INTRODUCTION
Infants and children undergoing cardiac surgery with cardiopulmonary bypass (CPB) frequently present with post-bypass coagulation abnormalities that are primarily attributed to hemodilution from a larger volume of pump priming relative to patient's blood volume.
1-
3 Decreased concentration of coagulation factors, particularly fibrinogen, is known to be a major cause of post-bypass coagulation abnormalities.
4,
5 Fresh whole blood, collected 48 hours (h) before surgery, has an adequate concentration of coagulation factors, including fibrinogen, can provide adequate volume replacement and is an example of blood product that has been considered ideal for pump priming.
6 However, reports evaluating the hemostatic benefit of the fresh-collected blood products for pump priming in neonates or infants undergoing CPB are divergent.
7,
8 Furthermore, fresh-collected blood products are not readily available at most institutions. Given that the most convenient alternative source of fibrinogen is fresh frozen plasma (FFP), the use of FFP in pump priming in infants weighing <8-10 kg was previously shown to increase fibrinogen levels after CPB.
9,
10 While neonates and small infants are most vulnerable to post-bypass coagulation derangement,
11-
13 it is necessary to evaluate the effects of FFP in pump prime for pediatric cardiac surgery on post-bypass hemostasis in a wide variety of patients, including older children or those undergoing repeat sternotomy. Additionally, it is important to use not only laboratory measurements, including fibrinogen level, but also functional evaluations of rotational thromboelastometry (ROTEM®, TEM Innovations, Munich, Germany). The aim of this prospective investigation is to evaluate the effects of FFP in pump priming for cardiac surgery in infants and children on the post-bypass coagulation profiles.
MATERIALS AND METHODS
After obtaining approval from local ethics committee and written consent from parents, 123 pediatric patients, aged 1 month to 16 years who were scheduled for elective cardiac surgery with CPB were recruited for this investigation. Exclusion criteria were as follows: neonate (<1 month of age), previously diagnosed coagulation disorders of non-cardiovascular origin, and any metabolic disorder leading to abnormalities in plasma protein profiles. Additionally, if a patient was transferred to the intensive care unit (ICU) with the chest open for hemodynamic instability, or required surgical re-exploration for postoperative bleeding within 24 h after initial surgery, that patient was also excluded from the analysis. Using a sealed envelope method, patients were randomly allocated into either control or treatment groups, which received 20% human albumin or FFP in pump priming, respectively. Coagulopathy after CPB is associated with patient age;
12 therefore, all patients were divided into infants (younger than 12 months) or children (older than 1 year) and the control and treatment groups within each age population were compared as follows: infants control vs. infants treatment, and children control vs. children treatment. To assess an individual surgical risk, an Aristotle Basic Complexity score was assigned to all patients, based on the main operation designated by the surgeon.
14 With the exception of perfusionists, anesthesiologists, surgeons, and personnel working in the ICU were all blinded to the designated group of a patient.
Anesthesia was induced with intravenous ketamine (1-2 mg/kg) with vecuronium (0.1-0.2 mg/kg) for muscle relaxation. Maintenance of anesthesia was achieved with a continuous infusion of ketamine (20-25 µg/kg/min), supplemented by intermittent inhalation of sevoflurane (<1.2 vol%) in oxygen and air before the initiation of CPB. For maintenance of anesthesia during CPB, fentanyl (20-30 µg/kg) and vecuronium (0.1-0.2 mg/kg) were given at the beginning of CPB and at the initiation of rewarming. Before cannulation of CPB, systemic anticoagulation was accomplished with IV heparin (300 units/kg of body weight). During CPB, additional doses of heparin were given to maintain an activated clotting time (ACT) of >450 sec. For heparin reversal, an initial dose of protamine was calculated to equal the pre-bypass dose of heparin. Additional doses of protamine were given until ACT returned to the baseline values.
