Abstract
Purpose
Few reports have been made on the therapeutic effects as well as pathological features of an antithrombin preparation in patients diagnosed with septic disseminated intravascular coagulation (DIC) by the diagnostic criteria for acute DIC.
Materials and Methods
A total of 88 sepsis patients who had received inpatient hospital care during the period from January 2000 through December 2008 were divided into two groups, an antithrombin group and a non-antithrombin group, to study the outcomes. Furthermore, the relationship between sepsis-related factors and DIC in 44 patients was studied.
Disseminated intravascular coagulation (DIC) is classified into 3 types depending on the fibrinolytic stage: fibrinolytic inhibitor DIC in septic shock; fibrinolysis-dominant DIC in hemorrhagic shock; and fibrinolysis hyperpermeability DIC in patients with solid tumors.1 The incidence of fibrinolytic inhibitor DIC in sepsis patients is high, and the outcome is poor.2 The first treatment goal in cases of DIC is treatment of the underlying disease. Anticoagulant drugs, such as heparin, are used to blunt the pathological coagulation activation in DIC. As the effect of heparin is achieved via antithrombin, for cases in which antithrombin (AT) activity is depressed, the administration of an AT preparation is recognized as a treatment method. Recently, recombinant thrombomodulin, which has an anticoagulant effect through protein C, was developed and introduced in Japan. The Society of Critical Care Medicine developed the Surviving Sepsis Campaign guidelines in 20043 and revised them in 2008.4 These guidelines exclusively recommended activation protein C5 as a therapeutic medication for septic DIC. There have, however, been conflicting reports on the efficacy of recombinant human activated protein C (APC), or drotrecogin alfa (activated) (DrotAA), for the treatment of patients with septic shock. A recent randomized, double-blinded, placebo-controlled, multi-center trial showed that DrotAA did not significantly reduce mortality at 28 or 90 days.6 In the present study, we evaluated the efficacy of the AT preparation in septic DIC patients.
The subjects were 88 sepsis patients treated in emergency and critical care department during the period from January 2000 through December 2008. They were divided into 2 groups, an AT preparation administration group and a non-AT preparation administration group, in order to compare the outcomes. All patients were treated based on the judgment of the doctor in charge, and none of the patients had hemorrhagic tendencies. The AT-treated patients received an intravenous loading dose of 1500 to 3000 IU per day for 3 to 5 days. And abnormality in coagulation factor was recognized in most of the treated cases (platelet was 120000/mm3 or less, prothrombin time ratio was 1.2 or more, fibrin/fibrinogen degradation productsfibrin/fibrinogen degradation products was 10 ug/mL or more) and AT was 80% or less.
A sub-group analysis for the patients diagnosed with DIC was conducted according to the diagnostic criteria of the Japanese Association for Acute Medicine,7 and the outcomes of both groups were compared. In addition, as sepsis-related factors, high mobility group box protein 1 (HMGB1), plas minogen activator inhibitor (PAI-1), protein C, endogenous cannabinoid N-arachidonoylethanolamine (AEA) and 2-arachidonoyl glycerol (2-AG) were measured in 44 patients. We used the Multiplex suspension array system (Bio-Plex™, Berkeley, CA, USA) to measure the expression levels of 17 cytokines, thereby evaluating the characteristics of DIC patients. A statistical analysis was conducted by using the t-test and Kaplan-Meier survival curves, with p values less than 0.05 indicating a significant difference.
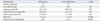
The subject group consisted of 58 men (65.9%) and 30 women (34.1%) with a mean age of 64.1±13.7 years. The mean score on the Acute Physiology and Chronic Health Evaluation (APACHE) II8 was 24.0±9.2, and the mean sepsis-related organ failure assessment (SOFA) score9 was 10.6±4.5. Although the results of a comparison of the background factors between the two groups did not reveal any differences in the APACHE II score or the SOFA score, the Japanese Association for Acute Medicine (JAAM) acute DIC score was significantly higher in the AT group than in the non-AT group (Table 1). Also, the AT group had a significantly better outcome than the non-AT group (p=0.0066) (Fig. 1).
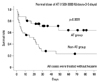
According to the results of a sub-group analysis of the group of patients that met the diagnostic criteria for DIC set by the Japanese Association for Acute Medicine, the group that received AT had a better outcome than the group that did not receive AT (p=0.0031) (Fig. 2).
With respect to the relationship between sepsis-related factors, cytokines and DIC patients, the protein C level was significantly reduced in DIC patients (p=0.0097) (Fig. 3). There were no significant differences in PAI-1, HMGB1, AEA, or 2-AG between the two groups. With respect to the 17 cytokines that were measured, the levels of IL-5 and IL-7 were significantly reduced in DIC patients (data not shown).
