Abstract
Purpose
Although Denis classification is considered as one of most clinically useful schemes for the evaluation of spinal fracture, there is little documentation on the relationship between fracture pattern and the neurologic recovery. The purpose is to evaluate the correlation between the fracture patterns according to Denis classification and neurologic recovery.
Materials and Methods
The 38 patients (26 men and 12 women) in this series had an average follow-up of 47.1 months, and they were all managed surgically. Denis classification had been used prospectively to determine the fracture morphology. Frankel Scale and American Spinal Injury Association Spinal Cord Injury Assessment Form [American Spinal Injury Association (ASIA) score] were obtained before surgery, after surgery and at the final follow-up.
Results
The common injuries making neurologic deterioration were burst fracture and fracture-dislocation. The degree of neurologic deficits seen first and at the final follow-up was more severe in fracture-dislocation than burst fracture. The neurologic recovery was not different between burst fracture and fracture-dislocation, assessed by Frankel grading and ASIA scoring system. The neurologic recovery evaluated by ASIA score was not different between the lumbar and thoracic spinal fracture. The neurologic recovery assessed by Frankel grade was greater in the lumbar spinal fractures in than the thoracic spinal fractures.
Neurologic recovery varies from 50% to 90% in the thoracolumbar burst fractures, managed with either conservative or surgical methods.1 Several studies assessed some of the variables associated with neurological recovery after neurologic injury with spinal fracture, such as the age of patients, the level of lesion, initial canal compromise, initial posttraumatic kyphosis, timing of operation, amount of canal decompression and treatment method.1-5
The three-column theory, first proposed by Denis6 for classifying the spinal fractures is almost 30 years old. Although it is considered as one of the most clinically useful and important schemes for the evaluation of spinal fracture, there is little documentation in the literature on the relationship between fracture patterns assessed by Denis classification and neurologic recovery. The purpose of the present study is to determine whether there is a preponderance of a fracture patterns by Denis classification associated with neurologic recovery.
Institutional Review Board approved this study. This is a retrospective review of 38 consecutive thoracic, thoracolumbar and lumbar fractures combined with neurologic deficit, managed surgically, between October 1989 and July 1999. All operations were performed by one surgical team under the supervision of the senior author at a single institution. The 38 patients (26 men and 12 women) in this series had an average follow-up of 47.1 months. All patients were observed for more than 12 months. The average age at the time of operation was 36.7 years, ranging from 16 to 74 years. The cause of injury was a fall from the height in 23 patients (60.5%) and automobile accident in 8 patients (21.1%). Other causes accounted for injury in 7 patients (18.4%).
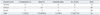
The data on 38 patients were complete enough to evaluate the fracture patterns from plain radiographs and computed tomography scan. Fracture patterns were identified according to the Denis classification (Table 1).6 The fracture-dislocations and the burst fractures were common in the thoracolumbar spines (T11-L1) (Table 1).
All patients received a comprehensive trauma assessment. Plain radiographs and computerized tomography scans were obtained in all cases; magnetic resonance images were available in 4 cases. The average delay from the time of injury until surgery was 4.6 days. The delay from the time of injury until surgery was less than 24 hours in 17 patients (44.7%) and longer than 24 hours in 21 patients (55.3%).
The 38 patients included 33 patients treated with instrumented posterior fusion using pedicle screw systems and 5 patients treated with the anterior interbody fusion using an anterior approach. The posterior laminectomy was performed in 14 patients (36.8%) for decompression and exploration of the dural sac and nerve roots of the cauda equina. Dural lacerations were observed in 3 patients and 1 patient had nerve root entrapment in the gap of laminar fracture. Postoperatively, all patients were treated with bed rest for approximately 5 days, after which they had to wear a thoracolumbosacral brace for an average of 3.3 months after their operation.
Neurologic function was assessed before and after surgery, and at the final follow-up using the Frankel grading system7 and the American Spinal Injury Association (ASIA score) rating for sensory and motor function.8 The percentage of neurologic recovery was defined as the "actual neural recovery" (final follow-up score minus preoperative score) divided by the "potential neural recovery" (maximal score minus preoperative score). The Frankel grade was exchanged numerically and analyzed. For example Frankel grade A was changed as 1 and Frankel grade E as 5.
The initial Frankel grading showed that 14 patients were Grade D, 9 patients were Grade C, 2 patients were Grade B and 13 patients were Grade A. Among 38 patients with neurologic compromise, the preoperative average ASIA sensory score was 86.7 points and the preoperative average ASIA motor score was 69.1 points. The clear neurologic improvement by Frankel grade was found in 14 patients. The average ASIA sensory scores improved from 86.7 to 89.6 points in 38 patients with neurologic injury. The average AISA motor scores similarly improved from 69.1 to 76.1 points. Neurological improvement was statistically proved by comparing the preoperative and the final follow-up values of Frankel grade, ASIA sensory and motor score (paired-samples t-test, level 5%).
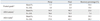
In the Denis classification, the most common injuries making neurologic compromise in this study were burst fracture and fracture-dislocation (Table 1). The severity of preoperative neurologic compromise was higher in the fracture-dislocation than burst fracture, and the severity of neurologic compromise at the final follow-up was higher in the fracture-dislocation than burst fracture, however, the neurologic recovery for Frankel grade, ASIA sensory and ASIA motor ratings was similar between burst fracture and fracture-dislocation (Table 2).
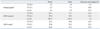
