Abstract
Purpose
We analyzed age-related changes of bone mineral density (BMD) and compared with those of U.S and Japanese participants to investigate the prevalence of osteoporosis in Korea.
Materials and Methods
The data were collected in the 2008-2011 in Korea National Health and Nutrition Examination Survey (KNHANES) IV and V to select a representative sample of civilian, noninstitutionalized South Korean population. Bone mineral measurements were obtained from 8332 men and 9766 women aged 10 years and older.
Results
BMD in men continued to decline from 3rd decade, however, in women, BMD remained nearly constant until the 4th decade and declined at rapid rate from the 5th decade. The prevalence of osteoporosis in Korea is 7.3% in males and 38.0% in females aged 50 years and older. The prevalence of osteopenia in Korea is 46.5% in males and 48.7% in females, aged 50 years and older. The lumbar spine and femur BMD in Korean females 20 to 49 years of ages was lower than in U.S. and Japan participants.
Osteoporosis is defined as a disease characterized by low bone mass and micro-architectural deterioration of bone tissue, leading to enhanced bone fragility and a consequent increase in fracture risk.1 Since osteoporosis causes fractures, pain and inconvenience of activity, prevention of osteoporosis is of great importance in maintaining quality-of-life of the elderly.2,3 Bone mineral density (BMD) is influenced by ethnicity, geographic factors, diet, exercise, family history, and other lifestyle factors. For example, BMD values in white females are lower than in black females, and values in Asian females are lower than in white females.4,5,6 Much effort is needed to determine appropriate reference values of BMD at different skeletal sites in different races and areas to accurately diagnose osteoporosis.
In Korea, the government and medical officials have recently emphasized the importance of osteoporosis, and marketing of osteoporosis medications has shown a dramatic increase during the past five years. Previous studies conducted in Korea have also investigated the prevalence of osteoporosis in specific populations. For example, one study surveyed the incidence of osteoporosis in a healthy Korean population by obtaining the BMD at the distal radius and calcaneus. The "Ansung cohort study," which was conducted in a rural setting, revealed the prevalence of Korean osteoporosis in the Ansung regional area.7,8
Large-scale epidemiologic studies regarding the prevalence of osteoporosis and osteopenia have been conducted extensively in Western countries; however, the Ministry of Health and Welfare in Korea had pushed back this task on the priority risk and had prevented similar studies in a representative South Korean sample. The Ministry of Health and Welfare in Korea began a nationwide, cross-sectional survey measuring the BMD (g/cm2) at the lumbar spine (L2-4), femoral neck, trochanter, and Ward's triangle using dual-energy X-ray absorptiometry (DXA) (Hologic Discovery, Hologic Inc., Bedford, MA, USA) in 2008. In this report, we present the 2008-2011 Korea National Health and Nutrition Examination Survey (KNHANES) IV and V data on BMD and the prevalence of osteoporosis among a South Korean population aged 10 years or older.
The data were collected in the 2008-2011 KNHANES IV and V, a nationwide, cross-sectional survey conducted in a South Korean population in 2008-2011 which used a stratified, multi-stage clustered probability sampling to select a representative sample of civilian, non-institutionalized South Korean population. All examination and health interviews by trained teams were conducted in mobile centers while nutrition survey was done in household. DXA examinations were conducted on sampled persons aged 10 years and older except for pregnant women or persons who had examination with a contrast agent within a week of the survey. Bone mineral measurements were obtained from 8332 men and 9766 women aged 10 years and older. Participants were analyzed according to age bracket and residential area (urban or rural: seven metropolitan cities or six provinces).
We obtained information regarding gender, age and chronic illness in each residential area.
We asked participants whether they had ever suffered hypertension, dyslipidemia, diabetes mellitus, thyroid disease, anemia, chronic hepatitis, cerebral stroke, ischemic heart disease, osteoporosis, or chronic lung disease. Participants were also asked about any history of bone fractures.
Research staff obtained anthropometric measurements while participants wore light clothing and no shoes. Height was measured to the nearest 0.1 cm, and weight was measured in the upright position to the nearest 0.1 kg on a calibrated balance-beam scale.
Body mass index (BMI) was calculated using the following equation:
BMI=weight (kg)/square of height (m2).
We measured BMD (g/cm2) at the lumbar spine (L2-4), femoral neck, trochanter, and Ward's triangle by DXA (Hologic Discovery, Hologic Inc., Bedford, MA, USA). The machine was calibrated daily, and the coefficients for duplicate measurements in 50 adults were 2.2%, 1.9%, and 2.3%, respectively. The BMD data for U.S. participants were available from the new reference databases, National Health and Nutrition Examination Survey (NHANES) (2007-2008). The Japanese BMD data were obtained from a previous healthy Japanese-population-based osteoporosis cohort study in which the BMDs at the lumbar spine and hip were measured with the Hologic QDR 4500 bone densitometer.12
