Abstract
Purpose
The cervical dynamic rotational plating system may induce bone graft subsidence, so it may cause loss of cervical lordosis. However there were few studies for alignments of cervical spines influencing the clinical results after using dynamic rotational plates. The purpose is to evaluate the effect of graft subsidence on cervical alignments due to the dynamic rotational cervical plates and correlating it with the clinical outcomes of patients undergoing anterior cervical fusion.
Materials and Methods
Thirty-three patients with disease or fracture underwent anterior cervical decompression and fusion using a dynamic rotational plate. The presence and extent of implant complications, graft subsidence, loss of lordosis were identified and Visual Analog Scale score (VAS score), Japanese Orthopaedic Association score (JOA score), clinical outcomes based on Odom's criteria were recorded.
Results
Fusion was achieved without implant complications in all cases. The mean graft subsidence at 6 months after the surgery was 1.46 mm. The lordotic changes in local cervical angles were 5.85° which was obtained postoperatively. VAS score for radicular pain was improved by 5.19 and the JOA score was improved by 3. Clinical outcomes based on Odom's criteria showed sixteen excellent, ten good and two satisfactory results. There was no significant relationship between clinical outcomes and changes in the cervical angles.
Since Böhler and Gaudernak1 commercialized static cervical plates for the first time, many different plates are being applied commercially and used according to their biomechanical characteristics; especially for their merits in load sharing. Dynamic anterior cervical plating after anterior decompression and bone grafting is an especially widespread method in the clinical field. It was reported that biomechanically, dynamic rotational cervical plates prevent stress shielding and enable full load sharing better than static plates by maintaining axial load to the bone graft, therefore inducing early bone union.2-4 The alignment of cervical spines change to become lordotic and this improves the function of the spine for patients with cervical myelopathy or cervical kyphosis.5 The abnormal changes in the alignment of the cervical vertebrae by arthrodesis caused degeneration to develop during the follow-up periods of a few studies.6-8 The cervical dynamic rotational plating system may induce graft subsidence, so cervical lordosis and the recovered disc space height can be lost by bone graft subsidence. In addition, the abnormal changes in the sagittal alignment of the cervical spine may affect clinical outcomes. However, there are only two studies that investigated the influence of dynamic rotational plates on the alignment of cervical spines in cervical arthrodesis.9,10
The purpose of this study is to evaluate the alignment of the cervical spines and clinical outcomes of dynamic rotational plates in patients who underwent anterior cervical decompression and fusion.
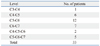
Thirty-three patients were recruited between March 1, 2005 through February 28, 2009 who had undergone cervical decompression and fusion with dynamic rotational anterior cervical plates under the diagnosis of cervical myelopathy, radiculopathy, or fracture. The indications for surgical treatment consisted of cervical myelopathy (n=5), cervical radiculopathy (n=23), and fracture (n=5), where 21 patients were male and 12 were female. The average age of the patients who had undergone surgery for each disease entity is as follows; 59.4 years old (range: 46-67 years old) for cervical myelopathy, 50.8 years old (range: 23-72 years old) for cervical radiculopathy, and 44 years old (range: 26-66 years old) for fracture. Additionally, the patients with cervical radiculopathy had received conservative treatment for 3 months before the surgery. The average follow-up period was 18 months (range: 12-24 months). In this study, we analyzed the collected clinical information and digitalized the images retrospectively. The Institutional Review Board of our university approved this study.
In all patients we measured the degree of pain before and after the surgery and the clinical manifestations using the Visual Analogue scale score (VAS score), Odom's Criteria and Japanese Orthopaedic Association score (JOA score). For the patients with radiculopathy, the degree of pain on the arms were measured by using the VAS score. In addition, the Odom's Criteria were assessed for the patients with cervical radiculopathy or fracture.
The same orthopedic surgeon performed every surgery. Twenty-six patients received one-level discectomy and a bone graft and the other seven patients received two-level discectomy with a bone graft (Table 1). The surgical approach was decided according to the pattern of the symptoms of the patients. Decompression was done by discectomy, and structural fibular allograft was used to maintain the lordotic alignment of the cervical spine by Smith and Robinson11 technique. The anterior endplate of the vertebral body was preserved and corticocancellous allograft was inserted. We used the Zephir plate (Medtronic Sofamor Danek, Memphis, TN, USA), which allows longitudinal rotational movements at the plate and screw junction with the screws fixed on the bone.
