Abstract
Purpose
The aim of this study is to explore non-steroid anti-inflammation drugs (NSAIDs) potency for pelvic floor muscle pain by measuring local concentration in a rat model.
Materials and Methods
We used nine NSAIDs, including nabumetone, naproxen, ibuprofen, meloxicam, piroxicam, diclofenac potassium, etodolac, indomethacin, and sulindac, and 9 groups of female Wister rats. Each group of rats was fed with one kind of NSAID (2 mg/mL) for three consecutive days. Thereafter, one mL of blood and one gram of pelvic floor muscle were taken to measure drug pharmacokinetics, including partition coefficient, lipophilicity, elimination of half-life (T1/2) and muscle/plasma converting ratio (Css, muscle/Css, plasma).
Chronic pelvic pain (CPP) is defined as pelvic pain of at least 6 months duration. It is a common gynecological problem with an estimated prevalence in 38 per 1000 in women aged 15 to 73 years.1 It is the single most common indication for referral to gynecology clinics, accounting for 20% in subsequent care.2 In the United States, over 600000 patients have a hysterectomy annually, including approximately 10% for the diagnosis of CPP.3,4,5
Various comprehensive factors contribute to the development of CPP syndrome. However, myofacial pain syndrome derived from pelvic floor muscles is one of the major potential factors. In general, remedy attention for myofacial pain includes: 1) analgesics and muscle relaxants, 2) message therapy, 3) and thermo treatment. The latter two require physical and therapeutic specialists. Because the pelvic floor muscle is embedded into deeper tissues, there is a limit to the efficacy and efficiency of thermo treatment and/or massage. Currently, medication is the effective choice of treatment in terms of patient benefit and complicity, especially for outpatient care.
The World Health Organization's guidelines for pain treatment in nonmalignant pain recommend drugs such as acetaminophen or a non-steroidal anti-inflammatory drug (NSAID).6 Theoretically, each NSAID should have the same active mechanism and should contribute the same level of analgesic effect.7,8 In fact, however, physicians empirically and generally either have a preference or select one in a trial and error process. Furthermore, the best choice of NSAID to relive CPP has not yet been illustrated. Currently, no research paper has given a clear insight into the selection of NSAIDs in relation to clinical practice on the subject of pelvic floor muscle pain.
The specific clinical experience attracted our attention to the variation in NSAID use for pain mitigation. Naproxen or ibuprofen was generally used and studied as the first choice for dysmenorrhea.9,10,11 Meanwhile, it is customary to prescribe both medicines for pelvic floor muscle pain. However, in our own experience they are unsatisfactory from a physician's point of view. We followed general procedure and substituted different kinds of NSAIDs for these medicines, and found some of them, such as diclofenac potassium and meloxicam, were more effective for pelvic floor muscle pain. It was thus deduced that various NSAIDs perform differently in terms of pain relief in real clinical practice.
Pain is a physical sensation, and it is not feasible to precisely detect the analgesic effect of NSAIDs on pelvic floor muscle pain in animals. Furthermore, it is not possible to recruit only a limited number of patients to rank analgesic effectiveness by taking several NSAIDs simultaneously. Rather large clinical trials are required to ascertain NSAIDs' efficacy in CPP clinical use, which is time consuming and cost effective.
Therefore, our study was designed to measure steady state pharmacokinetic parameters with mice and estimate the extent of distribution of NSAIDs among plasma and pelvic floor muscle. The aim of this study is to explore the NSAIDs potency for pelvic floor muscle pain by measuring local concentration in a rat model.
This study was approved by the Institutional Animal Care and Use Committee in Chang Gung Memorial Hospital. Wister female mice, weighing from 230 to 300 grams and aged eight weeks at the time of experiment, from the National Laboratory Animal Center were used. There were nine groups; each group included five mice (n=5) on which one NSAID was studied. In addition, another group of five mice was fed with a placebo serving as a control group.
Test NSAIDs were as follows: nabumetone, naproxen, ibuprofen, meloxicam, piroxicam, diclofenac potassium, etodolac, indomethacin, and sulindac. These active substances were generously donated by several different commercial suppliers and were in compliance with Pharmacopeia purity standards. NSAIDs comprise a heterogeneous group of medications, e.g., arylpropionic acids, enolic acids, alkanones, etc. (Table 1). The target regimen was designed at 2 mg at each dosing time, which was based upon solubility, partition coefficient (log P), lipophilicity (pKa) and dose converting factor for mice. The divergence between pKa and log P contributed to various biotransformation, such as the elimination of half-life (T1/2). The steady state period was calculated from various T1/2.
The aforementioned medicines were first dissolved in alcohol to make a fixed concentration of 20 mg/mL, denoted as stock solution. On the dosing date, individual stock solution was diluted with beta-cyclodextrin, serving as a vehicle, to make a dosing concentration of 2 mg/mL. One mL of test drug solution (containing 2 mg of drug substance) was fed to the mice with a feeding tube three times a day for three consecutive days.
On the 4th day, the mice were anesthetized with ether, and approximately 1 mL of blood was withdrawn from the inferior vena cava after 15 minutes, 30 minutes and 40 minutes of dosing. The blood was transferred into a sodium heparin coated vacutainer (green cap), centrifuged at 3000 g for 5 minutes, and 0.5 mL of plasma was removed from the supernatant. The plasma was transferred into a scintillation vial and frozen at -20℃. Then, the mice were sacrificed by CO2 respiration, and about 1 gram of pelvic floor muscle was removed. The muscle sample was immersed into 2 mL of methanol, homogenized, and centrifuged, and as much supernatant as possible was taken (around 2 mL). Methanol solution was transferred into a scintillation vial and frozen at -20℃.
A specific de-protein and extraction method was developed for each compound from each plasma sample. The methanol supernatant of muscle sample specimen was dried under nitrogen and reconstituted with 200 uL of methanol. Calibration standard curves were made, and samples on validated liquid chromatograph/tandem mass spectrometer (LC-MS/MS) methods were measured. Each drug's concentration in plasma as well as in the pelvic floor muscle was calculated from linear calibration curves.
Maxima plasma and pelvic floor muscle concentrations were measured for each study animal at steady state. With each study compound, five sets of concentrations from plasma and pelvic floor muscle were averaged and converted to its ratio at steady state (Css, muscle/Css, plasma). Css, muscle/Css, plasma of various groups were analyzed using the nonparametric testing (Kruskal Wallis test) for data that were not normally distributed. The pairwise comparison was analyzed by Dunn test. All probability values were two-sided. Significance level was accepted at probability below 5%.
In the present study, piroxicam had the longest T1/2, up to 50 hours. After calculation, the steady state period was determined at 3 days.
