Abstract
Purpose
In earlier analyses, desflurane has been shown to reduce average extubation time and the variability of extubation time by 20% to 25% relative to sevoflurane in adult patients. We undertook this study to determine which agents prompt less recovery time in pediatric patients undergoing minor surgery.
Materials and Methods
After obtaining Institutional Review Board approval, we retrospectively reviewed the anesthesia records of 499 patients, with an average age of 5 years, who underwent minor surgeries at Severance Eye and Ear, Nose and Throat Hospital between May 2010 and April 2011. Anesthesia was induced with propofol and rocuronium. Anesthesia was maintained with sevoflurane (n=340) or desflurane (n=159) with 50% air/O2. Time from cessation of anesthetics to recovery of self-respiration, eye opening on verbal command and extubation were compared between the two groups. Additionally, the incidences of postoperative respiratory adverse events were also compared.
Results
Times to self-respiration recovery, eye opening on verbal command, and extubation were significantly faster in the desflurane group than the sevoflurane group (4.6±2.5 min vs. 6.9±3.8 min, 6.6±3.0 min vs. 9.2±3.6 min, and 6.2±2.7 min vs. 9.3±3.7 min, respectively, p<0.005). There were no statistically significant differences between the two groups with respect to adverse respiratory events during the peri-operative period (38.2% vs. 34.6%, p=0.468).
The ideal recovery profile of a general anesthetic or technique comprises fast recovery without any postoperative adverse event. Previous studies demonstrated more rapid awakening after desflurane anesthesia compared with sevoflurane, as determined by times to eye opening, regaining of orientation, and ability to follow commands.1 In prior reports, desflurane reduced the average time to extubation and variability of extubation time by 20% to 25% relative to sevoflurane in adult patients.2 In addition, Mckay, et al.3 reported that desflurane allows for an earlier return of protective airway reflexes.
On the other hand, the effect of desflurane on the respiratory mechanics in the presence of bronchial hyper-responsiveness remains a subject of debate; desflurane has been reported to exert a relaxation effect against bronchoconstriction,4 to have no effect on increased airway tone,5 to irritate the airway under clinical conditions,6 and to worsen the resistance of the respiratory system.4
Although desflurane may irritate the airways as manifested by elevated respiratory resistance,7,8 it has become increasingly used because of its low solubility and fast recovery. Therefore, this study was designed to identify which agent between desflurane and sevoflurane prompts faster recovery times in pediatric patients with normal airway responsiveness undergoing minor surgery, without increasing the incidence of postoperative respiratory adverse events.
After obtaining Yonsei University Health System (YUHS) Institutional Review Board approval (4-2011-0654), we retrospectively reviewed the YUHS electronic medical records of 838 patients with an average age of 5-years-old (range 1 to 14 years) [American society of Anesthesiologists physical status classification system (ASA) I-II], who underwent minor surgery in the Department of Eye and Ear, Nose and Throat at Severance Hospital, Seoul, Korea, from May 2010 to April 2011. Children with a history of recent upper respiratory tract infection were excluded from the study (n=338). Also, one child who underwent a re-operation due to bleeding was excluded (Fig. 1).
All anesthetic procedures were standardized. Anesthesia was induced with propofol (3-5 mg/kg) and rocuronium (0.3-0.5 mg/kg). Children were intubated and mechanical ventilated. Anesthesia was maintained with sevoflurane (n=340) or desflurane (n=159) with 50% air/O2. The concentration and age-adjusted minimal alveolar concentration of exhaled anesthetic was monitored using an infrared analyzer (Dräger Primus®; Draeger Medical AG & Co KGaA, Luebeck, Germany). Bispectral index score (BIS VISTA™, Aspect Medical System Inc., Newton, MA, USA) was monitored during the surgery. Inhalation agents were titrated to maintain a BIS value between 40 and 60, and the hemodynamic variables within 20% of baseline values. Fentanyl (1 µg/kg) was administered intravenously after induction for prevention of postoperative pain. No additional muscle relaxant or opioid was administered during the surgery. At the moment when the surgeon notified the anesthesiologist of the last suture, inhalational anesthetics were discontinued. At the end of surgery, the administration of fresh gas was increased to 10 L/min until the return of airway reflexes, and residual muscle relaxation was completely reversed with neostigmine (0.02 mg/kg) and atropine (0.01 mg/kg) after confirming the recovery of neuromuscular function using a nerve stimulator (TOF-Watch SX, Organon Ireland Limited, Dublin, Ireland). A resident anesthetist, trained for more than 2 years, was entrusted with performing extubation. The anesthetist also recorded the time from discontinuation of anesthetic administration until the patient's first distinguishable response to the command, "Open your eyes". If the child did not respond to the calling of his or her name, the anesthetist continued calling the child's name with mild probing every 30s, until the child woke up. Each patient's trachea was extubated when the child demonstrated a cough or a gag reflex, grimace and purposeful movement, as well as regained spontaneous respiration. After extubation, each child was transported to the post-anesthetic care unit (PACU) and observed until fully awake. Forty percent of "blow by" oxygen was given by facemask until full recovery. Continuous oxygen saturation, electrocardiography and non-invasive blood pressure were monitored at 5 min intervals during transportation from the operating room to the PACU. After awakening, children who fulfilled the criteria of the Anesthesia Discharge Scoring system of Aldrete9 were transferred to the general ward. The face, legs, activity, cry, consolability scale was utilized to assess pain in children under the age of 7 years or individuals that were unable to communicate their pain.10 A score of less than two indicated sufficient recovery for which to discharge the children from the PACU. Severe postoperative pain was treated with intravenous fentanyl (0.5 µg/kg) in the PACU.
