Abstract
Purpose
Monocyte chemoattractant protein-1 (MCP-1) is a chemokine that can increase adhesion molecule expression on monocytes and produce superoxide anions. Hyperglycemia induces MCP-1 production in vascular endothelial cells and retinal pigmented epithelial cells, and has been implicated as a causal factor in the facilitation of vascular complications in diabetes. In the present study, we evaluated the association of a single nucleotide polymorphism (SNP) in the MCP-1 gene with proliferative diabetic retinopathy (PDR) in a Korean population with type 2 diabetes.
Materials and Methods
We conducted a case-control study, which enrolled 590 subjects with type 2 diabetes, and SNP genotyping of c.2518A/G in the MCP-1 gene was performed using polymerase chain reaction followed by digestion with PvuII restriction enzyme.
Results
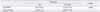
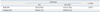
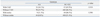
The prevalence of c.2518A/G polymorphism in diabetic patients was 13.2% (A/A), 47.1% (A/G) and 39.7% (G/G). In patients with diabetic retinopathy, the prevalence of PDR was significantly higher (p=0.009) in diabetic subjects with the c.2518A/A genotype (35.9%; n=78) compared to those with either the A/G or G/G genotype (22.3%, n=512). The prevalence of any other micro and macro-complications, including nephropathy and cerebrovascular events, were not different according to the c.2518A/G genotype.
Proliferative diabetic retinopathy (PDR) is a serious diabetic microvascular complication as a consequence of active angiogenesis in the etina.1 It is a leading cause of visual loss with a substantial impact on the quality of life of diabetic patients. It has been observed that neovascularization plays a pivotal role in the development of PDR. This process involves the migration and proliferation of endothelial cells as well as the remodeling of the extracellular matrix.2-4 The pathogenic mechanism of PDR remains to be fully elucidated, but several cytokines and chemokines, including vascular endothelial growth factor, intercellular adhesion molecule-1, transforming growth factor have been suggested in the etiology of PDR.5-8 Recently, a potent cytokine, monocyte chemoattractant protein-1 (MCP-1), was shown to exert a plethora of effects, including superoxide production, cytokine expression, and induction of adhesion molecule expression. More importantly, it has been shown to play a possible role as a modulator of PDR due to its ability to regulate arterial smooth muscle cell proliferation and induce retinal neovascularization.9-11 Intraocular MCP-1 level is significantly increased in PDR and is associated with clinical stage of PDR.12,13 A recent study identified that genetic variations in the MCP-1 gene influences MCP-1 production and function. Recent studies have identified a biallelic A/G polymorphism in the 5' flanking region at position -2518 of the MCP-1 gene, which influences MCP-1 expression in response to an inflammatory stimulus.14 This genetic variability correlates with individual differences in monocyte MCP-1 production and may be responsible for clinical differences in disease severity.
Because of the importance of MCP-1 in the biology of PDR and the genetic single nucleotide polymorphism (SNP) evidence for role in the regulation of MCP-1 production, we postulated that there may be an association between MCP-1 c.2518A/G with the pathogenesis of PDR. This study was designed to evaluate a sub-population of Korean patients exhibiting type 2 diabetes with or without PDR.
