Abstract
Purpose
To evaluate the effectiveness of digital rectal-compression immediately after transrectal prostate biopsy (P-bx) for improving the accuracy of prostate cancer (PCa) staging.
Materials and Methods
Between July 2008 and June 2010, 94 consecutive patients who had a radical prostatectomy were included in our retrospective analysis. The exclusion criteria included a history of previous P-bx and surgery, a biopsy performed in another hospital, a number of biopsy cores different from 12, or a condition interfering with bleeding assessment. The subjects were divided into two groups, compression and non-compression. All enrolled patients took magnetic resonance imaging (MRI) for PCa staging.
Results
The compression and non-compression groups were comparable with respect to several baseline characteristics. However, the total hemorrhage score of intraprostatic bleeding was significantly different between the groups, even with adjustment for the time from biopsy to MRI (compression:15.4±2.32, non-compression: 24.9±2.43, p<0.001). The intra-prostatic cancer location matching rate was higher in the compression group (78.0%) than in the non-compression group (70.2%) (p=0.011). Overall accuracy of staging in compression and non-compression groups was 84.7% and 77.3%, respectively.
Magnetic resonance imaging (MRI) plays an increasingly important role in the local staging of prostate cancer (PCa). However, conditions other than PCa, such as post-biopsy hemorrhaging, post-radiation and hormone therapy, scar/positional/inflammatory changes, and dystrophic changes can interfere with accurate MRI investigations.1-3 Among these factors, post-biopsy hemorrhaging offers substantial limitation to accurate detection of PCa after a prostate biopsy.4,5 Previous studies have shown that a waiting period of 3 weeks after biopsy can reduce the possibility of interference from intraprostatic hemorrhage.3,6 However, this is a passive approach, and our goal was to identify an active method to reduce intraprostatic hemorrhage after prostate biopsy.
We believe that prostate compression after prostate biopsy might help more accurately stage PCa because of the reduction in intraprostatic hemorrhage. Therefore, we evaluated the effects of digital rectal compression in patients who underwent ultrasound-guided transrectal prostate biopsy on PCa staging using MRI.
Between July 2008 and June 2010, 94 consecutive patients who had undergone a robot-assisted laparoscopic radical prostatectomy (RALRP) after ultrasound-guided prostate biopsy and prostate MRI investigation were enrolled in a retrospective analysis that was approved by our institution's review board.
All of the enrolled patients had biopsy-proven PCa. The exclusion criteria were a history of previous prostate biopsy and surgery; an interval from prostate biopsy to the MRI investigation of four weeks or more; an interval from MRI to surgery of more than 10 days; a history of use of 5-α reductase inhibitor within three months; a biopsy performed in another hospital; a number of biopsy cores different from 12; a positive nodal or bone metastasis based on preoperative imaging; or an additional condition, such as urinary tract stones, renal or bladder tumors, hemorrhoids, anal fissure, or rectal inflammatory disease, that could potentially cause hematuria or rectal bleeding and thus interfere with bleeding assessment.
All anticoagulant therapies, including aspirin/NSAIDs, warfarin, clopidogrel, and herbal supplements, were discontinued seven to ten days before the prostate biopsy. For patients with an underlying coagulopathy or for those taking warfarin, prostate biopsy was delayed until the International Normalized Ratio had been corrected to less than 1.5. Prophylactic oral ciprofloxacin (500 mg) was administrated once daily 30 to 60 minutes before the biopsy and was continued for two to three days after the procedure.
Patients self-administered a cleansing enema the night before the biopsy. No local anesthesia was administered to avoid any possible interference from bleeding.
For the procedure, patients were placed in a right lateral decubitus position. An intra-rectal lidocaine jelly injection was used as a topical analgesic. A spring-driven 18-gauge needle core biopsy gun was used for prostate tissue biopsy via a needle guide that was attached to the ultrasound probe. A systematic 12-core biopsy was performed for each patient by a urologist with six years of experience. The enrolled subjects were divided into two groups: a compression group (48 patients) and non-compression group (46 patients). After biopsy, digital rectal compression was immediately performed for five minutes in the compression group. This compression was performed only during the second year of the study (July 2009-June 2010).