Radiologic evaluation included standard lateral view of radiographs in a neutral position, which was taken preoperatively and postoperatively at 2 weeks, 6 weeks, 3 months, 6 months, and 12 months after the surgery. Bone union, graft subsidence, alignment of the cervical spine at the level of operation (local angle), and the alignment of the whole cervical spine (cervical angle) were measured. Also, loosening and breakage of the plate and screws were evaluated. The local angle was measured using two lines-one drawn horizontally to the cranial endplate of the most cranial vertebrae surgically and the other horizontally to the caudal endplate of the most caudal vertebrae surgically (Fig. 1).5 The cervical angle was measured in a similar way with a line horizontal to the cranial endplate of the 3rd cervical vertebrae and the other line horizontal to the caudal endplate of the 7th cervical vertebrae (Fig. 1). A negative angle refers to a lordotic curve, whereas a positive angle refers to cervical kyphosis. Bone union was defined when there was a bony bridge across the graft site and no visible movements seen on the flexion and extension views.
Paired t-tests were used to compare the VAS scores of the preoperative and postoperative status. Unfortunately, he JOA score was not analyzed because of the limited number of patients. Interval changes, bone graft subsidence, local angles, and cervical angles were compared. We analyzed the time course of interval changes using the paired t-test. We also analyzed the correlation between graft subsidence and changes in the sagittal angle using a linear regression method. Each statistical analysis had 95% of confidence interval and was statistically significant if the p-value was <0.05.
The patient groups with radiculopathy and fracture showed an average decrease of 5.19 points in VAS score for the arm pain, whereas the patient group who had cervical myelopathy showed an average increase of 3 points using the JOA score postoperatively. Clinical outcome reviews of twenty-eight patients with cervical radiculopathy or fracture confirmed that sixteen had excellent results, ten had good results and two had satisfactory results based on the Odom's criteria.
There was a bony bridge that crossed the graft site for all 33 patients who underwent surgery. The bony union was achieved at 9.3 months after operation (range: 6-12 months).
No patient had reoperation and there was no remarks with regards to graft loosening, breakage or loosening of the screws and plates.
The average depth of bone graft subsidence was 0.6 mm, 1.14 mm, 1.34 mm, 1.46 mm, and 1.51 mm after 2 weeks, 6 weeks, 3 months, 6 months, and 12 months of the surgery, respectively (Fig. 2).
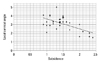
Radiologic evaluations revealed the mean local cervical angles to be -1.0 degrees before surgery and -5.85 degrees right after the surgery. Postoperative local cervical angles were -4.8, -3.5, -3.26, -3.13, and -2.98 degrees for 2 weeks, 6 weeks, 3 months, 6 months, and 12 months postoperatively, respectively (Fig. 2). Significant loss of lordosis was observed during the next 6 months after surgery; there was an average loss of lordosis of 2.59 degrees, but the remaining lordotic angle was maintained after 6 months had passed over the surgery (p<0.05). There was a statistically significant correlation between the degree of subsidence and the loss of local lordotic angle during the first 6 months after operation (p<0.05) (Fig. 3).
Radiologic evaluations revealed the mean regional cervical angles to be -3.0 degrees before surgery and -5.45 degrees right after the surgery. Postoperative regional cervical angles were -5.55, -5.7, -5.99, -6.03 and -6.08 degrees for 2 weeks, 6 weeks, 3 months, 6 months, and 12 months postoperatively, respectively (Fig. 2). Regional cervical lordosis showed no significant changes right after the surgery and during the 6 months after surgery.
The dynamic plate has an advantage in that it increases the union rate and decreases failure rate by delivering the load to the bone graft and translating the stress that comes from the screws to the plate.9,10 Since the introduction of the first dynamic plate, DOC plate,12 several kinds of dynamic plates are currently available. The types of dynamic plates are rotational plates, translational plates with slotted screw holes, and translational plates with a plate telescope. With the rotational plate, longitudinal rotation of a variable screw is available at the plate-screw interface. The abnormal changes in the alignment of the cervical vertebrae by arthrodesis caused the development of degeneration during the follow-up period of previous studies.6,7 The use of the static plate is known to maintain the lordotic state that is obtained by the bone graft. However, the dynamic plate may cause graft subsidence by load bearing, so kyphotic changes in the cervical alignment may occur. There was a report about loss of the lordotic curve after using translational plates,13,14 but there is no report about that after using rotational plates. In this study, we examined the effects of rotational plates with variable screws to the local and cervical regional alignment.
Significant loss of local lordosis was observed for 6 months postoperatively in this study, and there was an average loss of 2.59 degrees in lordosis. Two previous reports on translational plates about change to the local angle had similar results with this study. Ghahreman, et al.13 reviewed 55 patients who underwent anterior cervical decompression and fusion using a translational plate with slotted screw holes (ABC plate). Local lordotic angle was achieved as a result of surgery but there was a loss of lordosis in the first 6 months after surgery.13 In addition, Pitzen, et al.14 evaluated 33 patients who received an anterior cervical discectomy and fusion with either a translational plate with slotted screw holes (ABC plate) or a static plate. They found that the loss in local lordosis was higher when dynamic plates were used compared with the static plates.14 However, these studies are different from the current study in that they evaluated the translational plate with slotted screw holes, while the current study evaluated rotational plates with longitudinal rotation of a variable screw.
