Abstract
Purpose
Hypocalcemia is the most common complication after total thyroidectomy. The purpose of this study was to determine whether measurement of intact parathyroid hormone (i-PTH) level in thyroidectomy patients could predict hypocalcemia.
Materials and Methods
We performed a prospective study of patients undergoing total thyroidectomy. Serum concentration of i-PTH, total calcium (Ca), ionized calcium (Ca2+), phosphate (P), magnesium (Mg), and albumin were measured preoperatively and at 0 hour, 6 hours, 12 hours, 24 hours, 48 hours, and 72 hours postoperatively.
Results
108 patients were recruited to the study. A total of 50 patients (46%) experienced hypocalcemia. The serum i-PTH concentration was linearly related to the time of measurement, while concentrations of P, Mg, albumin, Ca, and Ca2+ were not. We compared odds ratios, and found that the concentration of i-PTH at 6 hours post operation was the most closely related to the occurrence of hypocalcemic symptom. On ROC analysis using i-PTH level at 6 hours, an i-PTH level of 10.6 mg/dL was found to maximize both sensitivity and specificity at the same time point.
Hypocalcemia is the most common etiology for prolonged hospitalization in patients undergoing total thyroidectomy.1,2 Traditional methods for detecting hypocalcemia in the postoperative period include frequent monitoring of total and ionized calcium (i-Ca) levels as well as close clinical monitoring for symptoms of hypocalcemia. These traditional methods can take 24 hours or longer to reveal hypocalcemia, which can prolong hospitalization.1,2
After total thyroidectomy, hypocalcemia may develop in cases of unexpected injury to the parathyroid glands or to the blood vessels that supply these glands.3 Despite various efforts to safely preserve the parathyroid glands, the reported incidence of hypocalcemia following surgery varies widely (5.4-50%).1-3 A need has, therefore, arisen to determine the predictive factors of hypocalcemia to prevent its occurrence, diagnose it as early as possible, and continuously monitor its development.
Many recent studies on the early predictive factors of hypocalcemia after total thyroidectomy reported that intact parathyroid hormone (i-PTH) levels predict hypocalcemia earlier than other factors,4-9 thus, facilitating earlier discharge (≤24 hours) and improving outcomes after total thyroidectomy. Nevertheless, the most useful test time and test standards for i-PTH remain controversial.
In the current study, we examined serial i-PTH levels and other factors associated with calcium metabolism in patients who underwent total thyroidectomy, from the time immediately after surgery, in order to determine the predictive factors for symptoms of hypocalcemia, as well as the most useful test time and test standards.
The protocol for this prospective clinical study was approved by the Institutional Review Board (GNUHIRB-2009-36), Gyeongsang National Medical School. A study flowchart is presented in Fig. 1. From May 2009 to March 2011, 165 patients who visited our outpatient clinic with thyroid papillary carcinoma were enrolled in this study.
The inclusion criteria were patients older than 20 years of age diagnosed with papillary thyroid carcinoma by a preoperative fine needle aspiration test and postoperative pathological tests, who agreed to enroll in the study and provided written informed consent.
The exclusion criteria included the presence of any of the following: history of head and neck malignancy, history of radiation therapy in the head and neck area, history of hyperventilation symptoms, medications affecting thyroid function, Graves' disease, hyperthyroidism, hypothyroidism, parathyroid diseases, thyroiditis, and other medical problems detected by presurgical tests. Of the initial 165 patients, 57 did not meet the eligibility criteria and were excluded from the study. The final number of patients included in the analysis was 108 patients who had undergone a total thyroidectomy by a single surgeon (Fig. 1).
The 108 patients were divided into two groups: those who developed symptoms of hypocalcemia (symptom development group) and those who did not (non-symptom development group). The age and gender of the patients and the inclusion of anterior neck dissection were compared between the two groups.
We measured the levels of factors associated with calcium metabolism (i-PTH, P, Mg, albumin, Ca, and Ca2+) before surgery and at 0 hour, 6 hours, 12 hours, 24 hours, 48 hours, and 72 hours after surgery. The development of postsurgical symptoms of hypocalcemia was defined by the presence of numbness in hands and feet, muscle stiffness, Chvostek's sign, or Trousseau's sign.
Blood collection time prior to surgery was defined as before surgery but after anesthesia; 0 hour after surgery as the time of completion of skin suturing; and 6 hours, 12 hours, 24 hours, 48 hours, and 72 hours after surgery as the time that had elapsed since surgery. The i-PTH was analyzed with an electrochemiluminescence immunoassay (ECLIA-PTH, Modular Analytics E170, Roche Diagnostics, Mannheim, Germany).
For statistical analysis, SPSS version 15.0 (SPSS Inc., Chicago, IL, USA) was used. To assess the differences between the symptom development and the non-symptom development groups, we performed the Mann-Whitney test and Fisher's exact test. To examine their correlation with the development of symptoms, we performed a stepwise method of logistic regression analysis on all factors. To assess the standard value of useful predictive factors, we used receiver operating characteristic (ROC) curves. In all statistical methods, p<0.05 was considered to be statistically significant.
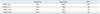