Subsequently, samples were taken at the steady state period. Specific preparations and analytical methods of LC-MS/MS were developed for each individual compound. Linear calibration curves with concentration ranges of 0 to 10000 ng/mL were used to calculate concentrations of unknown sample.
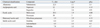
Table 2 illustrates the steady state concentrations for plasma and pelvic floor muscle. Maximum steady state concentration was chosen from the highest plasma concentration. The mean ratio ranged from 0.03 (ibuprofen) to 0.85 (diclofenac potassium), except for sulindac. Sulindac was largely more predominant in plasma than in muscle tissue to a large extent. The ratios for naproxen and ibuprofen were found to be lower at 0.04 and 0.03 respectively. The converting ratio of Css, muscle/Css, plasma was depicted in Fig. 1. The mean ratios of Css, muscle/Css, plasma of the nine groups were significantly different (p<0.001). However, the statistical significance was observed only in dilcofenac potassium versus naproxen (p=0.017), dilcofenac potassium versus ibuprofen (p=0.003), dilcofenac potassium versus sulindac (p=0.001), etodolac versus ibuprofen (p=0.025), etodolac versus sulindac (p<0.001), and meloxicam versus sulindac (p=0.027). The other pairs were insignificant. The results implied that diclofenac potassium tended to have a higher disposition in pelvic floor muscle than either naproxen or ibuprofen.
The pathogenesis of CPP is not well understood. Organs in the abdomen and/or pelvis can play a role in the etiology of CPP. Many disorders associated with these organs systems can induce CPP, including endometriosis, interstitial cystitis,
and irritable bowel syndrome, etc. Almost 40% of CPP patients who had no obvious pelvic lesion and 22% of CPP patients who were suspected of having a uterine pathology proclaimed persistent pain after hysterecomy.3,12 Therefore, CPP is considered a symptom, not a disease, requiring an integral multidisciplinary approach for diagnosis and treatment
in order to improve the successful rate of pain relief.
In our study, we focused mainly on the muscular area of the pelvic floor. However, much literature put special emphasis on physical therapy because many women with CPP have significant myofascial pain.13,14,15 Our clinical pelvic examinations found that many patients indeed have had trigger points in the pelvic floor musculature, including the levator ani, obturator, pubococcygeus, and deep transverse perineal muscles. Moreover, many researches have explored how the musculoskeletal system is involved in disorders such as vulvodynia, coccygodynia, levator ani syndrome, fibromyalgia, vulvar vestibulitis syndrome, dyspareunia, pelvic floor tension myalgia, urgency-frequency syndrome, and urethral syndrome.15,16,17,18,19,20 Therefore, to alleviate muscle pain itself is crucial in order to treat CPP caused by pelvic floor pain.
Naproxen and ibuprofen are widely believed to be the empirical choices in the gynecological field, especially for dysmenorrhea.7,8,9,10,11 However, our own experience found their effectiveness in treating CPP, caused by pelvic floor muscle pain, not satisfactory. Adhering to NSAID clinical practice guidelines, substitution is recommended and diclofenac potassium was incidentally found to have a good effect. Furthermore, different medical departments have always had their own preferences for empirical NSAIDs in their particular fields. This indicates the probability that specific NSAIDs are more suitable for different individual pains. These facts together aroused our curiosity to undertake a translational study and to explore various choices of NSAID to provide medical attention for pelvic floor muscle pain. It was of an interest to find that diclofenac potassium exerted a significant effect on pelvic floor muscle pain, coinciding with our clinical experience.
NSAID efficacy is shown by the interplay among multiple processes that regulate drug disposition (pharmacokinetics) and response (pharmacodynamics). For orally administered NSAID drugs, their pharmacological actions are greatly influenced by adequate intestinal absorption and distribution to the sites of action, before their elimination by metabolic and excretory pathways. The metabolism reactions are generally grouped into 2 phases. Phase I involve reactions such as oxidation, reduction, and hydrolysis, which are primarily mediated by cytochrome P450 family of enzymes. Phase II produce an endogenous compound, such as glucuronic acid, glutathione, or sulfate, for conjugation with the drug itself or its phase I derivatives, deriving metabolite to produce a more polar end product.21 An entire process, described as the LADMER system (liberation, absorption, distribution, metabolism, elimination and response), is involved in eliciting NSAID efficacy and response.
The pKa of a drug affects not only its absorption but also its metabolism, protein binding, and distribution. Generally, the higher the drug's pKa, the higher its metabolism, the stronger its binding to protein and the greater its distribution.22 Therefore, if two drug products have the same in vivo dissolution profile, they would have the same distribution. However, various physicochemical properties compromise in vivo distribution.
Each classification of NSAID has a different target concentration, governed by its physicochemical property and biotransformation. In this study, we hypothesized that individual NSAIDs can perform different responses for various pain relief. Indeed, the disposition ratio of plasma to pelvic floor muscle revealed wide variety, as shown in Table 2, illustrating that individual NSAIDs might produce different levels of pain relief in the pelvic floor muscle. Our data showed diclofenac potassium having a higher ratio than naproxen (p=0.017) and ibuprofen (p=0.003). Similarly, our clinical experience indicated that diclofenac potassium performed better in terms of clinical efficacy for pain relief than naproxen and ibuprofen.
The area of pharmacoeconomics has become more and more important for health authorities and health insurance companies worldwide. NSAIDs have been used for many decades and heralded for their safety and efficacy. However, suitable and scientifically-proven choices of NSAID for pelvic floor muscle pain would shorten the trial-and-error period and reduce therapeutic costs. Our animal model also offers concrete idea for choosing the most appropriate NSAIDs to effectively relieve various pains.
Chronic pelvic muscle pain is a troublesome problem due to deep anatomy and hard to approach by some invasive interventions. At present, the kind of pain attracts less attention than it should, and thus, the effectiveness of medication to relieve it is still compromised. In addition, various NSAIDs seem to have different effect for various pains. The goal of this study was to explore and find the best possible selection of NSAIDs for CPP caused by pelvic floor muscle pain. Our animal design is unique because it is at the cutting edge of application science. Even though the results do coincide with our clinical experience, a well-designed randomized controlled trial is needed to confirm our discoveries with this animal model.
Figures and Tables
Fig. 1
The conversion ratio of pelvic floor muscle concentration and plasma concentration (Css, muscle/Css, plasma) for each test drug. Nab, nabumetone; Nap, naproxen; Ibu, ibuprofen; Mel, meloxicam; Pir, piroxicam; Dil, dilcofenac potassium; Eto, etodolac; Ind, indomethacin; Sul, sulindac.
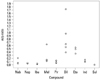
Table 2
Steady State Concentrations in Plasma and Muscle from Each Group