The cervical regional alignment was maintained in this study, even though the local angle of the fused segmental area decreased. A previous report on translational plates showed that there was no change in the regional cervical angles 6 months after surgery with a translational plate with slotted screw holes (ABC plate).13 It might be explained by the fact that the regional angle could have been affected by other variables such as muscle cramps and was compensated by the lordotic or kyphotic changes in other disc levels.
Several clinical studies about dynamic plates showed that the plates provides a faster fusion of the cervical spine compared to static plates and that the clinical outcomes were improved.14-17 In Goldberg's study where he compared dynamic plates and static plates, the static plate showed a 62.5% of fusion rate, while the dynamic plate showed 75% after 6 to 9 months postoperatively, and an 84.7% fusion rate for static versus 90% for dynamic plate after 10 to 13 months postoperatively.15 Unfortunately they did not specify the type of dynamic plates. Nunley, et al.16 compared the clinical outcomes in patients who underwent anterior cervical discectomy and fusion in one or more disc levels using translational plates with slotted screw holes (ABC, Aesculap) or static plates by the means of VAS score and Neck Disability Index (NDI). In a single-level fusion, different outcomes were not observed, but in multiple level fusions with translational plates there were lower VAS scores and NDI's postoperatively than those with static plates.16 Stulik, et al.17 compared the same translational plates (ABC, Aesculap) and static plates in patients who underwent one or two disc level anterior cervical discectomy and fusion. He showed that the rate of implant complication was lower with the group of patients receiving translational plates.17 Pitzen, et al.14 evaluated thirty-three patients who received an anterior cervical discectomy and fusion with either a translational plate with slotted screw holes (ABC plate) or static plate. They found the loss of local lordosis was higher when dynamic plates were used compared to the static plates.14 However, there were no differences regarding the clinical outcomes between the two groups.14
Nevertheless, it is still controversial whether the loss of local lordosis by dynamic plates deteriorates clinical outcomes. DuBois, et al.9 performed a retrospective study to compare the clinical outcomes of patients undergoing multilevel anterior cervical discectomy and fusion with either rotational plates (Atlantis, Medtronic Sofamor Danek) or static plates. Clinical results measured by the Odom's criteria were similar between the two groups.9 However, Okawa, et al.10 reported complications after rotational plates with variable screws in patients with multilevel cervical corpectomy. They reviewed 31 patients with myelopathy caused by multilevel cervical spondylosis or ossification of posterior longitudinal ligament (OPLL) who underwent multilevel corpectomy and reconstruction with autologous fibular grafts and anterior cervical plate placements.10 In the postoperative radiologic measurements, the local lordotic angle of the fused segment was larger in the patients who experienced reconstruction failures than in the patients who did not.10 The difference between their study and the current study could be explained by the fact that they reviewed the results of multilevel corpectomy and that the current study reviewed one-level or two-level discectomy and fusion.
There was no significant clinical influence related to a loss of local lordosis in this study. Although bone graft subsidence or migration occurred in a short-term follow-up, there were no changes in subjective symptoms or clinical status. However, these radiologic changes should not be ignored. The loss of cervical lordosis acts as a risk factor that contributes to progression of degenerative changes of adjacent segments.6 Also, cervical kyphosis accelerates progression of degenerative changes of the cervical spine kinetically and increases biomechanical stress on the anterior portion of vertebral bodies of adjacent segments.8 Continuous observation on progress is considered to be very important because we cannot exclude the possibility of reoperation when neurological symptoms manifest and the degenerative changes and structural changes of adjacent segments are stimulated.
There are limitations in this study. First, it was a retrospective study. Therefore, we did not have a protocol for standardizing all radiographs. Even though patients were asked to hold their neck in a neutral position, due to neck pain this may have not been possible in all cases.
In conclusion, anterior cervical fusion with dynamic rotational plates led to improvement and showed similar fusion rates compared with the former static cervical plating in anterior cervical fusion. There was partial loss in the cervical lordosis, but there was no significant clinical effect. Future studies with a longer follow-up period are needed to assure whether bone graft subsidence would have an influence on progression of degenerative changes in adjacent cervical segments.
Figures and Tables
Fig. 1
Local cervical angle (A) and regional cervical angle (B). A negative value corresponds to a lordotic angle and a positive value indicates the presence of kyphosis.