According to the World Health Organization (WHO) diagnostic classification, the diagnosis of osteoporosis is established by measurement of BMD by DXA of the spine and hip, and/or forearm, although a clinical diagnosis can be made in individuals who sustain a low-trauma or fragility ftracture.9 The WHO defines osteoporosis as a BMD of 2.5 standard deviations (SD) below the peak bone mass of a young, healthy, gender- and race-matched reference population, as follows:10
The T-score compares and individual's BMD with the mean value for young normal individuals and expresses the differences as a standard deviation score.9
1) Normal bone mass: T-score (-1.0 and above)
2) Low bone mass (osteopenia): T-score (between -1.0 and -2.5)
3) Osteoporosis: T-score (-2.5 and below)
The T-score compares and individual's BMD with the mean value for young normal individuals and expresses the differences as a standard deviation score.10
The exclusion criteria included current patient's report of any disease that affects bone metabolism, including hyperthyroidism, hyperparathyroidism, chronic renal failure, bronchial asthma, rheumatoid arthritis, and cancer, and objects which are being taken, such as glucocorticoids or thyroid hormone.
Data were analyzed using SAS software, version 9.2 (SAS Institute, Cary, NC, USA).
Mean bone mineral densities and prevalence of osteoporosis were estimated by performing PROC SURVEYMEANS procedure. The BMD differences between the geographic areas in Korean population and ethnic group in Korean and US population were tested using PROC SURVEYREG procedure. For comparison with US population, BMD data of NHANES (2007-2010) were used.11 The comparison of BMD in Korean female population with those in Japanese female population was performed using t-test, calculated based on the BMD estimates and their standard errors.12 Differences were considered to be statistically significant when the p value was less than 0.05. All estimates were obtained using the sample weight which was adjusted for oversampling, nonresponse and Korean population in 2008-2011, and standard error of estimates were estimated accounting for the complex survey design with SURVEY procedure. The age-specific prevalence of osteoporosis was calculated in males and postmenopausal females aged 50 years and older. Also, the prevalence of 50 years and older was calculated.
Exclusion criteria included those who reported any current disease that affects bone metabolism, including hyperthyroidism, hyperparathyroidism, chronic renal failure, bronchial asthma, rheumatoid arthritis, cancer, and objects which are being taken such as glucocorticoids or thyroid hormone.
18098 participants (8332 males and 9766 females) were included in the study.
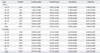
The anthropometric characteristics of participants, divided into 10-year age groups, are listed in Table 1. BMI tended to be greater in middle-aged (40-49) males and older females (60-69) than in young participants.
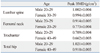
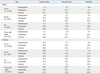
Table 2-1 lists age-specific mean BMD at the lumbar spine, femoral neck, femoral trochanter, and total hip. The mean BMD, according to residential area (urban or rural: seven metropolitan cities or six provinces), is also presented in Table 2-2. Table 3 shows the peak BMD at the lumbar spine, femoral neck, femoral trochanter, and total hip, according to different age spans. BMD at the lumbar spine, femoral neck, femoral trochanter, and total hip were lower in males than in females. For residential areas, overall BMD was lower in urban males aged 20 to 59 years than in rural males of the same age group. In female, overall BMD was lower in urban females 10 to 59 years of age than in rural females of the same age. The peak BMD of the lumbar spine, femoral neck, femoral trochanter, and total hip in Korean males reached at the ages of 20-29 years. In females, the peak BMD reached at different times in different skeletal findsites, 20-29 years of age at femoral neck, 30-39 years of age at lumbar spine, and 40-49 years of age at femur trochanter and total hip.
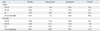
Table 4-1 shows the prevalence of osteoporosis in males and postmenopausal females aged 50 years and older. The prevalence of osteoporosis in Korea is 7.3% in males and 38.0% in females, aged 50 years and older. The prevalence of osteopenia in Korea is 46.5% in males and 48.7% in females aged 50 years and older. Table 4-2 lists the prevalence of osteoporosis in the same males and postmenopausal females aged, 50 years and older, according to specific skeletal sites. The prevalence of osteoporosis in the Korean population over age 50 at lumbar, femoral neck and total hip locations was 5.7%, 3.0%, and 0.7% in males and 30.1%, 23.1%, and 4.9% in females, respectively.
Fig. 1 illustrates the average BMD at the lumbar spine, femoral neck, femoral trochanter, and total hip in participants based on 10-year age groups, Fig. 2-1, 2-2 presents a comparison of reference curves for BMD at different skeletal sites in Korean and U.S. participants, and Fig. 3 presents a comparison of reference curves for BMD at different skeletal sites in Korean and Japanese females. The BMD at every measured skeletal site in Korean males and females was significantly lower than that of U.S. participants. The lumbar spine and femur BMD in Korean females of 20 to 49 years of age was significantly lower than in Japanese females, according to t-test.