The times from discontinuation of anesthetics to recovery of self-respiration, extubation and eye opening upon verbal command as well as the duration of PACU stay were compared. The occurrence of respiratory adverse events such as sustained coughing, laryngospasm, bronchospasm, respiration hold and oxygen saturation less than 95% were collected at each of the following time points: insertion of laryngoscope (T1), intubation (T2), extubation (T3), immediate post-extubation (T4), and PACU stay (T5). The times to self-respiration, extubation and eye opening were compared between the two groups as the primary end points. The incidences of respiratory adverse events were also compared between the two groups as a secondary endpoint.
All data were reported as means±SD and percentages. Parametric data were analyzed using an unpaired Student's t-test. Ordinal data were analyzed using the Mann-Whitney ranked sum test. Nominal data were analyzed using either the chi-square or Fisher's exact test. p-values <0.05 were considered statistically significant.
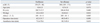
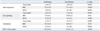
There were no clinically significant differences between the two groups with respect to demographic data, duration of surgery and anesthesia (Table 1). In the Desflurane group, time to self-respiration, eye opening and extubation were significantly faster compared to the Sevoflurane group (Table 2). At the moment of self-respiration and extubation, the values of BIS of the Desflurane group and Sevoflurane group were not different (Table 2), and the difference in BIS at eye opening had no clinical relevance. The duration of PACU stay was 3 minutes shorter in the Desflurane group than in the Sevoflurane group (p<0.05) (Table 2).
The times to restoration of self-respiration, eye opening and extubation according to the two different anesthetics were compared using the log rank test (p<0.001). The times to recovery of self-respiration, eye opening on verbal command and extubation for each group were plotted as Kaplan-Meier survival curves (Fig. 2). The overall estimated mean time required to recover self-respiration was 4.3 minutes in the Desflurane group, compared to 6.8 minutes in the Sevoflurane group (p<0.001) (Fig. 2A). In other words, at 5 minutes after the discontinuation of anesthetics, 63% of Desflurane group patients recovered self-respiration, whereas only 33% of Sevoflurane group patients did. The graphs of the times to eye opening and extubation demonstrated similar patterns (Fig. 2B and C).
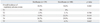
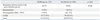
There were no significant differences between groups with respect to respiratory adverse events in the peri-operative period (Table 3). One case of bronchospasm and three cases of oxygen desaturation developed in the Sevoflurane group; however, no respiratory adverse event occurred in the Desflurane group. In the Sevoflurane group these events did not lead to detrimental or permanent complications. In the immediate post-extubation period, the overall incidences of respiratory adverse events were not different between the two groups. Coughing incidence was also not different between the Desflurane and Sevoflurane groups (26.7% vs. 29.9%, p=0.568) (Table 4).
We observed that maintenance of anesthesia with desflurane resulted in faster recovery compared with sevoflurane without increasing respiratory adverse events. The Desflurane group demonstrated a 3-minute shorter time to extubation, as well as a 3-minute shorter time to PACU discharge compared to the Sevoflurane group.
Desflurane exhibits the lowest blood-gas and tissue-blood solubility coefficients of any potent inhaled anesthetic available for clinical use.11 In adult patients undergoing outpatient anesthesia, White, et al.12 reported that recovery end points, such as time to eye opening on verbal command and regaining orientation, were significantly faster for desflurane compared with sevoflurane (p<0.05). In pediatric patients undergoing ambulatory anesthesia, the emergence (extubation) and recovery from anesthesia (Steward score 6) were significantly faster in the desflurane group compared with the sevoflurane group (5±2 min vs. 11±4 min and 11±4 min vs. 17±6 min respectively).13 These results are in agreement with our data. The differences between the two anesthetics might not be as important in the general population of surgical patients; however, a faster recovery of protective airway reflexes in patients undergoing oropharyngeal surgery, who are at risk of pulmonary aspiration caused by postoperative bleeding, may be helpful.3 In this regard, Mckay, et al.3 tested whether delayed awakening was associated with a delayed restoration of protective airway reflexes. As expected, they showed that desflurane, a less soluble anesthetic, allowed for an earlier return of protective airway reflexes. Also, airway reflex recovery was shown to be significantly less predictable after sevoflurane anesthesia compared to desflurane.14
