different time points were not significant. For the intervention group, the mean change before and after the procedure was significantly larger than that of the control (p<0.01) (Table 2).
The mean SAS score of the intervention group patients decreased significantly after the procedure compared to before (p<0.05), but the mean scores among control patients were essentially unchanged. Before the procedure, no significant differences in mean SAS scores between the two groups were found. However, the mean SAS score of the intervention group was significantly lower than that of the control group after the procedure (Table 2).
The mean visual analogue pain score 6 hours after surgery was 3.50±1.05 in the intervention group, significantly lower than the control group (4.85±1.31, p<0.01).
The main finding of this prospective, randomized, controlled clinical trial was that the mean SAS score of the intervention group was significantly lower after the intervention than before. In addition, the mean HF of the intervention group was significantly higher after the procedure than before, and the mean LF and LF/HF ratio were significantly lower after the intervention than before. Between groups, the mean difference between perioperative and postoperative values for LF, HF, LF/HF ratio, and SAS scores differed in the intervention group more than that of the control group.
Heart rate variability refers to successive fluctuating RR intervals (instantaneous heart rate).9,13 The frequency bands of frequency domain analysis are divided into total power, ultra-low frequency power, extremely low frequency power, LF power, and HF power. The short-term HRV spectrum shows that the HRV power spectrum can be used to monitor cardiac vagal modulation levels. LF increases when sympathetic activity is enhanced, and the LF/HF ratio can act as a quantitative indicator of the cardiac vagal-sympathetic balance.
In this study, the mean HF of the intervention group was higher after the procedure than before. This indicates that the activity of the parasympathetic nervous system was enhanced. The mean LF and LF/HF ratio of the intervention group decreased significantly after the procedure compared to before. These results demonstrate that direct psychological intervention can significantly reduce the activity of the sympathetic nervous system, restore the balance of the sympathetic and the parasympathetic nervous system, and reduce preoperative anxiety. These effects may also contribute to patient safety throughout the perioperative period.
Additionally, pain associated emotions can affect the perception of pain, influence the pain-related physiological reactions, and anxiety. All of these effects on the hypothalamus autonomic nervous system, leading to enhancement of the somatosensory reaction to stimulation, which results in increased sensitivity to pain or the perception of increased pain.1,14 This may explain the low visual analogue pain score 6 hours after surgery in the intervention group.
The association of psychological factors with human health and disease has come under increasing scrutiny. Patients fear anesthesia and surgery because of a lack of understanding and may have some misconceptions regarding the surgical procedure. These emotions can lead to anxiety. Mental stress can stimulate the sympathetic-adrenal system. Leading to coronary artery spasm, platelet aggregation, increased blood viscosity, or cardiovascular complications such as myocardial ischemia and myocardial infarction. And may even lead to cardiac arrhythmias and sudden death.15
Psychological therapy and music before surgery can significantly reduce the blood levels of prednisone and natural killer cells, reduce neural hormones and immune-mediated stress, eliminate worries, reduce fear and anxiety, and enhance patient confidence in surgery and anesthesia.16,17,18 Soltner, et al.7 also reported that psychological intervention and direct communication with patients by anesthetists and nurses before surgery can effectively reduce patient anxiety and improve patient satisfaction.
There were also some limitations in our study. Anesthetic drugs may affect HRV;19,20,21 however, we did not collect data intraoperatively or postoperatively. Some important information within this period could have been missed. Thus, further studies are needed.
In summary, perioperative psychological and music interventions in elderly patients can effectively reduce anxiety and relieve postoperative pain.
Figures and Tables
Table 2
Heart Rate Variability Frequency Domain Analysis and Self-Rating Anxiety Scale (SAS) Scores (Mean±SD)
LF:HF, the ratio of low-frequency power to high-frequency poer.
n=20 in each group. Pre-intervention represents data obtained before the intervention at the preoperative visit. Post-intervention represents data obtained after the intervention and 5 min before the anesthesia procedure.
*p<0.01 within group.
†p<0.01 between groups.
References
1. Lautenbacher S, Huber C, Schöfer D, Kunz M, Parthum A, Weber PG, et al. Attentional and emotional mechanisms related to pain as predictors of chronic postoperative pain: a comparison with other psychological and physiological predictors. Pain. 2010; 151:722–731.

2. Beattie WS, Buckley DN. Frequency domain measures of heart period and postoperative ischemia. Anesthesiology. 1993; 79(3A):A1249.
3. Kim SJ, Oh YJ, Kim KJ, Kwak YL, Na S. The effect of recorded maternal voice on perioperative anxiety and emergence in children. Anaesth Intensive Care. 2010; 38:1064–1069.

4. Zhang XW, Fan Y, Manyande A, Tian YK, Yin P. Effects of music on target-controlled infusion of propofol requirements during combined spinal-epidural anaesthesia. Anaesthesia. 2005; 60:990–994.

5. Jlala HA, French JL, Foxall GL, Hardman JG, Bedforth NM. Effect of preoperative multimedia information on perioperative anxiety in patients undergoing procedures under regional anaesthesia. Br J Anaesth. 2010; 104:369–374.

6. Koch ME, Kain ZN, Ayoub C, Rosenbaum SH. The sedative and analgesic sparing effect of music. Anesthesiology. 1998; 89:300–306.

7. Soltner C, Giquello JA, Monrigal-Martin C, Beydon L. Continuous care and empathic anaesthesiologist attitude in the preoperative period: impact on patient anxiety and satisfaction. Br J Anaesth. 2011; 106:680–686.

8. Fortier MA, Blount RL, Wang SM, Mayes LC, Kain ZN. Analysing a family-centred preoperative intervention programme: a dismantling approach. Br J Anaesth. 2011; 106:713–718.

9. Bailey JR, Fitzgerald DM, Applegate RJ. Effects of constant cardiac autonomic nerve stimulation on heart rate variability. Am J Physiol. 1996; 270(6 Pt 2):H2081–H2087.

10. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007; 39:175–191.

12. Zung WW. The measurement of affects: depression and anxiety. Mod Probl Pharmacopsychiatry. 1974; 7:170–188.

13. Nicolini P, Ciulla MM, De Asmundis C, Magrini F, Brugada P. The prognostic value of heart rate variability in the elderly, changing the perspective: from sympathovagal balance to chaos theory. Pacing Clin Electrophysiol. 2012; 35:622–638.

14. Rainville P, Bao QV, Chrétien P. Pain-related emotions modulate experimental pain perception and autonomic responses. Pain. 2005; 118:306–318.

15. Mallik S, Krumholz HM, Lin ZQ, Kasl SV, Mattera JA, Roumains SA, et al. Patients with depressive symptoms have lower health status benefits after coronary artery bypass surgery. Circulation. 2005; 111:271–277.

16. Wang SM, Kulkarni L, Dolev J, Kain ZN. Music and preoperative anxiety: a randomized, controlled study. Anesth Analg. 2002; 94:1489–1494.

17. Lepage C, Drolet P, Girard M, Grenier Y, DeGagné R. Music decreases sedative requirements during spinal anesthesia. Anesth Analg. 2001; 93:912–916.

18. Ayoub CM, Rizk LB, Yaacoub CI, Gaal D, Kain ZN. Music and ambient operating room noise in patients undergoing spinal anesthesia. Anesth Analg. 2005; 100:1316–1319.

19. Mazzeo AT, La Monaca E, Di Leo R, Vita G, Santamaria LB. Heart rate variability: a diagnostic and prognostic tool in anesthesia and intensive care. Acta Anaesthesiol Scand. 2011; 55:797–811.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download