Of a total of 165 patients, 108 patients fulfilled the study inclusion criteria. Fifty patients developed symptoms of postsurgical hypocalcemia (symptom development group), and 58 patients did not (non-symptom development group). Average age, and the ratio of male to female patients were not statistically different between the two groups. However, the surgical methods used were statistically different between the two groups (Table 1).
Serum levels of i-PTH, P, Mg, albumin, Ca, and Ca2+ measured pre-operation (pre OP), as well as at 0 hour, 6 hours, 12 hours, 24 hours, 48 hours and 72 hours after surgery were divided according to whether they fell into the hypocalcemic symptom development group or the non-symptom development group, and the mean values and standard deviations were examined (Fig. 2). Unlike the results of the other tests, i-PTH showed a change in mean values with time, particularly in the symptom development group. The mean value of i-PTH in the symptom development group decreased rapidly from pre OP to 6 hours after surgery, and then slightly increased from 12 hours after surgery (Fig. 2).
The test results over time were classified into the hypocalcemic symptom development group and the non-symptom development group, and the relationship of each blood test result to the development of hypocalcemic symptoms was examined.
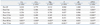
The relationship between symptoms and calcium levels was statistically significant only 48 and 72 hours after surgery, ionized calcium was significant only 48 hours, magnesium significant only 48 and 72 hours, and phosphate significant only 72 hours after surgery. The relations between i-PTH and symptoms were statistically significant from 0 hour to 72 hours after surgery (Table 2).
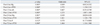
To examine the correlation of each factor with the development of symptoms, we performed a stepwise logistic regression analysis. At 6 hours after surgery, the relationships between the levels of magnesium and i-PTH and symptom development were statistically significant, as were the relationships of albumin and i-PTH at 12 hours after surgery, magnesium and i-PTH at 24 hours after surgery, and phosphate and parathyroid hormone at 72 hours after surgery (Table 3).
However, the levels of various factors did not show continuous significance in predicting symptoms of hypocalcemia except the levels of i-PTH measured after surgery. With an exception of measurements prior to surgery and at 0 hour after surgery, i-PTH levels predicted hypocalcemia with statistical significance at all times. Parathyroid hormone was found to be the only factor that could predict hypothyroid symptoms after surgery. The level of i-PTH 6 hours after surgery was 1.572 (95% confidence interval 1.128-2.191), thus confirming that i-PTH level 6 hours after surgery is valuable as a predictive factor in the development of clinical hypocalcemic symptoms.
To assess the standard value of i-PTH, we divided the measurements into four groups by using ROC curves, and compared their sensitivity and specificity in predicting symptoms of hypocalcemia. When the level of i-PTH was lower than 4.2 mg/dL, the sensitivity in predicting hypocalcemic symptoms was 31%, the specificity was 100%, and the positive predictive value (PPV) was 100%. When i-PTH was lower than 7.1 mg/dL, the sensitivity was 79%, the specificity was 78%, and the PPV was 88%. When measured i-PTH was lower than 10.6 mg/dL, the sensitivity was 89%, the specificity was 88%, and the PPV was 85%. Finally, when the concentration of i-PTH was lower than 13.6 mg/dL, the sensitivity was 95%, the specificity was 75%, and the PPV was 81% (Table 4). Therefore, considering the sensitivity, specificity, and positive predictive value, an i-PTH concentration of 10.6 mg/dL was found to be the most useful predictor of symptoms (Fig. 3).
After thyroid surgery, hypocalcemia is induced by direct injury of the parathyroid glands, adjacent blood vessels, or other adjacent structures,1-13 and a broad range in the incidence of such cases of hypocalcemia has been reported (5.4-50%).1-3 Hypocalcemia not only inconveniences the patient, but may also lead to fatalities.1-3
Numerous studies have been conducted on the factors involved in the early prediction of hypocalcemia following thyroidectomy, most of which measured postsurgical i-PTH and calcium levels.5-10 While calcium levels have been shown to have limited applicability as predictive factors, i-PTH levels have been reported to be useful in the prediction of postoperative hypocalcemia. Nonetheless, times at which concentrations were measured and reported values differ among investigators, therefore, the application of a test of i-PTH levels in predicting the development of clinical symptoms has remained controversial.
To determine the factors that may be useful in predicting the development of hypocalcemia, we measured the serum levels of i-PTH, P, Mg, albumin, Ca, and Ca2+ at 0, 6, 12, and 24 hours after thyroid surgery, as well as once daily for several days (48 hours and 72 hours following surgery), and comprehensively analyzed the changes in each test value. The first postsurgical blood collection time after 0 hour was decided to be 6 hours after thyroidectomy, because the process of patient waking from anesthesia, being transferred to a ward, and resting requires 6 hours. Furthermore, a certain amount of time is necessary for several components within the body fluid to stabilize. In fact, in the hypocalcemic symptom development group, the parathyroid hormone level at 6 hours after surgery showed the lowest mean value in comparison with the mean values measured at all other times (Fig. 2). The half-life of i-PTH in vivo is 3 to 4 minutes, therefore, at the time of blood collection, the condition of the parathyroid glands should be immediately reflected in the level of i-PTH; nonetheless, the test performed immediately after surgery showed higher values than the test performed 6 hours postoperatively. We speculate that the parathyroid function did not stabilize for a certain period after surgery, and that the inefficient blood circulation that developed during surgery continued to deteriorate up until a certain point, but improved thereafter.14