Depending on the fibrinolytic stage, DIC patients manifest clearly different clinical symptoms and laboratory findings. For many years, the diagnosis of DIC has been based on the criteria of the Ministry of Health, Labour and Welfare in Japan7 and the International Society on Thrombosis and Haemostasis (ISTH).10 In particular, the diagnostic criteria for DIC from the Ministry of Health, Labour and Welfare in Japan have shown high sensitivity and specificity in the detection of fibrinolysis hyperpermeability DIC in patients with solid tumors.11 Since DIC in the field of acute medicine progresses very quickly, as does the fibrinolytic inhibitor DIC in sepsis patients, it is necessary to make a diagnosis promptly without the need of special tests. In this context, the diagnostic criteria for acute DIC were reported by the JAAM in 2005.7 With regard to these diagnostic criteria for acute DIC, the relationship between the APACHE II score, the SOFA score, and the correlation with the outcome in septic shock cases have been reported.4 The JAAM DIC score serves as a useful, simple and easy tool to identify the severity of sepsis. When early diagnosis becomes possible by means of a simple, easy and prompt DIC score, then an effective post-diagnostic treatment method becomes indispensable.
APC was recommended in the Surviving Sepsis Campaign guidelines2 as a therapeutic medication for sepsis. APC inhibits excessive activation of the coagulation system, and it is believed to serve as an effective therapeutic medication for septic DIC. However, this treatment is not currently authorized in Japan, and the company that manufactured APC announced the withdrawal of its APC product from all markets following the results of a recent prospective study of recombinant APC.12
It has been confirmed that the AT-III activity level in the blood is significantly reduced in patients with septic DIC. As a result, double-blind tests have been performed in the belief that supplementation of AT-III in patients with septic DIC would improve the outcomes of sepsis.13 The main results included: positive outcomes were achieved in the AT-III administration group, although no significant differences were revealed by meta-analysis; a significantly shortened ICU stay; and an improved survival rate for patients who also experienced septic shock. In the present study, the patients received either an intravenous loading dose of 3000 IU AT-III followed by a maintenance dose of 1500 IU every 12 h for 5 days or equivalent amounts of placebo. The above treatment AT-III dose is similar to our manuscript treatment dose. A controlled double-blinded, randomized, multicenter study showed that high-dose (total dose, 24000 IU) AT-III replacement therapy in patients with sepsis and/or postsurgical complications decreased the risk of death.14 A systemic review of three randomized clinical trials showed that the combined odds ratio for short-term all-cause mortality in those who received antithrombin was 0.649.15 Another study showed that adjusted therapy with antithrombin was costly, but was associated with a reduction of total cost of care for patients with diffuse secondary peritonitis.16
In a previous paper, high-dose antithrombin without concomitant heparin in septic patients with DIC resulted in a significant mortality reduction, and it was concluded that the adapted ISTH DIC score could be used to identify patients with severe sepsis who would potentially benefit from high-dose antithrombin treatment.17 In the present retrospective study of 88 sepsis patients, significant improvements in outcomes were shown; the efficacy of antithrombin treatment was prominent particularly in DIC patients. Therefore, it is highly possible that AT-III improves the outcome of patients with septic DIC. Additionally, our study showed that the JAAM DIC score may identify patients with sepsis who could potentially benefit from normal-dose antithrombin treatment.
In conclusion, the findings of this study suggest that early administration of antithrombin might improve the outcomes of septic DIC patients who are classified according to the diagnostic criteria for acute DIC.
Figures and Tables
Fig. 1
Survival rate. Among sepsis patients, outcomes in the AT-III group were significantly better (p=0.0066). AT, antithrombin.
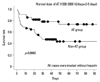
Fig. 2
Survival rate in septic DIC cases. Among septic DIC patients, outcomes in the AT-III group were significantly better (p=0.0031). AT, antithrombin; DIC, disseminated intravascular coagulation.
References
1. Kushimoto S, Gando S, Saitoh D, Ogura H, Mayumi T, Koseki K, et al. Clinical course and outcome of disseminated intravascular coagulation diagnosed by Japanese Association for Acute Medicine criteria. Comparison between sepsis and trauma. Thromb Haemost. 2008. 100:1099–1105.