A case-control study was designed in which 590 type 2 diabetic patients were enrolled with a defined ophthalmologic status. This study was approved by the Institutional Review Board of Chungbuk National University Hospital, and all patients gave informed consent prior to being included in the study. Inclusion criteria were age at diagnosis of diabetes ≥30 years and a known duration of diabetes of ≥5 years. Diabetes was diagnosed according to WHO criteria.15 All patients underwent biochemical tests and medical history. Diabetic retinopathy was assessed through dilated pupils by trained ophthalmologists. The patients were classified using the criteria based on the International Clinical Retinopathy Severity Scale: 1) no apparent diabetic retinopathy; 2) non-proliferative diabetic retinopathy (NPDR); or 3) PDR. Diabetic nephropathy was defined by the presence of microalbuminuria or overt albuminuria. Macrovascular complications, such as coronary artery disease or stroke, were assessed according to the available medical records.
Peripheral leukocytes were isolated from EDTA-treated whole blood obtained from each patient, and genomic DNA was extracted for polymerase chain reaction (PCR) amplification of MCP-1. The following primers were used for amplification: forward 5'-CCGAGATGTTCCCAGCACAG-3' and reverse 5'-CTGCTTTGCTTGTGCCTCTT-3'. The DNA was amplified by cycling at 94° for 1 minute, 55° for 1 minute, and 72° for 1.5 minutes. After 40 cycles, the reaction was extended for an additional 10 minutes at 72°. The amplified PCR product was subsequently restriction digested overnight at 37° with PvuII (5U).14 Agarose gel electrophoresis of the digested products were analyzed to determine the presence of the various genotypes: 1) A/A genotype yields only a single 930 bp band; 2) G/G genotype results in two bands (222 bp and 708 bp); and 3) A/G genotype results in three bands (222 bp, 708 bp and 930 bp).
All statistical tests were performed with SPSS version 12.0 (SPSS Inc., Chicago, IL, USA). Genotype frequencies were calculated from the observed numbers. Hardy-Weinberg equilibrium was tested with the χ2 test. The data was expressed as mean±standard deviation. Means and frequencies of variables were evaluated using Student's t-test, and χ2 test, respectively. All p values <0.05 were considered statistically significant.
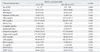
In our subject population, 142 patients were diagnosed with proliferative diabetic retinopathy and the remaining 448 patients were categorized as having NPDR. The demographics of the study population according to the MCP-1 c.2518A/G genotype are summarized in Table 1. The clinical characteristics did not differ among genotype subgroups.
Genetic variation in the SNP analysis of c.2518A/G in the MCP-1 gene was analyzed with the following distribution: A/A (13.2%), A/G (47.1%) and G/G (39.7%). The genotypic distribution of the MCP-1 c.2518A/G was in Hardy-Weinberg equilibrium. In terms of severity of diabetic retinopathy (Table 2), the prevalence of PDR was significantly higher (p=0.009) in subjects with the c.2518A/A genotype (35.9%; 28/78 patients) compared to those carrying either the A/G or G/G genotype [22.3% (114/512)].
The pathogenesis of PDR remains poorly understood. Recent studies have implicated a number of cytokines and chemokines in the activation of a complex network of pathways to promote cellular migration and proliferation.5-8 In conjunction with these factors, there appears to be a critical role for genetics in the regulation of PDR, since only a subgroup of diabetic patients develop PDR, even between PDR and NPDR patients with similar glycemic control and duration of diabetes.
Among the genetic factors being considered as a susceptibility gene for PDR, MCP-1 is known to be associated with diabetic microvascular or macrovascular complications. MCP-1 is a chemokine that exerts several effects on monocytes and macrophages including induction of superoxide anion, cytokine production, and adhesion molecule expression. Moreover, intraocular MCP-1 levels have been shown to be significantly increased in diabetic retinopathy (DR) and associated with clinical stage of DR.13,14