By applying the Mann-Whitney test, which considers the test results of the defined times as a single variable, we examined the association of each blood test result with the development of hypocalcemic symptoms, and observed that the relationship between symptoms of hypocalcemia and i-PTH concentrations measured at all time points was statistically significant (Table 2). However, in examining the relationship between the test results and hypocalcemic symptoms by logistic regression analysis, which considers all factors as continuous variables, we found that the relationship between hypocalcemic symptoms and parathyroid hormone was not statistically significant at 0 hour after surgery, however, it was statistically significant at 6 hours, 12 hours, and 72 hours after surgery. When odds ratio values were assessed using a stepwise method, i-PTH level at 6 hours after surgery showed the highest correlation with the development of symptoms of hypocalcemia (Table 3).
In the present study, we confirmed the i-PTH level as a predictor of hypocalcemia in thyroidectomy patients. The results of logistic regression analysis also showed that the levels of magnesium at 6 hours, albumin at 12 hours, magnesium at 24 hours, and phosphate at 72 hours after surgery were statistically significant predictors of the development of hypocalcemic symptoms. These results were not temporally continuous, however, and are thus considered not significant (Table 3).
An i-PTH is metabolized in the liver and kidney, and has a half-life as short as 3 minutes, therefore, it can be measured very shortly after total thyroidectomy; hence, it can accurately determine parathyroid function. On the other hand, other factors (P, Mg, albumin, Ca, and Ca2+) affect the deterioration of parathyroid function after surgery, and thus the changes appear to be delayed or homeostasis is maintained; hence, changes in function are not always shown early on.8 To determine the standard for early diagnosis of the development of hypocalcemic symptoms, we determined the cutoff values for parathyroid hormone values (6 hours after surgery) by using ROC analysis. When the parathyroid hormone level was lower than 10.6 mg/dL, the sensitivity for the development of hypocalcemic symptoms was 89%, the specificity was 88%, and the positive predictive value was 85%, and high values occurred; thus, this level maximizes both sensitivity and specificity at the same time point (Fig. 3).
If the development of hypocalcemic symptoms can be predicted by prognostic factors, these symptoms could be prevented by advance administration of calcium agents. Patients whose level of risk for the development of hypocalcemic symptoms is low could be discharged early, thereby reducing the inconvenience of hospitalization and its associated costs.5,9,15-17 If it is thought that the development of hypocalcemia symptoms is a possibility in patients who are discharged early, these symptoms might easily be resolved by prescribing emergency calcium agents at the time of discharge, thoroughly explaining the symptoms associated with hypocalcemia, and advising patients to take prescribed calcium agents and return to the hospital when unexpected symptoms occur.
This study is not without limitation. More accurate measurement timings could have been found if i-PTH had been measured every hour. In reality, however, it is hard to obtain a sample from a patient every hour. Another shortcoming of this study is that it would have been better if hypocalcemia patients had been divided into those with symptomatic hypocalcemia and biochemical hypocalcemia.
In conclusion, on the basis of statistically significant results obtained in this study, we confirmed that the earliest possible predictor of the development of symptoms of hypocalcemia was a serum i-PTH concentration of less than 10.6 mg/dL 6 hours after surgery. We propose that these patients need further inpatient monitoring for safe discharge. Furthermore, patients with less than 10.6 mg/dL decrease of PTH at 6-hour time point are unlikely to develop hypocalcemia and may be considered safe for discharge.
Figures and Tables
 | Fig. 2Comparison by Mann-Whitney test of preoperative and postoperative serum concentrations between patients with and without hypocalcemic symptoms. Ca, calcium; i-Ca, ionized calcium; Mg, magnesium; P, phosphate; alb, albumin; i-PTH, intact parathyroid hormone; Pre, preoperative; Post, postoperative; No, patients with no hypocalcemic symptoms; Hypo, Patients with hypocalcemic symptoms; OP, operation; h, hour. |
 | Fig. 3Receiver operating characteristic (ROC) analysis for the prediction of hypocalcemic symptoms, based on 6-hour post-thyroidectomy i-PTH values. For 6-hour i-PTH ≤10.6 mg/dL, specificity is 88% and sensitivity is 89%. Area under an ROC curve=0.931. i-PTH, intact parathyroid hormone. |
Table 1
Comparison of Patients with Normocalcemia and Symptomatic Hypocalcemia after Total Thyroidectomy
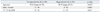
Table 2
Comparison of Preoperative and Postoperative Laboratory Data p-Values in 108 Patients by Mann-Whitney Test
References
1. Lindblom P, Westerdahl J, Bergenfelz A. Low parathyroid hormone levels after thyroid surgery: a feasible predictor of hypocalcemia. Surgery. 2002. 131:515–520.