Css, muscle, concentration in pelvic floor muscle at steady state (ng/mL); Css, plasma, plasma concentration at steady state (ng/mL); ND, not detectable.
Values are given as mean±SD. The Css, muscle of sulindac is undetectable, by which the Css, muscle/Css, plasma is incomparable.
*Kruskal Wallis test.
ACKNOWLEDGEMENTS
This study was supported by the Medical Research Project (CMRPG280101) in Chang Gung Memorial Hospital and its laboratory animal center at Keelung. In addition, the experiment was supported by the Chemical laboratory in Standard Chemistry & Pharmaceutical. Co., Ltd. However, the research was not sponsored by any pharmaceutical factory and company. The authors thank Ms. Hsiu-Ping Yang for her assistance. The authors also thank Mr. Evan Colbert for his editing English, and Ms. Hsiao-Jung Tseng for statistical consultation, who was supported by grants from Biostatistical Center for Clinical Research, Chang Gung Memorial Hospital (CLRPG340599).
References
1. Zondervan KT, Yudkin PL, Vessey MP, Dawes MG, Barlow DH, Kennedy SH. Prevalence and incidence of chronic pelvic pain in primary care: evidence from a national general practice database. Br J Obstet Gynaecol. 1999; 106:1149–1155.

2. Howard FM. The role of laparoscopy in chronic pelvic pain: promise and pitfalls. Obstet Gynecol Surv. 1993; 48:357–387.