All of the patients were imaged using a 3.0T MRI system (Intera Achieva 3.0T, Philips Medical System, Best, the Netherlands) equipped with a six-channel phased-array coil. No endorectal coil has been used because of discomfort of patients without no significant effectiveness.8 This imaging was performed prior to the radical prostatectomy. All of the patients underwent diffusion-weighted imaging (DWI) in addition to the imaging sequences as part of a routine prostate MRI protocol. T2-weighted turbo spin-echo images were acquired in three orthogonal planes (axial, sagittal, and coronal). The T2-weighted imaging scan parameters were TR/TE, 3300 to 3800/80 to 100 milliseconds; slice thickness, 3 mm; interslice gap, 0.3 mm; 512×360 matrix; field of view (FOV), 20 cm; number of signals acquired, 3; and sensitivity encoding (SENSE) factor 2. Axial T1-weighted THRIVE sequences (3 mm slice thickness; FOV, 20 cm) were acquired to detect artifacts from the biopsy and to assess the lymph nodes. Axial DWI was obtained using a single-shot echo planar imaging technique with the following imaging parameters: TR/TE, 2300 to 3000/63 to 65 milliseconds; slice thickness, 3 mm; interslice gap, 1 mm; matrix, 80×80; FOV, 20 cm; SENSE factor 2; number of signals acquired 4. Diffusion-encoding gradients were applied in the axial directions of motion-probing gradients as bipolar pairs at b values of 0 and 1000 s/mm2. ADC DWI maps were automatically constructed on a pixel-by-pixel basis.
All images were retrospectively reviewed by two radiologists with 6 and 11 years of experience in interpreting prostate MRI results (J.H.K and J.J.J, respectively) and 2 years of experience in DWI. Two radiologists conducted a consensus review of the MR images obtained for all patients and determined the degree and number of hemorrhages on three axial MR images for each patient, selected using the following methods. First, the axial image containing the verumontanum area was selected as a standard plane. Second, a base and apex plane 10 mm from the standard plane was selected. Third, each plane was divided into four peripheral zones and two transitional zones. Each hemorrhagic prostate segment was scored according to the diameter of the segment on a scale of 0 to 3 as follows: 0=none, 1=greater than 0 mm and less than 5 mm, 2=greater than 5 mm and less than 10 mm, 3=greater than 10 mm. In each segment, cancer foci were counted using a two-point scale, where 0=<50% and 1=>50% chance of cancer. A hemorrhage was defined as a high-signal intensity on a T1-weighted image and a low-signal intensity on a T2-weighted image. The observer was unaware of the pathology results. These techniques were used for similar prostate MRI based study from December 2007.7
Previously prepared pathology slides were retrospectively reviewed by one pathologist (B.J.L.). The slides were chosen from consecutive pathology files using the same criteria as the radiology interpretations. The pathologist outlined the region of cancer and hemorrhage on each slide. The slides were then digitized and saved as a jpeg image. Based on these digitized slides, each tumor and hemorrhage regions were scored by the pathologist (B.J.L.) in the same manner as the radiology interpretations. The pathologist was blinded to the MRI results. We validated the limited sensitivity of MRI9 in order to make a proper radiologic-pathologic correlation. Under the cross-sectional area of the fixed specimen, a region with greater than 0.1 cm diameter was considered to be a meaningful lesion. Hemorrhage was defined as the presence of red blood cells outside the identifiable blood vessels, especially in the interstitium and glandular lumen. The urologist (K.K.P.) independently reviewed the pathology and radiology scoring results. Finally, we analyzed for concordance for tumor location between these results by time period between the biopsy and MRI.
The relationship between the total hemorrhage score and the period from the biopsy to MRI was assessed using a Pearson's correlation test. Differences in patient characteristics between the two groups were analyzed using a t-test and Pearson's chi-square statistical test. Period-adjusted hemorrhage scores for the two groups were compared using the ANCOVA test separately. When the two groups were divided into 4 groups according to the period between prostate biopsy and MRI, separate groups were compared using the t-test. All statistical tests were conducted using SAS (version 9.0), and all tests were two sided, with a p-value <0.05 being considered statistically significant.
The compression and non-compression groups were comparable with regard to age, serum prostate-specific antigen level, prostate volume, tumor volume involvement, pathologic T stage, and Gleason score sum (Table 1). There was a significant difference in hemorrhage score between the two groups up to 24 days after biopsy after adjusting for the period from biopsy to MRI (ANCOVA test, compression groups: 15.4±2.32, non-compression group: 24.9±2.43, p<0.001). Total hemorrhage scores were negatively correlated with the time between biopsy and MRI (r=-0.345, p=0.031).
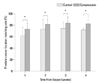
To evaluate the accuracy of PCa stage using MRI, cancer location data obtained through MRI were compared with pathologic data. The intra-prostatic cancer location matching rate was significantly increased in the compression group compared to the non-compression group (Fig. 1). Matching rates for intraprostatic cancer location were 78.0% in the compression groups and 70.2% in the non-compression groups (t-test, p=0.011). Matching rate of extracapsular extension was 82% in the compression group and 75% in the non-compression group (t-test, p=0.032). Matching rate about seminal vesicle invasion was observed to be 90% in the compression group and 85% in the non-compression group cases (t-test, p=0.046). Overall accuracy of PCa staging obtained through MRI was 84.7% in the compression groups and 77.3% in the non-compression groups (t-test, p=0.037).