The pump priming solution, the volume of which was calculated on the basis of body weight, included crystalloid fluid (Plasma solution A®, CJ Pharma, Seoul, Korea) and packed red blood cells (PRBC) to obtain a predictive hematocrit value of 30% after dilution. To maintain the colloid oncotic pressure, either 20% human albumin (50-100 mL) or FFP (1-2 units) was added to pump priming for patients randomly allocated to control or treatment groups, respectively. Volume differences between 20% human albumin and FFP were eliminated with the crystalloid component to reach the calculated volume of pump priming. Medications in pump priming included 20% mannitol (5 mL/kg of body weight), heparin (1 unit) and 8.4% NaHCO3 (0.4 mL) per 1 mL of priming volume, CaCl2 (60-90 mg per unit of stored PRBC), and 5% dextrose-in-water (10 mL/kg of body weight when the patient weight was <30 kg). The CPB circuits contained a hard-shell venous reservoir and a hollow-fiber membrane oxygenator (Capiox Baby Rx®, Terumo, Tokyo, Japan), which were adapted to patient size, an arterial filter, and a roller pump. Non-pulsatile blood flow was maintained at 2.0-2.4 mL/min/m2 with mild hypothermia of 28-32℃ measured rectally. The target temperature of hypothermia was determined by the surgeon according to the planned surgical procedure. Cold, intermittent blood cardioplegia, prepared during CPB, was used for myocardial protection. The α-stat strategy was applied throughout the CPB period. To maintain the hematocrit >28% during CPB period, additional PRBC was given to the CPB circuit and/or ultrafiltration was performed at the discretion of the assigned perfusionist. In principle, modified ultrafiltration (MUF) in arteriovenous fashion was done for 5-10 min after weaning from CPB in every patient. However, in 33 patients (27%), MUF could not be done because clinical conditions didn't permit. Additional transfusion of blood products after heparin reversal was at the discretion of the anesthesiologist and intensivist who were responsible for patient care in the operating theater and ICU, respectively.
Study protocol
Laboratory tests, including hemoglobin concentration and hematocrit (Hb/Hct), platelet count, functional fibrinogen level, prothrombin time (PT) and activated partial thromboplastin time (aPTT) were done as routine preoperative work-ups. Measurements of arterial blood gas (ABG), ACT and rotational thromboelastogram (ROTEM®, TEM Innovations, Munich, Germany) were performed before skin incision as baseline values. ROTEM measurements included INTEM, EXTEM and FIBTEM for analysis of intrinsic and extrinsic coagulation pathways and fibrinogen activity, respectively. Except for FIBTEM, which contains amplitude at 10 min after CT (A10) and maximal clot firmness (MCF) only, all ROTEM measurements have the following parameters in common: clotting time (CT), A10, clot formation time (CFT), α angle, and MCF. After weaning from CPB and heparin reversal, Hb/Hct, platelet count, functional fibrinogen level, ABG, ACT and ROTEM measurements were repeated. Surgical blood loss and transfusion requirements during the surgery were calculated and recorded. During ICU stay, chest tube drainage and transfusion requirements were recorded for the initial 24 h. At the first postoperative day, laboratory tests, including Hb/Hct, platelet count, functional fibrinogen level, PT, aPTT, and ROTEM measurements were performed for follow-up.
Statistical analysis
Based on previous investigations, power analyses suggested that the inclusion of >20 patients per group would enable detection of a >30 mL/kg difference in mean chest tube drainage during 24 h ICU stay between the control and treatment groups with a chance of 80% (α=0.05, β=0.2). Categorical variables are presented as the numbers of patients (percent), and a χ2-test was used for statistical analysis. Continuous variables are presented mean±SD or median (interquartile range), and statistically evaluated with Student's t-tests or Mann-Whitney U tests, as appropriate. A p-value of <0.05 was considered statistically significant.
RESULTS
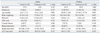
A total of 123 patients were initially recruited, but one in the infant treatment group and one patient in the children control group were excluded as they required delayed sternal closure for hemodynamic stability. In total, 121 infants and children were finally included for analysis. Patient characteristics, and surgical and bypass data were comparable between the control and treatment groups of infants and children (
Table 1).
Diagnosis and corresponding surgery for infants are presented in
Table 2-1, showing no differences between the control and treatment groups. In children, there were no differences for surgical procedures performed between the control and treatment groups (
Table 2-2).