In the present study, the prevalence of PDR was significantly higher in diabetic patients with the c.2518A/A genotype compared to those with either the A/G or G/G genotype. However, the relationship between SNP polymorphism c.2518A/G in the MCP-1 gene with diabetic retinopathy remains controversial. Katakami, et al.16 reported that the G allele in the c.2518A/G polymorphism is a susceptibility allele for diabetic retinopathy in a Japanese population of diabetic patients. In this study, however, the mean duration of diabetes was for only a length of 9 years, which was much shorter than in other published studies.17-19 In another Japanese study, Yoshioka, et al.20 showed that there was no association between c.2518A/G polymorphism of the MCP-1 gene with diabetic retinopathy in a group of Japanese patients with type 2 diabetes. This study did not match the duration of diabetes and glycemic control with the previous study by Katakami, et al.16 Towards this end, our study was designed to match both the duration of diabetes (>12 years) and glycemic control between the various genotypes, i.e., A/A and A/G+G/G. Using this approach, the number of PDR patients was significantly higher in the A/A genotype population compared to those in the other A/G+G/G genotype population. This data would suggest that the c.2518A/A genotype of the MCP-1 gene could be a potential risk factor for PDR in Korean type 2 diabetic patients. The difference in the nucleotide that was associated with PDR between the current study and the Katakami, et al.16 may be attributed to ethnic variation.
In other microvascular complications observed in diabetes, such as nephropathy and MCP-1 polymorphism, Moon, et al.21 showed that carriage of the A allele of MCP-1 c.2518A/G polymorphism was associated with a susceptibility to kidney failure in patients with Korean type 2 diabetes. In our study, there was no association of the 2518A/G SNP with diabetic nephropathy. This may be due to differences in the types of patients that were recruited for the Moon, et al.21 study, who included 112 hemodialyzed patients with kidney failure. This was not a selection criterion in our protocol and we did not have any patients in this category. The role of the c.2518A/G polymorphism may play an important diagnostic role in kidney disease detection. Kim, et al.22 reported that urinary MCP-1 concentration was much greater in A/A genotype patients compared to the other genotypes in Korean patients with lupus nephritis. These results would suggest that the A allele of MCP-1 c.2518A/G polymorphism may be associated with kidney diseases in Korean patients.
In cardiovascular disease (CVD) and MCP-1 polymorphism, Buraczynska, et al.23 showed that the G allele of the MCP-1 gene is associated with an increased risk of CVD in hemodialyzed renal failure patients. In our study, MCP-1 polymorphism was not associated with CVD. Different patient traits and ethnicity may explain the differences in the role of the SNP in the MCP-1 gene with various other phenotypes. Interestingly, the distribution of allele frequency in the MCP-1 gene was different between Caucasian and Asian patients. G allele carriers were more prevalent in Asian populations (G allele : A allele=60 : 40), while A allele carriers were more prevalent in Caucasian populations (G allele : A allele=40 : 60).
There are some limitations to our study that could impact our conclusions. First, this was a cross-sectional study, and as such, we did not measure plasma MCP-1 in this study. For more accurate results, prospective studies will be needed to investigate the role of MCP-1 polymorphism in PDR in type 2 diabetic patients, and a larger prospective genome wide association study that includes family history will be required to fully clarify the pathogenesis of PDR in type 2 diabetic patients.
In conclusion, this study suggests that the c.2518A/G polymorphism in the MCP-1 gene can be used as a novel method to detect susceptibility to PDR manifestation in Koreans with type 2 diabetes.
Figures and Tables
Table 1
Clinical Characteristics of Patients with Type 2 Diabetes According to the MCP-1 c.2518A/G SNP
ACKNOWLEDGEMENTS
This work was supported by a research grant 2010 from Chungbuk National University.
References
2. Adamiec-Mroczek J, Oficjalska-Młyńczak J, Misiuk-Hojło M. Proliferative diabetic retinopathy-the influence of diabetes control on the activation of the intraocular molecule system. Diabetes Res Clin Pract. 2009. 84:46–50.