Nevertheless, previous reports demonstrated that desflurane had deleterious effects with markedly exaggerated airway narrowing in children with susceptible airways.15 As respiratory adverse events are major causes of morbidity and mortality during pediatric anesthesia, some clinicians are reluctant to use desflurane in children with susceptible airways. However, as seen in our results, there were no significant differences between desflurane and sevoflurane with respect to respiratory adverse events in the perioperative period (Table 3). There were also no differences in the incidence of peri-operative coughing (20.9% vs. 13.7%, p=0.118), although we did not consider the severity or duration of coughing. Therefore, our data insists that there are no differences with respect to perioperative respiratory adverse effects between desflurane and sevoflurane, when used at concentrations commonly used in clinical practice and combined with small doses of opioid. White, et al.12 reported the overall incidence of coughing during the perioperative period was significantly higher for desflurane in comparison to sevoflurane (21% vs. 10%, p<0.05). However, previous data that showed desflurane affects respiratory mechanics in the presence of bronchial hyper-responsiveness are under debate. Lele, et al.4 reported that the bronchodilating capacity of desflurane and sevoflurane could relieve basal airway smooth muscle tension, and desflurane demonstrated equivalent relaxation activity on airway muscle to other inhalation anesthetics in vitro. Airway tone is regulated by the sympathetic nervous system, which is influenced by inhalation agents. Desflurane stimulates the sympathetic nervous system, causes the activation of bronchial smooth muscle to worsen the resistance of the airway. As a small dose of opioid could block sympathetic stimulation, desflurane might have a protective effect against acetylcholine-induced broncho-constriction.16,17
Notwithstanding, desflurane was previously shown to be associated with a higher incidence of emergence agitation in a prior study of pediatric adenoidectomy, although desflurane enabled more rapid wake-up than sevoflurane or halothane. Welborn, et al.13 reported that desflurane involves a significantly greater incidence (55%) of postoperative agitation and excitement in pediatric patients, compared with sevoflurane (10%), both of which are known to prolong PACU stay.18 In our retrospective study, we could not assess the incidence of postoperative emergence delirium according to inhalation agents. Previous study explained that a rapid transition from anesthesia to consciousness in a strange area with unfamiliar people and postoperative pain result in fear and apprehension in children.18 Welborn, et al. anesthetized with halothane induction, 67% N2O, no opioid and Mapleson D circuit, whereas we used propofol (3-5 mg/kg) and fentanyl (1 µg/kg) intravenously and a low flow semi-closed circuit system. In addition, our children were induced while accompanied by their parents holding their hands and met their parents at the moment of PACU arrival. We consider that these multi-modalities, such as large doses of propofol,19,20 the usage of opioid,21 slow transition to consciousness and developing close relationships between children and caregivers, could reduce the incidence of emergence agitation.22 In our study, the duration of PACU stay was shorter in the Desflurane group than the Sevoflurane group. Shorter stay in the PACU might have resulted from the attenuating effect of emergence delirium in children. Our results suggested that the incidence of emergence agitation may not be directly correlated with the type of inhalation agent used.
In addition, the potential decrease in OR and PACU labor costs from rapid emergence has economic implications. If patients emerge from anesthesia more quickly, then the time from when surgery is finished to the time the patient leaves the OR may be decreased. This reduction of emergence time can in turn reduce direct labor costs of OR time, especially when either the OR has over-utilized time or there is more than 8 hr of staffing planned for the OR.23,24 Dexter, et al.2 insisted that reductions in the average of and variance in time to extubation can be interpreted and monitored in terms of corresponding expected 75% reductions in the incidences of prolonged extubation times by using desflurane relative to sevoflurane.
This study was limited by its retrospective design. We were unable to assess the severity and duration of peri-operative respiratory adverse events. However, none of the children in our study experienced long-term or permanent adverse sequelae. Although one case of bronchospasm and three cases of oxygen desaturation developed in the Sevoflurane group, these events did not lead to detrimental or permanent complications.
In conclusion, emergence and recovery from anesthesia were significantly faster in the desflurane group based on times to eye opening, regaining spontaneous respiration, extubation and duration of PACU stay in children who underwent minor surgery. In addition, desflurane did not increase the incidences of any respiratory adverse events in the perioperative period compared to sevoflurane.
Figures and Tables
Fig. 2
Kaplan-Meier survival curves of proportional patients who did not respond over time: according to self-respiration (A), eye opening (B) and extubation (C).