Preoperatively, Hb/Hct, platelet count, functional fibrinogen level, PT and aPTT were all comparable between the control and treatment groups of infants and children. After protamine administration, Hb/Hct were significantly higher in the infants treatment group than those in the infants control group, however, comparable between the children control and children treatment groups. Functional fibrinogen levels were greater in the treatment groups of infants and children after heparin reversal. Thereafter, there were no differences in Hb/Hct, platelet count, fibrinogen level, PT and aPTT between the control and treatment groups of infants and children at 24 h in the ICU (
Table 3-1). The ACT data measured before skin incision and after heparin reversal are presented in
Table 3-2, showing no significant differences between the control and treatment groups of infants and children, except for significantly longer ACT measurement after protamine administration in the infant control compared to the infant treatment group.
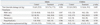
ROTEM measurements performed before skin incision were comparable between the infants control and infants treatment groups. After heparin reversal, however, shorter CFT and greater α for INTEM and EXTEM, and greater A10 and MCF for all three ROTEM measurements were shown in the infants treatment group. However, at 24 h in the ICU, there were no differences in ROTEM values between the infants control and infants treatment groups (
Table 4-1). In children, baseline ROTEM values did not differ between the control and treatment groups. INTEM measurements were shown to be comparable between the children control and children treatment groups after protamine administration, as well as at 24 h in the ICU. For EXTEM measurements, slightly shorter CFT and greater α were observed in the children treatment group after protamine administration, then no differences were shown between the children control and children treatment groups at 24 h in the ICU. For FIBTEM measurements, A10 and MCF were greater in the children treatment group after heparin reversal. MCF was still greater in the children treatment group at 24 h in the ICU, but statistical significance was marginal (
p=0.048) (
Table 4-2).
It is reasonable that the amount of FFP added into the pump prime was significantly greater in the treatment groups of infants and children. No differences were found in the amount of PRBC in pump priming between the control and treatment groups of infants and children.
The amount of additional PRBC given to the CPB circuit to maintain a hematocrit of >28% was significantly greater in the infants treatment group. After heparin reversal, PRBC transfusion was greater in the Infants treatment group (
p=0.047). But FFP transfusion was greater in the infants control group (
p=0.042) after heparin reversal. There were no differences in the transfusion of platelets and autologous salvaged blood between the infants control and infants treatment groups, as well as in the total amount of intraoperative bleeding after heparin reversal. In total, intraoperative transfusion requirements after heparin reversal were greater in the infant treatment group. After excluding FFP in the pump prime, however, the amount of transfusion after protamine administration was comparable between the infants control and infants treatment groups (
Table 5-1).
In children, there were no differences in additional PRBC during CPB and PRBC transfusion after heparin reversal between the control and treatment groups. But FFP transfusion was significantly greater in the children control group after protamine administration. Transfusion of platelets and autologous salvaged blood did not differ between the children control and children treatment groups. Total amount of intraoperative transfusion requirements were also comparable between the children control and children treatment groups. Total transfusion requirements without FFP in pump priming were greater in the children control group but the difference was not statistically significant (
p=0.06) (
Table 5-1).
During 24 h of ICU stay, there were no differences found in the total amount of transfusion requirements, as well as in the transfusion requirements of individual blood products between the control and treatment groups of infants and children. Chest tube drainage for 24 h in the ICU was also comparable between the control and treatment groups of infants and children (
Table 5-2).
Perioperatively, there were no significant differences in the ABG measurements between the control and treatment groups of infants and children (data not shown).
DISCUSSION
Inclusion of FFP in pump priming for congenital heart surgery was shown to significantly lessen hemodilution-induced reductions in fibrinogen level immediately after heparin reversal, resulting in improvements in thromboelastometry parameters reflecting clot formation and firmness in infants and children. These beneficial effects of FFP in pump priming, however, were not sustained until 24 h in the ICU, and any clinical benefits of transfusion requirements and/or postoperative bleeding were not clearly demonstrated.
Post-CPB coagulopathy can be described as "dilutional",
1-
3 and hypofibrinogenemia has been demonstrated to be a major cause.
4,
5 In this study, platelet count and functional fibrinogen level were all reduced immediately after heparin reversal in the control and treatment groups of infants and children even though hemodilution was considered to be well-compensated with modified ultrafiltration, evidenced by comparable Hb/Hct measurements pre- and post-CPB. In the treatment groups, however, fibrinogen levels were significantly less reduced than those in the control groups of infants and children. This difference could be attributed to the inclusion of FFP in pump priming, as previous investigations had demonstrated.