3. Vercellini P, Viganò P, Somigliana E, Abbiati A, Barbara G, Fedele L. Medical, surgical and alternative treatments for chronic pelvic pain in women: a descriptive review. Gynecol Endocrinol. 2009; 25:208–221.

4. Lee NC, Dicker RC, Rubin GL, Ory HW. Confirmation of the preoperative diagnoses for hysterectomy. Am J Obstet Gynecol. 1984; 150:283–287.

6. Krames E. Using a pain treatment continuum: a logical and cost-effective approach. In : Raj PP, editor. Practical Management of Pain. St. Louis: Mosby;2000. p. 441–444.
7. Owen PR. Prostaglandin synthetase inhibitors in the treatment of primary dysmenorrhea. Outcome trials reviewed. Am J Obstet Gynecol. 1984; 148:96–103.

8. Zhang WY, Li Wan Po A. Efficacy of minor analgesics in primary dysmenorrhoea: a systematic review. Br J Obstet Gynaecol. 1998; 105:780–789.

9. Akin MD, Weingand KW, Hengehold DA, Goodale MB, Hinkle RT, Smith RP. Continuous low-level topical heat in the treatment of dysmenorrhea. Obstet Gynecol. 2001; 97:343–349.

10. Budoff PW. Use of mefenamic acid in the treatment of primary dysmenorrhea. JAMA. 1979; 241:2713–2716.

11. Milsom I, Minic M, Dawood MY, Akin MD, Spann J, Niland NF, et al. Comparison of the efficacy and safety of nonprescription doses of naproxen and naproxen sodium with ibuprofen, acetaminophen, and placebo in the treatment of primary dysmenorrhea: a pooled analysis of five studies. Clin Ther. 2002; 24:1384–1400.

12. Hillis SD, Marchbanks PA, Peterson HB. The effectiveness of hysterectomy for chronic pelvic pain. Obstet Gynecol. 1995; 86:941–945.

13. Prather H, Dugan S, Fitzgerald C, Hunt D. Review of anatomy, evaluation, and treatment of musculoskeletal pelvic floor pain in women. PM R. 2009; 1:346–358.

14. Baker PK. Musculoskeletal origins of chronic pelvic pain. Diagnosis and treatment. Obstet Gynecol Clin North Am. 1993; 20:719–742.
15. Weiss JM. Pelvic floor myofascial trigger points: manual therapy for interstitial cystitis and the urgency-frequency syndrome. J Urol. 2001; 166:2226–2231.

16. Glazer HI, Rodke G, Swencionis C, Hertz R, Young AW. Treatment of vulvar vestibulitis syndrome with electromyographic biofeedback of pelvic floor musculature. J Reprod Med. 1995; 40:283–290.

17. Lukban J, Whitmore K, Kellogg-Spadt S, Bologna R, Lesher A, Fletcher E. The effect of manual physical therapy in patients diagnosed with interstitial cystitis, high-tone pelvic floor dysfunction, and sacroiliac dysfunction. Urology. 2001; 57:6 Suppl 1. 121–122.

18. Sinaki M, Merritt JL, Stillwell GK. Tension myalgia of the pelvic floor. Mayo Clin Proc. 1977; 52:717–722.
19. Gunter J. Chronic pelvic pain: an integrated approach to diagnosis and treatment. Obstet Gynecol Surv. 2003; 58:615–623.

20. Thiele GH. Coccygodynia: cause and treatment. Dis Colon Rectum. 1963; 6:422–436.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download