3. Leal EC, Santiago AR, Ambrósio AF. Old and new drug targets in diabetic retinopathy: from biochemical changes to inflammation and neurodegeneration. Curr Drug Targets CNS Neurol Disord. 2005. 4:421–434.

4. Fong DS, Aiello LP, Ferris FL 3rd, Klein R. Diabetic retinopathy. Diabetes Care. 2004. 27:2540–2553.

5. Simó R, Carrasco E, García-Ramírez M, Hernández C. Angiogenic and antiangiogenic factors in proliferative diabetic retinopathy. Curr Diabetes Rev. 2006. 2:71–98.

6. Crawford TN, Alfaro DV 3rd, Kerrison JB, Jablon EP. Diabetic retinopathy and angiogenesis. Curr Diabetes Rev. 2009. 5:8–13.

7. Hernández C, Burgos R, Cantón A, García-Arumí J, Segura RM, Simó R. Vitreous levels of vascular cell adhesion molecule and vascular endothelial growth factor in patients with proliferative diabetic retinopathy: a case-control study. Diabetes Care. 2001. 24:516–521.
8. Beránek M, Kanková K, Benes P, Izakovicová-Hollá L, Znojil V, Hájek D, et al. Polymorphism R25P in the gene encoding transforming growth factor-beta (TGF-beta1) is a newly identified risk factor for proliferative diabetic retinopathy. Am J Med Genet. 2002. 109:278–283.

9. Niu J, Kolattukudy PE. Role of MCP-1 in cardiovascular disease: molecular mechanisms and clinical implications. Clin Sci (Lond). 2009. 117:95–109.

10. Kolattukudy PE, Niu J. Inflammation, endoplasmic reticulum stress, autophagy, and the monocyte chemoattractant protein-1/CCR2 pathway. Circ Res. 2012. 110:174–189.

11. Deshmane SL, Kremlev S, Amini S, Sawaya BE. Monocyte chemoattractant protein-1 (MCP-1): an overview. J Interferon Cytokine Res. 2009. 29:313–326.

12. Capeans C, De Rojas MV, Lojo S, Salorio MS. C-C chemokines in the vitreous of patients with proliferative vitreoretinopathy and proliferative diabetic retinopathy. Retina. 1998. 18:546–550.

13. Mitamura Y, Takeuchi S, Matsuda A, Tagawa Y, Mizue Y, Nishihira J. Monocyte chemotactic protein-1 in the vitreous of patients with proliferative diabetic retinopathy. Ophthalmologica. 2001. 215:415–418.

14. Rovin BH, Lu L, Saxena R. A novel polymorphism in the MCP-1 gene regulatory region that influences MCP-1 expression. Biochem Biophys Res Commun. 1999. 259:344–348.

15. Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003. 26:Suppl 1. S5–S20.
16. Katakami N, Matsuhisa M, Kaneto H, Matsuoka TA, Imamura K, Ishibashi F, et al. Monocyte chemoattractant protein-1 (MCP-1) gene polymorphism as a potential risk factor for diabetic retinopathy in Japanese patients with type 2 diabetes. Diabetes Res Clin Pract. 2010. 89:e9–e12.

17. Malecki MT, Cyganek K, Mirkiewicz-Sieradzka B, Wolkow PP, Wanic K, Skupien J, et al. Alanine variant of the Pro12Ala polymorphism of the PPARgamma gene might be associated with decreased risk of diabetic retinopathy in type 2 diabetes. Diabetes Res Clin Pract. 2008. 80:139–145.

18. Petrovic MG, Kunej T, Peterlin B, Dovc P, Petrovic D. Gly482Ser polymorphism of the peroxisome proliferator-activated receptor-gamma coactivator-1 gene might be a risk factor for diabetic retinopathy in Slovene population (Caucasians) with type 2 diabetes and the Pro12Ala polymorphism of the PPARgamma gene is not. Diabetes Metab Res Rev. 2005. 21:470–474.
19. Stefanski A, Majkowska L, Ciechanowicz A, Frankow M, Safranow K, Parczewski M, et al. Lack of association between the Pro12Ala polymorphism in PPAR-gamma2 gene and body weight changes, insulin resistance and chronic diabetic complications in obese patients with type 2 diabetes. Arch Med Res. 2006. 37:736–743.

20. Yoshioka K, Yoshida T, Kogure A, Takakura Y, Umekawa T. Monocyte chemoattractant protein-1 -2518 polymorphism is not associated with diabetic retinopathy in Japanese type 2 diabetes. Diabetes Metab Syndr: Clin Res Rev. 2009. 3:166–168.

21. Moon JY, Jeong L, Lee S, Jeong K, Lee T, Ihm CG, et al. Association of polymorphisms in monocyte chemoattractant protein-1 promoter with diabetic kidney failure in Korean patients with type 2 diabetes mellitus. J Korean Med Sci. 2007. 22:810–814.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download