ACKNOWLEDGEMENTS
This study was supported by the Yonsei University Research Grant (No. 6-2008-0279, B-N.K.).
References
1. Chen X, Zhao M, White PF, Li S, Tang J, Wender RH, et al. The recovery of cognitive function after general anesthesia in elderly patients: a comparison of desflurane and sevoflurane. Anesth Analg. 2001. 93:1489–1494.

2. Dexter F, Bayman EO, Epstein RH. Statistical modeling of average and variability of time to extubation for meta-analysis comparing desflurane to sevoflurane. Anesth Analg. 2010. 110:570–580.

3. McKay RE, Large MJ, Balea MC, McKay WR. Airway reflexes return more rapidly after desflurane anesthesia than after sevoflurane anesthesia. Anesth Analg. 2005. 100:697–700.

4. Lele E, Petak F, Fontao F, Morel DR, Habre W. Protective effects of volatile agents against acetylcholine-induced bronchoconstriction in isolated perfused rat lungs. Acta Anaesthesiol Scand. 2006. 50:1145–1151.

5. McKay RE, Bostrom A, Balea MC, McKay WR. Airway responses during desflurane versus sevoflurane administration via a laryngeal mask airway in smokers. Anesth Analg. 2006. 103:1147–1154.

6. Klock PA Jr, Czeslick EG, Klafta JM, Ovassapian A, Moss J. The effect of sevoflurane and desflurane on upper airway reactivity. Anesthesiology. 2001. 94:963–967.