Little epidemiological study data are available for osteoporosis prevalence in Korea. Therefore, this study is highly significant, because this is the first nationwide, cross-sectional survey, performed in Korea on osteoporosis incidence, under the supervision of the Ministry of Health and Welfare. In the present study, BMD at the femoral neck, femoral trochanter and total hip were significantly lower in females than in males. Residential area factors indicated that overall BMD was lower in urban males aged 20 to 59 years than in rural males of the same age group. In female, overall BMD was lower in urban females 10 to 59 years of age than in rural females of the same age. Geographic differences in BMD in the older-aged group were observed in our participants even though the Korean population predominantly consists of only one race. If future studies can analyze determinants of the differences in BMD, such as environmental or lifestyle factors, then the cause of these differences could be clarified.
The peak BMD of the lumbar spine, femoral neck, femoral trochanter, and total hip in Korean males reached at the ages of 20-29 years. In females, the peak BMD reached at different times in different skeletal sites: 20-29 years of age at femoral neck, 30-39 years of age at lumbar spine, and 40-49 years of age at femur trochanter and total hip. This finding indicates that Korean females attain peak BMD over a variable time interval depending on skeletal sites. This difference in peak BMD age among the skeletal sites is important for implementing preventive procedures for females, including actions for obtaining greater peak bone at sites, such as the femur. We suggest that this difference between genders might be caused by the difference in sex hormones and geometry of the hip axis between males and females.13,14 However, the determinants of the differences between the two genders remain un clear.
Prevalence of osteoporosis in Korea is 7.3% in males and 38.0% in females aged 50 years and older, and prevalence of osteopenia in Korea is 46.5% in males and 48.7% in females aged 50 years and older. The prevalence found in this study was higher than that reported in previous Korean cohort studies performed in rural settings, such as the Namwon and Ansung cohort studies.7,8,15 We suggest that this discrepancy resulted from the differences in general nutritional status and environment (such as sun exposure), according to each residential area. This difference may also result from the fact that T-scores was calculated using different normal reference data. Our study used a manufacturer-provided reference population based on a healthy Japanese-population-based osteoporosis study cohort.12,16,17,18 Since we assumed that the previous reference data of a Korean population were obtained from one rural residential area that did not represent the nationwide Korean population, we chose the reference data of the Japanese, another Asian race, as the best alternative plan. Therefore, considerable changes would occur if we adopted other reference population data in this study.4 According to skeletal sites, the prevalence of osteoporosis in the Korean population over 50 years of age at lumbar, femoral neck and total hip locations was 5.7%, 3.0%, and 0.7% in males and 30.1%, 23.1%, and 4.9% in females, respectively. The prevalence of osteoporosis at the lumbar spine was similar to the general prevalence in both genders. In comparison with other countries' reference curves, the BMD at every skeletal site in Korean males and females was significantly lower than that of the U.S. participants according to 2007-2010 NHANES. The lumbar spine and femur BMD in Korean females 20 to 49 years of ages was lower than in Japanese participants also. Previous studies revealed that the BMD of European population exceeds that of the Chinese; however, the difference would disappear after adjusting for height.5,6 The differences in our present study might have likely resulted from the different skeletal sizes common to each respective race. We should also consider nutrition and activity habits in each country. For example, people in Korea, spend less time in outdoor sports activities, therefore, they might not get enough sun exposure and gravity condition of bone to reach peak BMD as residents in other countries do.19 We should also have considered the nutritional differences including calcium intake between Korean, Japanese and U.S. participants.
Our study has several limitations. The first limitation is that no Korean reference values exist that differentiate between BMD values at different skeletal sites; such parameters would allow clinicians to make a more accurate diagnoses of osteoporosis in a Korean population. Additionally, the present data apply only to non-institutionalized Koreans. Institutionalized patients may have lower BMDs due to their conditions, especially if they are bed-ridden.
Even though there are limitations, our present study constitutes rare data to represent the nationwide Korean population. We expect to be able to estimate reference data through ongoing efforts of KNHANES in near future.
Figures and Tables
Fig. 1
Average bone mineral density (BMD) at the lumbar spine, femoral neck, femoral trochanter, and total hip in participants based on 10-year age groups.