The severity of preoperative neurologic compromise was high in thoracic spinal fractures (T3-T10) and low in lumbar spinal fractures (L2-L4) (Table 3). The neurologic recovery evaluated by Frankel grade was greater in the lumbar spinal fractures than in the thoracic spinal fractures. The neurologic recovery by the fractured level, evaluated by ASIA score, was not different among the three groups.
The long-term prognosis following severe neurologic injury remains discouraging despite surgical strategies. The predominant mechanism of neurologic injury with spinal fracture is similar to that of spinal fracture.9 Therefore, it is important to correlate neurologic deficits with the classification of spinal fracture based on the mechanism of injury. Bravo, et al.2 reported that no correlation was found between the patterns of fracture and neurological recovery with spinal fracture combined with neural injury. However, their spinal fractures were classified by only compression and flexion-rotation types, but not by Denis classification. Cengiz, et al.4 reported that no correlation was found between the patterns of fracture and neurological recovery in patients with thoracolumbar fracture combined with neural injury. However, their spinal fractures were classified by Magerl classification,10 but not by Denis classification. Gertzbein11 reported the relationship between the initial neurologic injury with spinal fracture and Denis classification. However, they did not report neurologic recovery according to Denis classification. The purpose of the present study, therefore, was to determine whether there is a preponderance of a fracture pattern associated with neurologic recovery by Denis classification.
In the current study, the neurologic injuries were common at burst fractures and fracture-dislocations. Similarly, the previous studies found that neurologic deficits were common at burst fractures and fracture-dislocations classified by Denis classification.9,11 In the current study, the initial neurologic deficit was more severe in fracture-dislocations than burst fractures. Denis6 reported 52.4% of complete paraplegia in fracture-dislocations vs. 3.6% in burst fractures in the spinal fractures with neurologic injury, and stated that the fracture-dislocations are the most severe mechanical and neurologic instability. The quantity of energy delivered to neural tissue depends on the vectors by which kinetic energy is transferred to the spinal bony structure. With burst fractures, the energy from the axial load is primarily transferred to the vertebral bodies and intervertebral discs where neurologic structures only experience the kinetic energy transferred from the retropulsed vertebral body fragments.9,12 Contrarily, in the case of fracture-dislocations, the spinal canal compromise typically results from kyphotic and translational deformities. At the time of impact, the acute deformation of neural tissue resulted in the shear and stretch injury.9 Therefore, injuries to neural tissue might be more severe in the fracture-dislocation than in the burst fracture.
As for neurologic recovery, it has been suggested that re-establishing an adequate spinal canal improves the chances of neurologic recovery.13,14 On the other hand, however, there are studies to indicate no relationship between neural decompression and neurologic recovery.2,9,15-18 Interestingly, the recovery of neurologic function following severe traumatic spinal cord injury occur more frequently in children than in adults,19 suggesting that subsequent neuronal regeneration compensate for the initial neural damage and disruption. The current study showed that neurologic recovery was similar between burst fracture and fracture-dislocation, thus showing that neurologic recovery was not correlated with the fracture patterns assessed by Denis classification. Our study is supported by the previous studies that neurologic recovery was not related to the type of fracture of injury in patients with traumatic incomplete cervical spinal cord injuries5 and also in patients with thoracolumbar burst fractures and neurologic deficits.20
Several studies evaluated all spinal levels as one, making it difficult to precisely evaluate which factors actually influence neurologic recovery in patients with spinal fractures.2,21 The thoracic spine is mechanically stiffer and less mobile due to thoracic rib cage and costovertebral ligaments than thoracolumbar and lumbar regions. Therefore, greater energy is required to disrupt it.22 Consequently, it is necessary to analyze the correlation between the level of lesion and neurologic injury. In the present study, neurologic injuries were found to be more severe at the thoracic spine than at the thoracolumbar and lumbar spines. In the thoracic spine fracture, dislocations are common due to high-energy trauma. However, burst fractures are common in the lumbar spine due to relative low-energy trauma. Neurologic recovery evaluated by ASIA score was similar among the three groups by the fractured level. However, the current study showed that neurologic recovery was greater in the lumbar spinal fractures by Frankel grade, which is similar to the result of previous study.21 It might be explained by the fact that the cauda equina of lumbosacral spine have different pathophysiology and recovery potentials, and that the ASIA score evaluation system could detect difference more precisely than the Frankel grading system.
Like any other study, the present investigation has several potential problems. This is a retrospective study and mean follow-up period is 47.1 months. Therefore, the long-term follow-up is necessary to evaluate the recovery of neural injury. Furthermore, the clear neurological improvement was found in 14 out of 38 patients with posttraumatic neurological deficit. The number of patients, especially the number of patients with neurological deficit, might be too small for sound statistical analysis. Finally, we did not evaluate all four fracture patterns of Denis classification for neurologic recovery because of limited number of patients with neural deficits.
In conclusion, the severity of initial posttraumatic and final follow-up neurologic deficits was correlated with the fracture patterns assessed by Denis classification and anatomic fractured levels. However, neurologic recovery was not correlated with fracture patterns of Denis classification.
Figures and Tables
References
1. Dendrinos GK, Halikias JG, Krallis PN, Asimakopoulos A. Factors influencing neurological recovery in burst thoracolumbar fractures. Acta Orthop Belg. 1995. 61:226–234.
2. Bravo P, Labarta C, Alcaraz MA, Mendoza J, Verdú A. An assessment of factors affecting neurological recovery after spinal cord injury with vertebral fracture. Paraplegia. 1996. 34:164–166.