2. Petros S, Kliem P, Siegemund T, Siegemund R. Thrombin generation in severe sepsis. Thromb Res. 2012. 129:797–800.

3. Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004. 32:858–873.

4. Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008. 36:296–327.

5. Bernard GR, Vincent JL, Laterre PF, LaRosa SP, Dhainaut JF, Lopez-Rodriguez A, et al. Efficacy and safety of recombinant human activated protein C for severe sepsis. N Engl J Med. 2001. 344:699–709.

6. Ranieri VM, Thompson BT, Barie PS, Dhainaut JF, Douglas IS, Finfer S, et al. Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med. 2012. 366:2055–2064.

7. Gando S, Iba T, Eguchi Y, Ohtomo Y, Okamoto K, Koseki K, et al. A multicenter, prospective validation of disseminated intravascular coagulation diagnostic criteria for critically ill patients: comparing current criteria. Crit Care Med. 2006. 34:625–631.

8. Wagner DP, Draper EA. Acute physiology and chronic health evaluation (APACHE II) and Medicare reimbursement. Health Care Financ Rev. 1984. Suppl. 91–105.
9. Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996. 22:707–710.

10. Taylor FB Jr, Toh CH, Hoots WK, Wada H, Levi M. Scientific Subcommittee on Disseminated Intravascular Coagulation (DIC) of the International Society on Thrombosis and Haemostasis (ISTH). Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Thromb Haemost. 2001. 86:1327–1330.

11. Wada H, Sase T, Matsumoto T, Kushiya F, Sakakura M, Mori Y, et al. Increased soluble fibrin in plasma of patients with disseminated intravascular coagulation. Clin Appl Thromb Hemost. 2003. 9:233–240.

12. Silva E, de Figueiredo LF, Colombari F. Prowess-shock trial: a protocol overview and perspectives. Shock. 2010. 34:Suppl 1. 48–53.
13. Eisele B, Lamy M, Thijs LG, Keinecke HO, Schuster HP, Matthias FR, et al. Antithrombin III in patients with severe sepsis. A randomized, placebo-controlled, double-blind multicenter trial plus a meta-analysis on all randomized, placebo-controlled, double-blind trials with antithrombin III in severe sepsis. Intensive Care Med. 1998. 24:663–672.
14. Baudo F, Caimi TM, de Cataldo F, Ravizza A, Arlati S, Casella G, et al. Antithrombin III (ATIII) replacement therapy in patients with sepsis and/or postsurgical complications: a controlled double-blind, randomized, multicenter study. Intensive Care Med. 1998. 24:336–342.

15. Wiedermann CJ, Kaneider NC. A systematic review of antithrombin concentrate use in patients with disseminated intravascular coagulation of severe sepsis. Blood Coagul Fibrinolysis. 2006. 17:521–526.

16. Welcker K, Lederle J, Schorr M, Siebeck M. Surgery and adjuvant therapy in patients with diffuse peritonitis: cost analysis. World J Surg. 2002. 26:307–313.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download