Fig. 2-1
Comparison of reference curves for BMD at different skeletal sites in Korean and U.S. participants in males. BMD, bone mineral density.
Fig. 2-2
Comparison of reference curves for BMD at different skeletal sites in Korean and U.S. participants in females. BMD, bone mineral density.
Fig. 3
Comparison of reference curves for BMD at different skeletal sites in Korean and Japanese females. BMD, bone mineral density.
Table 2-2
Bone Mineral Density (g/cm2) at Various Skeletal Sites by Age Bracket-Regional Population (Urban: Seven Metropolitan Cities/Rural: Six Provinces)
References
1. Consensus development conference: diagnosis, prophylaxis, and treatment of osteoporosis. Am J Med. 1993; 94:646–650.
2. Koval KJ, Zuckerman JD. Functional recovery after fracture of the hip. J Bone Joint Surg Am. 1994; 76:751–758.

4. Kanis JA, McCloskey EV, Johansson H, Oden A, Melton LJ 3rd, Khaltaev N. A reference standard for the description of osteoporosis. Bone. 2008; 42:467–475.

5. Kao CH, Chen CC, Wang SJ. Normal data for lumbar spine bone mineral content in healthy elderly Chinese: influences of sex, age, obesity and ethnicity. Nucl Med Commun. 1994; 15:916–920.
6. Russell-Aulet M, Wang J, Thornton JC, Colt EW, Pierson RN Jr. Bone mineral density and mass in a cross-sectional study of white and Asian women. J Bone Miner Res. 1993; 8:575–582.

7. Kung AW, Ho AY, Ross PD, Reginster JY. Development of a clinical assessment tool in identifying Asian men with low bone mineral density and comparison of its usefulness to quantitative bone ultrasound. Osteoporos Int. 2005; 16:849–855.

8. Shin C, Abbott RD, Lee H, Kim J, Kimm K. Prevalence and correlates of orthostatic hypotension in middle-aged men and women in Korea: the Korean Health and Genome Study. J Hum Hypertens. 2004; 18:717–723.

9. Diab DL, Watts NB. Diagnosis and treatment of osteoporosis in older adults. Endocrinol Metab Clin North Am. 2013; 42:305–317.

10. Binkley N, Bilezikian JP, Kendler DL, Leib ES, Lewiecki EM, Petak SM, et al. Official positions of the International Society for Clinical Densitometry and Executive Summary of the 2005 Position Development Conference. J Clin Densitom. 2006; 9:4–14.

11. Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey Data, 2007-2010. National Center for Health Statistics;Available at: http://wwwn.cdc.gov/nchs/nhanes/search/nhanes07_08.aspx/, http://wwwn.cdc.gov/nchs/nhanes/search/nhanes09_10.aspx/.
12. Iki M, Kagamimori S, Kagawa Y, Matsuzaki T, Yoneshima H, Marumo F. Bone mineral density of the spine, hip and distal forearm in representative samples of the Japanese female population: Japanese Population-Based Osteoporosis (JPOS) Study. Osteoporos Int. 2001; 12:529–537.

13. Yang TS, Chen YR, Chen YJ, Chang CY, Ng HT. Osteoporosis: prevalence in Taiwanese women. Osteoporos Int. 2004; 15:345–347.

14. Cummings SR, Cauley JA, Palermo L, Ross PD, Wasnich RD, Black D, et al. Racial differences in hip axis lengths might explain racial differences in rates of hip fracture. Study of Osteoporotic Fractures Research Group. Osteoporos Int. 1994; 4:226–229.

15. Cui LH, Choi JS, Shin MH, Kweon SS, Park KS, Lee YH, et al. Prevalence of osteoporosis and reference data for lumbar spine and hip bone mineral density in a Korean population. J Bone Miner Metab. 2008; 26:609–617.

16. Kin K, Kushida K, Yamazaki K, Okamoto S, Inoue T. Bone mineral density of the spine in normal Japanese subjects using dual-energy X-ray absorptiometry: effect of obesity and menopausal status. Calcif Tissue Int. 1991; 49:101–106.

17. Yoshimura N, Hashimoto T, Morioka S, Sakata K, Kasamatsu T, Cooper C. Determinants of bone loss in a rural Japanese community: the Taiji Study. Osteoporos Int. 1998; 8:604–610.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download