Fig. 2
Bone graft subsidence, lordotic change of local cervical angle and regional cervical angle after operation.
ACKNOWLEDGEMENTS
The authors thank Dai Jung for the work done within the study, especially preparing English manuscript.
References
1. Böhler J, Gaudernak T. Anterior plate stabilization for fracture-dislocations of the lower cervical spine. J Trauma. 1980. 20:203–205.

2. Brodke DS, Gollogly S, Alexander Mohr R, Nguyen BK, Dailey AT, Bachus AK. Dynamic cervical plates: biomechanical evaluation of load sharing and stiffness. Spine (Phila Pa 1976). 2001. 26:1324–1329.
3. Brodke DS, Klimo P Jr, Bachus KN, Braun JT, Dailey AT. Anterior cervical fixation: analysis of load-sharing and stability with use of static and dynamic plates. J Bone Joint Surg Am. 2006. 88:1566–1573.
4. Fogel GR, Li Z, Liu W, Liao Z, Wu J, Zhou W. In vitro evaluation of stiffness and load sharing in a two-level corpectomy: comparison of static and dynamic cervical plates. Spine J. 2010. 10:417–421.

5. Ferch RD, Shad A, Cadoux-Hudson TA, Teddy PJ. Anterior correction of cervical kyphotic deformity: effects on myelopathy, neck pain, and sagittal alignment. J Neurosurg. 2004. 100:1 Suppl Spine. 13–19.

6. Katsuura A, Hukuda S, Saruhashi Y, Mori K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J. 2001. 10:320–324.

7. Matsunaga S, Onishi T, Sakou T. Significance of occipitoaxial angle in subaxial lesion after occipitocervical fusion. Spine (Phila Pa 1976). 2001. 26:161–165.

8. Barsa P, Suchomel P. Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J. 2007. 16:1395–1400.

9. DuBois CM, Bolt PM, Todd AG, Gupta P, Wetzel FT, Phillips FM. Static versus dynamic plating for multilevel anterior cervical discectomy and fusion. Spine J. 2007. 7:188–193.

10. Okawa A, Sakai K, Hirai T, Kato T, Tomizawa S, Enomoto M, et al. Risk factors for early reconstruction failure of multilevel cervical corpectomy with dynamic plate fixation. Spine (Phila Pa 1976). 2011. 36:E582–E587.

11. Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg Am. 1958. 40-A:607–624.

12. Bose B. Anterior cervical arthrodesis using DOC dynamic stabilization implant for improvement in sagittal angulation and controlled settling. J Neurosurg. 2003. 98:1 Suppl. 8–13.

13. Ghahreman A, Rao PJ, Ferch RD. Dynamic plates in anterior cervical fusion surgery: graft settling and cervical alignment. Spine (Phila Pa 1976). 2009. 34:1567–1571.
14. Pitzen TR, Chrobok J, Stulik J, Ruffing S, Drumm J, Sova L, et al. Implant complications, fusion, loss of lordosis, and outcome after anterior cervical plating with dynamic or rigid plates: two-year results of a multi-centric, randomized, controlled study. Spine (Phila Pa 1976). 2009. 34:641–646.
15. Goldberg G, Albert TJ, Vaccaro AR, Hilibrand AS, Anderson DG, Wharton N. Short-term comparison of cervical fusion with static and dynamic plating using computerized motion analysis. Spine (Phila Pa 1976). 2007. 32:E371–E375.

16. Nunley PD, Jawahar A, Kerr EJ 3rd, Cavanaugh DA, Howard C, Brandao SM. Choice of plate may affect outcomes for single versus multilevel ACDF: results of a prospective randomized single-blind trial. Spine J. 2009. 9:121–127.

17. Stulik J, Pitzen TR, Chrobok J, Ruffing S, Drumm J, Sova L, et al. Fusion and failure following anterior cervical plating with dynamic or rigid plates: 6-months results of a multi-centric, prospective, randomized, controlled study. Eur Spine J. 2007. 16:1689–1694.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download