Abstract
Purpose
The laryngeal mask airway (LMA) is a supraglottic airway device designed to seal around the laryngeal inlet. A controlled study was designed to compare the effectiveness and complications in inserting the LMA when the cuff is fully deflated and partially inflated.
Materials and Methods
American Society of Anesthesiologists physical status I or II 172 female patients scheduled for gynecologic procedures were included in this study. Patients were randomly allocated into one of the two groups; fully deflated (n=86) and partially inflated group (n=86). A size #4 LMA was inserted. The number of attempts, time taken for successful insertion, grade of leak, grade of fiberoptic view, and complications were evaluated.
The laryngeal mask airway (LMA) is a supraglottic airway device that is designed to seal around the laryngeal inlet. The LMA is handled with greater ease by less skillful personnel,1,2 and is known to have a low complication rate. LMA insertion not only allows adequate airway control during both controlled and spontaneous ventilation, but also airway patency can be maintained under less anesthetic doses compared to endotracheal intubation.3,4 For these reasons, the LMA is frequently used for airway management in ambulatory anesthesia.5
The LMA is used widely in pediatric anesthesia due to frequent ambulatory surgery in children. Therefore, the research on LMA insertion techniques has been carried out mostly in the field of pediatric anesthesia. Kundra, et al.6 demonstrated that the lateral approach with a partially inflated cuff as an alternative LMA insertion technique improved the ease and success of LMA insertion in children compared with the standard Brain technique. And Ghai, et al.7 and Nakayama, et al.8 also reported that the rotational technique with the LMA cuff partially inflated is associated with a higher success rate of insertion and lower incidence of complications in children. Meanwhile, in adult patients, there is a report that inserting the LMA with the cuff partially inflated is likely to be more successful than with the cuff fully deflated.9 On the other hand, insertion of the LMA with the cuff partially inflated has been shown to be less successful than with the cuff fully deflated.10
However, all the above-mentioned studies were carried out without controls on neuromuscular blockade, spontaneous breathing, and the LMA insertion skills of anesthesiologists. Furthermore, until now, there are no prospective, randomized, controlled studies regarding these factors. Therefore, this study was designed to compare the ease, grade of leak around the cuff, grade of fiberoptic view, and complications when inserting the LMA with the cuff fully deflated and partially inflated.
After obtaining approval of the Institutional Review Board (Seoul, Korea) and written informed consents from the patients, American Society of Anesthesiologists physical status I or II 172 female patients (20-50 years old) scheduled for short gynecologic procedures, which lasted for 30 min under general anesthesia, were included in this study. Patients with respiratory tract infections, esophageal problems, or cardiovascular diseases, and at risk for aspiration were excluded.
Patients were premedicated with intramuscular midazolam (0.05 mg/kg) 60 minutes before the induction of general anesthesia. Upon arrival at the operation room, standard monitoring devices including 3-lead electrocardiogram, non-invasive blood pressure measurement, and pulse oximetry were applied. All patients received IV glycopyrrolate (0.2 mg). Anesthesia was induced with 2 mg/kg of propofol and 1 µg/kg of remifentanil. A size #4 LMA was inserted 2 minutes after intravenous atracurium injection (0.5 mg/kg). All LMA insertions were done by an anesthesiologist who had experienced more than 3000 LMA insertions since 1998. Patients were randomly allocated into one of the two groups using computer generated random numbers; the fully deflated (n=86) and partially inflated group (n=86). In the fully deflated group, the LMA was inserted with the cuff fully deflated using the standard method described by Brain3 In the partially inflated group, the LMA was inserted using the same method described by Brain3 with the cuff partially inflated with 15 mL of air (half the amount of air recommended by the manufacturer). Once the LMA was inserted, the cuff was inflated until it reached a pressure of 60 cmH2O using a manometer (Cuff pressure gauge, VBM Medizintechnik, Sulz, Germany). The position of the LMA was confirmed clinically by auscultating both lung fields to ensure symmetrical air entry, the absence of gastric insufflation with auscultation of the epigastrium, and the presence of end-tidal carbon dioxide tracing. The number of attempts and the time taken for successful insertion (from the beginning of LMA introduction until the confirmation of adequate LMA position) were recorded by an observer not involved in this study. An attempt was defined as one passage of the LMA into the oropharynx. Maximal attempts were limited to two. If unsuccessful after two attempts, orotracheal intubation was done. General anesthesia was maintained with sevoflurane (1.5-3 vol%) and remifentanil infusion (0.1 µg/kg/min). Patients' lungs were ventilated with a tidal volume of 8-10 mL/kg at a rate of 8-12 breaths/min in 50% O2/50% air (2 L), adjusted to maintain the end-tidal CO2 partial pressure (PETCO2) between 30-40 mm Hg. Arterial blood pressure (systolic, diastolic, and mean), pulse oximetric saturation, and PETCO2 were monitored throughout surgery at 5-min intervals. The remaining data were evaluated by another anesthesiologist blinded to the groups. In order to maintain airway pressure at 20 cmH2O, manual bagging was done during the evaluation of leakage. The leak around the cuff at an airway pressure of 20 cmH2O was graded as 1=no leak, 2=palpable leak only, 3=palpable and audible leak with satisfactory ventilation, 4=palpable and audible leak, with inadequate ventilation, and 5=total obstruction with no possible ventilation.6 The grade of fiberoptic view was also evaluated: 1=glottis only seen, 2=epiglottis and glottis seen, 3=epiglottis impinging on grille, glottis seen, 4=epiglottis down folded, glottis not seen.6 At the end of surgery, the LMA was removed. The tip of the LMA was examined for the presence of blood. In the evening of postoperative day one, patients were asked if they had any discomfort during swallowing saliva (odynophagia), sore throat and hoarseness. Patients were followed up until discharge and medical records were reviewed for the evaluation of other esophageal or laryngeal injuries.