To determine the extent of tumor and the choice of management, accurate tumor staging is essential. The major role of MRI in PCa is to assist with local staging of the disease. Prostate carcinoma usually demonstrates lower signal intensity of MR images, as compared to the peripheral zone. The changes of signal intensity are nonspecific. In patiens with tumors, post-biopsy hemorrhage, post-radiation and hormone therapy, scar/positional/inflammatory changes, and dystrophic changes, prostate MR images would demonstrate show low signal intensity within the peripheral zone on T2-weighted images.1-3
In a patient who is diagnosed with PCa via a prostate biopsy, post-biopsy hemorrhaging is a major factor that interferes with accurate MR image interpretation. Reducing the risk of post-biopsy hemorrhaging, therefore, is necessary in order to minimize this interference. First, all anticoagulant therapy should be discontinued before the biopsy. For those patients coagulation problem such as coagulopathy or taking anticoagulant, a prostate biopsy should be delayed until normal coagulation had been restored.10 Second, several studies have reported that post-biopsy hemorrhaging diminishes with time.3,6,11 We also observed a statistically significant negative correlation between the sum of the hemorrhage score and the time from the biopsy in our previous and current study.7 However, some authors argue that post-biopsy hemorrhaging is not significantly reduced until 55 days after the biopsy.12,13 Third, another technique that is less influenced by post-biopsy hemorrhage than conventional MRI can be used.12,14,15
We believe that all three of the above-mentioned methods can passively reduce post biopsy hemorrhage. Therefore, we sought a method to reduce post biopsy intraprostatic hemorrhage.
Digital rectal compression is a well-known method for reducing rectal bleeding after prostate biopsy.16 However, our results demonstrate that this method can also reduce intraprostatic hemorrhage and increase the accuracy of MRI. In this study, we found that compression can reduce the amount of post biopsy hemorrhage. The accuracy of tumor detection in the compression group was 78.0%, which is significantly superior to the accuracy of detection in the noncompression group (70.2%). Therefore, reducing hemorrhage through digital rectal compression makes it significantly more accurate for the detection of PCa. We aimed to develop an approach to actively increase the accuracy of MRI staging for PCa, rather than passively waiting for 2 weeks. Based on our results, we recommend the routine use of digital rectal compression after prostate biopsy to increase the accuracy to detect PCa.
We believe that digital rectal compression has a few additional merits. First, rectal compression may reduce surgical difficulty. Some authors have reported that post biopsy hemorrhage may induce operative difficulty. Hong, et al.13 reported that the degree of post biopsy hemorrhage detected by MR image has a significant association with operative outcome such as operative time, estimated blood loss, and return of erectile function in patients who received RALRP. However, as shown in this study, if digital rectal compression is conducted in patients after prostate biopsy, operative difficulty might decrease because digital rectal compression could reduce intraprostatic hemorrhage. Second, some authors have argued that conventional MRI is significantly affected by the amount of post biopsy hemorrhage.3,14 Rectal compression may shorten the period during which there is interference in the interpretation of the prostate by conventional MRI. In this study, using multiparametric MRI, the timing of MRI did not affect the accuracy of PCa staging. Because multiparametric MRI usually has a greater sensitivity and specificity than conventional MRI, we believe that interpretation of MRI is less influenced by post biopsy hemorrhage.7,12,14,15 However, if the institute uses conventional MRI rather than multiparametric MRI for PCa staging, rectal compression may reduce the development of intraprostatic hemorrhage at biopsy. Therefore, the interval between biopsy and prostate MRI can be shortened due to the decrease in the absolute amount of developing hemorrhage, and postbiopsy hemorrhage will disappear more quickly.
There are some limitations in our study. First, the period between biopsy and MRI was a maximum of 24 days. Therefore, we did not evaluate the effects of compression over more than 24 days. Second, in order to achieve an objective interpretation, three investigators were involved. Because the results from the radiologist and pathologist were integrated by the third investigator, it is possible that an increased level of observer error might have been introduced into the final results. Third, this was a retrospective study. Even if the most similar MRI and pathology sections were selected, there were still some inconsistencies between pathology and radiology sections.
In conclusion, this study demonstrates that digital rectal compression immediately after prostate biopsy can reduce intraprostatic hemorrhage. the accuracy in detecting PCa can be improved by performing transrectal digital compression only immediately after biopsy. Therefore, we believe that digital rectal compression should be carried out after prostate biopsy.
Figures and Tables
References
1. Schiebler ML, Tomaszewski JE, Bezzi M, Pollack HM, Kressel HY, Cohen EK, et al. Prostatic carcinoma and benign prostatic hyperplasia: correlation of high-resolution MR and histopathologic findings. Radiology. 1989. 172:131–137.