3. Dall BE, Stauffer ES. Neurologic injury and recovery patterns in burst fractures at the T12 or L1 motion segment. Clin Orthop Relat Res. 1988. 171–176.

4. Cengiz SL, Kalkan E, Bayir A, Ilik K, Basefer A. Timing of thoracolomber spine stabilization in trauma patients; impact on neurological outcome and clinical course. A real prospective (rct) randomized controlled study. Arch Orthop Trauma Surg. 2008. 128:959–966.

5. Pollard ME, Apple DF. Factors associated with improved neurologic outcomes in patients with incomplete tetraplegia. Spine (Phila Pa 1976). 2003. 28:33–39.

6. Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983. 8:817–831.

7. Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia. 1969. 7:179–192.

8. Standard for neurologic and functional class of spinal cord injury. 1992. Chicago: American Spinal Injury Association.
9. Lemons VR, Wagner FC Jr, Montesano PX. Management of thoracolumbar fractures with accompanying neurological injury. Neurosurgery. 1992. 30:667–671.

10. Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994. 3:184–201.

11. Gertzbein SD. Neurologic deterioration in patients with thoracic and lumbar fractures after admission to the hospital. Spine (Phila Pa 1976). 1994. 19:1723–1725.

12. Limb D, Shaw DL, Dickson RA. Neurological injury in thoracolumbar burst fractures. J Bone Joint Surg Br. 1995. 77:774–777.

13. Carl AL, Tromanhauser SG, Roger DJ. Pedicle screw instrumentation for thoracolumbar burst fractures and fracture-dislocations. Spine (Phila Pa 1976). 1992. 17:8 Suppl. S317–S324.

14. Durward QJ, Schweigel JF, Harrison P. Management of fractures of the thoracolumbar and lumbar spite. Neurosurgery. 1981. 8:555–561.

15. Bedbrook GM. Treatment of thoracolumbar dislocation and fractures with paraplegia. Clin Orthop Relat Res. 1975. 27–43.
16. Guttmann L. Spinal deformities in traumatic paraplegics and tetraplegics following surgical procedures. Paraplegia. 1969. 7:38–58.

17. Osebold WR, Weinstein SL, Sprague BL. Thoracolumbar spine fractures Results of treatment. Spine (Phila Pa 1976). 1981. 6:13–34.
18. Rimoldi RL, Zigler JE, Capen DA, Hu SS. The effect of surgical intervention on rehabilitation time in patients with thoracolumbar and lumbar spinal cord injuries. Spine (Phila Pa 1976). 1992. 17:1443–1449.

19. Wang MY, Hoh DJ, Leary SP, Griffith P, McComb JG. High rates of neurological improvement following severe traumatic pediatric spinal cord injury. Spine (Phila Pa 1976). 2004. 29:1493–1497.

20. Dai LY, Wang XY, Jiang LS. Neurologic recovery from thoracolumbar burst fractures: is it predicted by the amount of initial canal encroachment and kyphotic deformity? Surg Neurol. 2007. 67:232–237.
21. Strømsøe K, Hem ES, Aunan E. Unstable vertebral fractures in the lower third of the spine treated with closed reduction and transpedicular posterior fixation: a retrospective analysis of 82 fractures in 78 patients. Eur Spine J. 1997. 6:239–244.

22. Bohlman HH, Ducker TB. Rothman RH, Simeone FA, editors. Spine and spinal cord injuries. The spine. 1999. 4th ed. Philadelphia: W.B. Saunders company;889–1002.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download