9,
10
To maintain a target Hct of 28%, significantly more PRBCs were added into the CPB circuit in the infant treatment group, which resulted in significantly higher, but clinically acceptable Hb/Hct measurements immediately after heparin reversal, compared to the infant control group. Reasonably, more FFP was included into pump prime in the treatment groups of infants and children. After heparin reversal, however, significantly greater transfusions of FFP were needed intraoperatively in the control groups of infants and children. Unlike in children, overall intraoperative transfusion requirements were significantly greater in the infants treatment group. The amount of FFP included in pump priming presumably made such a difference, because transfusion requirement excluding FFP in pump priming was comparable between the infants control and infants treatment groups. Of the transfusion requirements in the ICU, total amounts were numerically greater in the control groups of infants and children, but without statistical significances. Most of the differences in the transfusion requirements in the ICU in infants may be attributed to the greater requirement for FFP in the control group. After all, for patients in control groups, more FFP might be given after heparin reversal in the ICU and intraoperatively in infants and children, respectively. This means that FFP transfusion was done as a part of the postoperative hemostatic management at the discretion of the assigned physician, which may have resulted in comparable intraoperative bleeding and chest tube drainage in the ICU between the control and treatment groups of infants and children. We could not, however, confirm this within the scope of analyses in this study.
Although coagulation profiles were evaluated only with blood cell counts and/or fibrinogen level, inclusion of FFP in pump priming was previously evaluated in neonates (<8-10 kg) undergoing congenital heart surgery with the goal of determining the effects on transfusion and blood loss.
9,
10 These previous studies demonstrated that the use of FFP in pump priming only augmented post-CPB fibrinogen level, and did not reduce transfusion requirements and/or chest tube drainage, similar to the results of this study using hematologic assays. Thus, it is important to adopt a certain method to evaluate the coagulation profiles functionally. One study performed the functional evaluations with thromboelastography (TEG) in pediatric patients after CPB, but found no differences in TEG parameters between groups.
9 In this study, however, ROTEM is a reagent-assisted method with the ability to examine all aspects of the coagulation pathways, including intrinsic and extrinsic pathways and fibrinogen activity. Additionally, it has been shown that ROTEM is able to identify post-bypass coagulation abnormalities more quickly and with higher specificity, compared to standard coagulation tests.
15,
16
In infants, ACT measurements were nearly restored to the original levels measured before skin incision in both control and treatment groups. With respect to ROTEM measurements, however, clot initiation was delayed because CT in INTEM measurements was prolonged to nearly twice the upper normal limit after heparin reversal in both control and treatment groups, which is considered to be a residual effect of heparin. Clot formation was also delayed after heparin reversal because of prolonged CFT and reduced α-angle in both control and treatment groups. FFP in pump priming significantly improved delayed clot formation, which was shown by findings of significantly less altered CFT and α-angle in the treatment group. Clot firmness was reduced in both control and treatment groups after heparin reversal. However, the use of FFP in pump priming also significantly improved clot firmness in the infants treatment group, as evidenced by less reduced TEG parameters reflecting clot firmness, A10 and MCF. Reduced clot firmness demonstrated in both INTEM and EXTEM measurements could be attributed to platelet or fibrinogen deficiency. A reduction in clot firmness shown in this study was primarily attributed to fibrinogen deficiency because clot firmness was also measured to be reduced in FIBTEM, which utilizes platelet inhibition reagent. Moreover, platelet count was similarly reduced in both control and treatment groups after heparin reversal, but the fibrinogen level was significantly less reduced in the treatment group. Prevention of fibrinogen reduction in the treatment group may explain why clot firmness was significantly less affected by a dilution coagulopathy. Previously, it was demonstrated that fibrinogen level was important for clot strength especially in the setting of platelet deficiency.
17
In children, a similar pattern of dilutional coagulopathy to that of infants, delayed clot initiation and formation, and reduced clot firmness after heparin reversal. In contrast, there were no significant differences between the children control and children treatment groups in the coagulation profile of the intrinsic pathway, evaluated with INTEM measurements. In the consideration of less elevated CT in INTEM measurements, an equal restoration of ACT and much less reduced platelet count in both control and treatment groups after protamine administration, children undergoing congenital heart surgery were shown to be less affected by residual heparin and hemodilution, compared to infants. As previously demonstrated, post-CPB coagulopathy was shown to be dependent on age.