2. Schiebler ML, Schnall MD, Pollack HM, Lenkinski RE, Tomaszewski JE, Wein AJ, et al. Current role of MR imaging in the staging of adenocarcinoma of the prostate. Radiology. 1993. 189:339–352.

3. White S, Hricak H, Forstner R, Kurhanewicz J, Vigneron DB, Zaloudek CJ, et al. Prostate cancer: effect of postbiopsy hemorrhage on interpretation of MR images. Radiology. 1995. 195:385–390.

4. Chelsky MJ, Schnall MD, Seidmon EJ, Pollack HM. Use of endorectal surface coil magnetic resonance imaging for local staging of prostate cancer. J Urol. 1993. 150(2 Pt 1):391–395.

5. Schnall MD, Imai Y, Tomaszewski J, Pollack HM, Lenkinski RE, Kressel HY. Prostate cancer: local staging with endorectal surface coil MR imaging. Radiology. 1991. 178:797–802.

6. Ikonen S, Kivisaari L, Vehmas T, Tervahartiala P, Salo JO, Taari K, et al. Optimal timing of post-biopsy MR imaging of the prostate. Acta Radiol. 2001. 42:70–73.

7. Park KK, Lee SH, Lim BJ, Kim JH, Chung BH. The effects of the period between biopsy and diffusion-weighted magnetic resonance imaging on cancer staging in localized prostate cancer. BJU Int. 2010. 106:1148–1151.

8. Kim BS, Kim TH, Kwon TG, Yoo ES. Comparison of pelvic phased-array versus endorectal coil magnetic resonance imaging at 3 Tesla for local staging of prostate cancer. Yonsei Med J. 2012. 53:550–556.

9. Kirkham AP, Emberton M, Allen C. How good is MRI at detecting and characterising cancer within the prostate? Eur Urol. 2006. 50:1163–1174.

10. Douketis JD. Perioperative anticoagulation management in patients who are receiving oral anticoagulant therapy: a practical guide for clinicians. Thromb Res. 2002. 108:3–13.

11. Qayyum A, Coakley FV, Lu Y, Olpin JD, Wu L, Yeh BM, et al. Organ-confined prostate cancer: effect of prior transrectal biopsy on endorectal MRI and MR spectroscopic imaging. AJR Am J Roentgenol. 2004. 183:1079–1083.

12. Tamada T, Sone T, Jo Y, Yamamoto A, Yamashita T, Egashira N, et al. Prostate cancer: relationships between postbiopsy hemorrhage and tumor detectability at MR diagnosis. Radiology. 2008. 248:531–539.
13. Hong SK, Kim DS, Lee WK, Park H, Kim JK, Doo SH, et al. Significance of postbiopsy hemorrhage observed on preoperative magnetic resonance imaging in performing robot-assisted laparoscopic radical prostatectomy. World J Urol. 2010. 28:721–726.

14. Kaji Y, Kurhanewicz J, Hricak H, Sokolov DL, Huang LR, Nelson SJ, et al. Localizing prostate cancer in the presence of postbiopsy changes on MR images: role of proton MR spectroscopic imaging. Radiology. 1998. 206:785–790.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download