2. McHenry CR, Speroff T, Wentworth D, Murphy T. Risk factors for postthyroidectomy hypocalcemia. Surgery. 1994. 116:641–647.
3. Sturniolo G, Lo Schiavo MG, Tonante A, D'Alia C, Bonanno L. Hypocalcemia and hypoparathyroidism after total thyroidectomy: a clinical biological study and surgical considerations. Int J Surg Investig. 2000. 2:99–105.
4. Grodski S, Farrell S. Early postoperative PTH levels as a predictor of hypocalcaemia and facilitating safe early discharge after total thyroidectomy. Asian J Surg. 2007. 30:178–182.

5. Grodski S, Serpell J. Evidence for the role of perioperative PTH measurement after total thyroidectomy as a predictor of hypocalcemia. World J Surg. 2008. 32:1367–1373.

6. Khafif A, Pivoarov A, Medina JE, Avergel A, Gil Z, Fliss DM. Parathyroid hormone: a sensitive predictor of hypocalcemia following total thyroidectomy. Otolaryngol Head Neck Surg. 2006. 134:907–910.

7. Payne RJ, Hier MP, Tamilia M, Mac Namara E, Young J, Black MJ. Same-day discharge after total thyroidectomy: the value of 6-hour serum parathyroid hormone and calcium levels. Head Neck. 2005. 27:1–7.

8. Sywak MS, Palazzo FF, Yeh M, Wilkinson M, Snook K, Sidhu SB, et al. Parathyroid hormone assay predicts hypocalcaemia after total thyroidectomy. ANZ J Surg. 2007. 77:667–670.

9. Vescan A, Witterick I, Freeman J. Parathyroid hormone as a predictor of hypocalcemia after thyroidectomy. Laryngoscope. 2005. 115:2105–2108.

10. Kim JH, Chung MK, Son YI. Reliable early prediction for different types of post-thyroidectomy hypocalcemia. Clin Exp Otorhinolaryngol. 2011. 4:95–100.

11. Pattou F, Combemale F, Fabre S, Carnaille B, Decoulx M, Wemeau JL, et al. Hypocalcemia following thyroid surgery: incidence and prediction of outcome. World J Surg. 1998. 22:718–724.

12. Choi SJ, Kim TY, Lee JC, Shong YK, Cho KJ, Ryu JS, et al. Is routine central neck dissection necessary for the treatment of papillary thyroid microcarcinoma? Clin Exp Otorhinolaryngol. 2008. 1:41–45.

13. Lee SH, Lee SJ, Jin SM, Lee NH, Kim DH, Chae SW, et al. Relationships between lymph node metastasis and expression of CD31, D2-40, and vascular endothelial growth factors A and C in papillary thyroid cancer. Clin Exp Otorhinolaryngol. 2012. 5:150–155.

14. Lombardi CP, Raffaelli M, Princi P, Santini S, Boscherini M, De Crea C, et al. Early prediction of postthyroidectomy hypocalcemia by one single iPTH measurement. Surgery. 2004. 136:1236–1241.

15. Cote V, Sands N, Hier MP, Black MJ, Tamilia M, MacNamara E, et al. Cost savings associated with post-thyroidectomy parathyroid hormone levels. Otolaryngol Head Neck Surg. 2008. 138:204–208.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download