11-
13 For extrinsic pathway measurements, clot formation was shown to be significantly less delayed in the children treatment group, evidenced by significantly less altered CFT and α-angle after heparin reversal. Fibrinogen activity, evaluated by FIBTEM measurements, was significantly less affected in the children treatment group, demonstrated by significantly less reduced A10 and MCF values. As in infants, reduced clot firmness in the children control group could be attributed to fibrinogen deficiency, as parameters reflecting clot firmness were reduced in all ROTEM measurements after heparin reversal. In the children treatment group, however, clot firmness measured with FIBTEM was reduced from baseline value, but was nearly within the normal range. Furthermore, fibrinogen level was significantly less reduced than that in the children control group while platelet count between the control and treatment groups were comparable. These results suggest that the use of FFP in pump priming has a beneficial effect on clot firmness after heparin reversal in children undergoing cardiac surgery with CPB.
Beneficial effects of FFP in pump priming were not sustained until 24 h postoperatively, as evidenced by the lack of significant differences in hematologic and ROTEM data recorded at 24 h in the ICU in both infants and children. Furthermore, clinical benefits to reduce transfusion requirements and/or postoperative bleeding were not clearly demonstrated. As mentioned above, FFP transfusion in the control groups of infants and children were done immediately after heparin reversal and during ICU stay for postoperative hemostasis. As reported previously, a certain positive clinical effect would have been found if the patients were categorized with the complexity of the surgery or cyanosis.
9 In fact, however, the complexity of the surgery could be a subjective measurement made by the surgeon and the proportion of cyanotic patients was too small to be separately analyzed in this study.
In this study, we found that commonly used clinical parameters of coagulation profiles have certain limitations. Important components of the coagulation pathway, including platelet count and fibrinogen level, were shown to be quantitatively reduced in spite of sufficient restoration of Hb/Hct measurements by means of free water removal, such as modified ultrafiltration. Likewise, sufficient restoration of ACT to the preoperative value was not shown to guarantee full recovery of clot initiation, as ROTEM measurements remained elongated. Actually, ROTEM was demonstrated to be useful to exclude residual heparin effects on elongated ACT after CPB in a previous pilot study.
18 In this study, functional evaluation of blood coagulation with ROTEM measurements provided a more detailed picture of postoperative hemostasis, including more augmented effects of residual heparin in infants, and clot formation and clot strength measurements that were less affected by dilutional hypofibrinogenemia with FFP in pump priming.
There are some limitations in this study. First, reference values for qualitative and quantitative methods of blood coagulation, especially ROTEM measurements, have not been specified in a pediatric population. Therefore, adult values had to be used in this study.
19 Second, plasma oncotic pressures of pump priming were assumed to be comparable between the control and treatment groups by reducing the amount of crystalloid included in pump priming to obtain a volume difference between 20% albumin and FFP. Considering that 20% albumin has three times the level of oncotic pressure with the one third of volume of FFP, it would be acceptable clinically. Additionally, it was previously reported that oncotic pressure of pump priming did not affect postoperative findings including transfusion requirements and postoperative bleeding.
20 Third, to confirm the residual effects of heparin, it is better to use HEPTEM of ROTEM measurements, which additionally uses heparinase. However, this was not commercially available when this study was being conducted. Most of all, most of transfusions were done based on empirical decision of the assigned physician due to lack of consensus on transfusion threshold in pediatric patients after cardiac surgery. Use of predetermined transfusion guidelines based on point-of-care tests, such as ROTEM, would allow for more effective means to predict transfusion requirements, as in other investigations on the use of ROTEM measurements for determining transfusion requirements.
21
In conclusion, inclusion of FFP in pump priming for congenital heart surgery in infants and children was shown to improve hemodilution-related coagulation dysfunction immediately after weaning from CPB and heparin reversal. However, beneficial effects were not shown to be continued until 24 h in the ICU, and clinical benefits were not clearly evident. To evaluate clinical and functional benefits of FFP in pump priming, large, randomized investigations with risk stratification are necessary in the future. Furthermore, it is necessary to adopt predetermined, clinical transfusion guidelines based on point-of-care tests, which can provide information not only on the quantitative aspects, but also on the qualitative aspects of coagulation profiles.









 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download