7. Goff MJ, Arain SR, Ficke DJ, Uhrich TD, Ebert TJ. Absence of bronchodilation during desflurane anesthesia: a comparison to sevoflurane and thiopental. Anesthesiology. 2000. 93:404–408.
8. Dikmen Y, Eminoglu E, Salihoglu Z, Demiroluk S. Pulmonary mechanics during isoflurane, sevoflurane and desflurane anaesthesia. Anaesthesia. 2003. 58:745–748.

9. Chung F. Discharge criteria--a new trend. Can J Anaesth. 1995. 42:1056–1058.
10. Merkel SI, Voepel-Lewis T, Shayevitz JR, Malviya S. The FLACC: a behavioral scale for scoring postoperative pain in young children. Pediatr Nurs. 1997. 23:293–297.
12. White PF, Tang J, Wender RH, Yumul R, Stokes OJ, Sloninsky A, et al. Desflurane versus sevoflurane for maintenance of outpatient anesthesia: the effect on early versus late recovery and perioperative coughing. Anesth Analg. 2009. 109:387–393.

13. Welborn LG, Hannallah RS, Norden JM, Ruttimann UE, Callan CM. Comparison of emergence and recovery characteristics of sevoflurane, desflurane, and halothane in pediatric ambulatory patients. Anesth Analg. 1996. 83:917–920.

14. McKay RE, Malhotra A, Cakmakkaya OS, Hall KT, McKay WR, Apfel CC. Effect of increased body mass index and anaesthetic duration on recovery of protective airway reflexes after sevoflurane vs desflurane. Br J Anaesth. 2010. 104:175–182.

15. von Ungern-Sternberg BS, Saudan S, Petak F, Hantos Z, Habre W. Desflurane but not sevoflurane impairs airway and respiratory tissue mechanics in children with susceptible airways. Anesthesiology. 2008. 108:216–224.

16. Lee J, Oh Y, Kim C, Kim S, Park H, Kim H. Fentanyl reduces desflurane-induced airway irritability following thiopental administration in children. Acta Anaesthesiol Scand. 2006. 50:1161–1164.

17. Kong CF, Chew ST, Ip-Yam PC. Intravenous opioids reduce airway irritation during induction of anaesthesia with desflurane in adults. Br J Anaesth. 2000. 85:364–367.

18. Aouad MT, Nasr VG. Emergence agitation in children: an update. Curr Opin Anaesthesiol. 2005. 18:614–619.

19. Pieters BJ, Penn E, Nicklaus P, Bruegger D, Mehta B, Weatherly R. Emergence delirium and postoperative pain in children undergoing adenotonsillectomy: a comparison of propofol vs sevoflurane anesthesia. Paediatr Anaesth. 2010. 20:944–950.

20. Aouad MT, Yazbeck-Karam VG, Nasr VG, El-Khatib MF, Kanazi GE, Bleik JH. A single dose of propofol at the end of surgery for the prevention of emergence agitation in children undergoing strabismus surgery during sevoflurane anesthesia. Anesthesiology. 2007. 107:733–738.

21. Dong YX, Meng LX, Wang Y, Zhang JJ, Zhao GY, Ma CH. The effect of remifentanil on the incidence of agitation on emergence from sevoflurane anaesthesia in children undergoing adenotonsillectomy. Anaesth Intensive Care. 2010. 38:718–722.

22. Przybylo HJ, Martini DR, Mazurek AJ, Bracey E, Johnsen L, Coté CJ. Assessing behaviour in children emerging from anaesthesia: can we apply psychiatric diagnostic techniques? Paediatr Anaesth. 2003. 13:609–616.

23. Dexter F, Macario A, Manberg PJ, Lubarsky DA. Computer simulation to determine how rapid anesthetic recovery protocols to decrease the time for emergence or increase the phase I postanesthesia care unit bypass rate affect staffing of an ambulatory surgery center. Anesth Analg. 1999. 88:1053–1063.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download