Sample size was predetermined using a power analysis program (Power and Sample Size Calculation ver 3.0, Vanderbilt University, Nashville, TN, USA) based on the assumptions that 1) the incidence of blood on the tip of LMA in the partially inflated group would be about 20% (based on the results of a preliminary study with a sample size of 10). 2) The incidence of blood on the tip of LMA will be decreased by 15% with the fully deflated standard technique, and 3) α=0.05 with a power (1-β) of 0.8.
Statistical analyses were performed with SAS software (version 6.12, SAS Institute, Cary, NC, USA). Demographic data, vital signs, number of LMA insertion attempts, time to successful LMA insertion, and number of complications were compared between the two groups using the Student's t-test. The data of vital sign trends during surgery in each group were compared using the repeated measures analysis of variance. Posthoc analysis was done using the Bonferroni test. The grade of leak around the cuff and fiberoptic view were compared between the two groups using chi-square test. p<0.05 was considered statistically significant.
All 172 patients completed the study protocol. There were no cases of insertion failure in both groups.
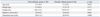
Patients' characteristics were similar in both groups (Table 1). There were no significant differences in hemodynamic variables between the groups during surgery.
The number of attempts and time to successful insertion were not significantly different. In the fully deflated group, grade 1 leak around the cuff was observed in 95.3%, and grade 2 leak was observed in 4.7% of patients. In the partially inflated group, grade 1 leak was observed in 89.5%, grade 2 leak in 8.1%, and grade 3 leak in 2.3% of patients. The grade of fiberoptic view in the fully deflated group was grade 1 in 94.2%, and grade 2 in 5.8% of patients. In the partially inflated group, 80.2%, 18.6% and 1.2% of patients presented with fiberoptic view grade 1, 2, and 3, respectively. Although there was no significant difference in the grade of leak, the grade of fiberoptic view was significantly different between the two groups (p<0.05).
The incidence rate of blood observed on the LMA at removal was significantly lower in the fully deflated group than in the partially inflated group (1.7% vs. 16.3%, p<0.05). The incidence rate of odynophagia was significantly lower in the fully deflated group than in the partially inflated group as well (5.8% vs. 18.6%, p<0.05). The incidence rate of sore throat was not significantly different between the two groups, and hoarseness was not observed in any patients in both groups (Table 2).
All patients were discharged from the hospital without any other specific complications such as esophageal or laryngeal injuries.
The LMA was invented by Dr. Archie Brain in 1981. Since its invention, the LMA has been proven to be useful in many settings, such as supporting difficult intubations, ambulatory surgery, resuscitation of neonates and adults, teaching blind nasal intubation, etc.11-19
Brain suggested that the LMA should be inserted with the cuff fully deflated. With the patient's neck flexed and the head extended, the LMA is pushed up softly against the palate in the manner of holding a pen. After the LMA is in place, the cuff is inflated and the position of the LMA is confirmed clinically by observing for signs of airway obstruction.20
Many attempts have been made to improve the success rate of LMA insertion by modifying the standard Brain technique, whereas different LMA insertion techniques have been shown to have diverse degrees of success.6-10,20 Matta, et al.9 demonstrated that inserting the LMA with the cuff partially inflated is likely to be more successful than with the fully deflated cuff. On the other hand, Brimacombe and Berry10 reported that insertion of the LMA with the cuff partially inflated is less successful than with the cuff fully deflated. However, these earlier studies were done without controls on spontaneous breathing and the LMA insertion skills of the anesthesiologist, and neuromuscular blockades were not used.
In this study, we controlled the aforementioned factors to obtain more accurate and objective results. Because an experience is a very important factor on the successful insertion of LMA, LMA insertion was done by a skilled expert who had experienced more than 3000 LMA insertions since 1998. As a result, we found that the number of attempts and the time taken for successful insertion were not significantly different between the fully deflated and partially inflated groups. Moreover, the grade of leak around the cuff did not show any significant difference in the both groups. These results indicate that, the two different insertion techniques show similar success rates if the degree of success is confirmed by clinical methods such as observing any signs of airway obstruction.
In the present study, we also studied the grade of fiberoptic view and complication rates in the both groups. The grade of fiberoptic view was significantly different between the two groups, with the fully deflated group showing superior results. Also, there were statistically more complications such as bleeding and odynophagia in the partially inflated group. Although the degree of success were not different between the two groups, the accuracy of LMA insertion therefore seemed to be higher with lower complication rates in the fully deflated insertion method. In conclusion, although the fully deflated and partially inflated LMA insertion techniques do not differ in the ease of insertion and clinical degrees of success in adult patients, the fully deflated method is more accurate with a lower complication rate than the partially inflated method.
Figures and Tables
Table 2
Comparisons between the Two Groups

LMA, laryngeal mask airway.
Data are presented as number (percentage). Grade of leak: no leak (1), only palpable leak (2), palpable and audible leak with satisfactory ventilation (3), palpable and audible leak, with inadequate ventilation (4), total obstruction with no possible ventilation (5). Grade of fiberoptic view: Glottis only seen (1), Epiglottis and Glottis seen (2), Epiglottis impinging on grille, glottis seen (3), Epiglottis down folded, glottis not seen (4).
*p<0.05.
References
1. Howes BW, Wharton NM, Gibbison B, Cook TM. LMA Supreme insertion by novices in manikins and patients. Anaesthesia. 2010. 65:343–347.
2. Castle N, Owen R, Hann M, Naidoo R, Reeves D. Assessment of the speed and ease of insertion of three supraglottic airway devices by paramedics: a manikin study. Emerg Med J. 2010. 27:860–863.

3. Brain AI. The intavent laryngeal mask instruction manual. 1991. 2nd ed. Henley-on-Thames: Intavent international SA.
4. Lopez-Gil M, Brimacombe J, Alvarez M. Safety and efficacy of the laryngeal mask airway. A prospective survey of 1400 children. Anaesthesia. 1996. 51:969–972.

5. Joshi GP. Inhalational techniques in ambulatory anesthesia. Anesthesiol Clin North America. 2003. 21:263–272.

6. Kundra P, Deepak R, Ravishankar M. Laryngeal mask insertion in children: a rational approach. Paediatr Anaesth. 2003. 13:685–690.

7. Ghai B, Makkar JK, Bhardwaj N, Wig J. Laryngeal mask airway insertion in children: comparison between rotational, lateral and standard technique. Paediatr Anaesth. 2008. 18:308–312.

8. Nakayama S, Osaka Y, Yamashita M. The rotational technique with a partially inflated laryngeal mask airway improves the ease of insertion in children. Paediatr Anaesth. 2002. 12:416–419.

9. Matta BF, Marsh DS, Nevin M. Laryngeal mask airway: a more successful method of insertion. J Clin Anesth. 1995. 7:132–135.

10. Brimacombe J, Berry A. Insertion of the laryngeal mask airway--a prospective study of four techniques. Anaesth Intensive Care. 1993. 21:89–92.

11. McClune S, Regan M, Moore J. Laryngeal mask airway for caesarean section. Anaesthesia. 1990. 45:227–228.

12. Brain AI. Three cases of difficult intubation overcome by the laryngeal mask airway. Anaesthesia. 1985. 40:353–355.

13. Cork R, Monk JE. Management of a suspected and unsuspected difficult laryngoscopy with the laryngeal mask airway. J Clin Anesth. 1992. 4:230–234.

14. Lavies NG. Use of the laryngeal mask airway in neonatal resuscitation. Anaesthesia. 1993. 48:352.

15. Berry A, Brimacombe J. Laryngeal mask airway and recovery room pollution. Anaesthesia. 1993. 48:541–542.

16. Thomson KD. A blind nasal intubation using a laryngeal mask airway. Anaesthesia. 1993. 48:785–787.

18. O'Neill B, Templeton JJ, Caramico L, Schreiner MS. The laryngeal mask airway in pediatric patients: factors affecting ease of use during insertion and emergence. Anesth Analg. 1994. 78:659–662.
19. Kamada M, Kouno S, Satake Y, Kawashima S, Adachi Y. [Use of intubating laryngeal mask airway in combination with fiberoptic intubation in a patient with morbid obesity and unexpected lingual tonsillar hypertrophy]. Masui. 2010. 59:460–463.
20. Haghighi M, Mohammadzadeh A, Naderi B, Seddighinejad A, Movahedi H. Comparing two methods of LMA insertion; classic versus simplified (airway). Middle East J Anesthesiol. 2010. 20:509–514.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download