Abstract
Purpose
Urinary tract infection (UTI) is an ascending infection of fecal uropathogens, urogenital lactobacilli are suggested to play a role in the prevention of UTI. This study was to investigate whether lactobacillus mixture (LM) could prevent the experimental infantile UTI.
Materials and Methods
The LM were composed of three lactobacillus strains (L. gasseri, L. rhamnosus, and L. reuteri). Mother rats were grouped as lactobacillus (LB) group I (LB I, n=22), II (LB II, n=24) and control (n=20). LB I and LB II were fed with LM (1 mL/day) and control with phosphate-buffered saline (PBS) from late pregnancy through lactation. All newborn rats were breast-fed and their urine and stool were collected at the end of the 3rd week to compare lactobacillus colony. Then, infant rats from LB II were treated with intravesical instillation of LM. Infant rats from LB I and control were instilled with PBS. Twenty-four hours later, experimental UTI was introduced by intravesical instillation of standard E. coli strain. After 72 hours later, the infant rats were sacrificed for histologic examination.
Results
Lactobacilli colonies in urine and stool were not statistically different among the three groups. The incidence of pyelonephritis in the LB II was 16.7% (4/24), LB I 72.7% (16.22) and control 75.0% (15/20) (p=0.015). The incidence of cystitis was not significantly different among the three groups.
Urinary tract infection (UTI) is the most common bacterial infection in infants and has been documented as an ascending infection of the patient's own fecal uropathogens, evidenced by genomic profiling study.1 Therefore, the role of lactobacillus, the most dominant urogenital microflora, has been a focus in preventing UTI.2,3
Intraurethrally instilled lactobacillus strains were proven to prevent experimental UTI in adult animal models,4-6 and clinical application of lactobacillus suppositories showed beneficial effects in reducing the recurrence rate of UTI in adult women.7-9 However, the preventive effect of oral lactobacillus probiotics against UTI has not sufficiently been investigated in adults.10,11
In early infancy when the UTI incidence is extremely high, postnatal development of genitourinary lactobacilli is considered very important in preventing UTI. It was confirmed that some maternal lactobacilli are transferred to their infants during birth and through breast milk.12-14 Probiotic lactobacilli, administered to lactating mother rats, were also proven to be transferred to their infant guts15,16 and then to genitourinary tract.17 However, a question of whether this mother to infant transmission prevents infantile UTI has not been clarified.
Therefore, we evaluated whether lactobacilli orally administered to pregnant and lactating mother rats could prevent experimental UTI of their infant rats, and compared the effects with those of intravesically instilled lactobacilli to infant rats.
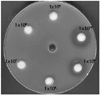
For this study, we selected three lactobacillus strains (L. gasseri, L. rhamnosus, L. reuteri), which were isolated from the healthy infant feces and mixed. For optimal dosage, the lactobacillus mixture (LM) was incubated in the DeMan-Rogosa-Sharpe (MRS) agar medium to make six different dosages [106-1011 colony forming unit (CFU)/mL], which were tested for the antimicrobial activities against standard E. coli strain (ATCC No. 25922, Seattle, WA, USA). We selected the dosage 1010 CFU/mL, whose antimicrobial activity was maximal (Fig. 1).
Forty-eight breast-fed Sprague Dawley infant rats (Seoul, Korea), whose mother rats were fed the LM (1 mL/day) via gavage tube from late pregnancy through lactation, were evenly allocated to the lactobacillus (LB) I (n=24) or II group (n=24). The control group included 20 infant rats, whose mother rats were given phosphate-buffer solution (PBS, 1 mL). All infant rats were breast-fed for 3 weeks, when the same LM (1 mL) was intravesically instilled to infant rats of the LB II group and PBS to those of the LB I and the control group. The study protocol was approved by the ethical committee of the hospital.
At age 3 weeks of infant rats, urines and stools were collected. Fecal specimens were placed to a 50 mL test tube together with sterile saline and shaken for 1 minute. For lactobacillus culture, urines and diluted fecal supernatants (200 µL) were inoculated into lactobacillus-selective MRS agar (Oxoid, Basingstroke, UK) and incubated anaerobically at 37℃ for 48 hours. Lactobacillus was confirmed by Gram-positive white, smooth bacillus, and colonies (CFU/mL) were counted.
After completion of stool and urine collection, the same LM (1 mL), given to the mother rats, was instilled into the bladder of infant rats of the LB II group using a 16-gauge silicone catheter after ketamine anesthesia. PBS (1 mL) was instilled into LB I and the control group.
Twenty-four hours after intravesical instillation of the LM or PBS, 1 mL of standard E. coli strain (107 CFU/mL) was instilled into the bladder of infant rats to induce experimental E. coli UTI through a 16-gauge silicone catheter after ketamine anesthesia.
Seventy-two hours after intravesical instillation of E. coli, the infant rats were sacrificed for histopathologic examination. Both kidneys and bladder were extracted and fixed for 24 hours in 10% buffered formalin solution. The kidney was embedded in paraffin, sectioned 3 µm in thickness using a rotatory microtome, and Hematoxylin-Eosin staining and Masson-Trichrome staining were performed. According to the histopathological changes, cystitis and pyelonephritis were diagnosed and the incidence was compared. For semiquantative evaluation, the severity of inflammation in cystitis and pyelonephritis was scored. The cystitis score ranged from 0 to 3 (0 point without inflammatory cells, 1 point with a few inflammatory cells in the submucosa, 2 points with more than 5 focal inflammatory cells in the submucosa, and 3 points with diffuse inflammatory cells in the submucosa). The pyelonephritis score ranged from 0 to 4 (0 point without inflammation, 1 point with occasional inflammation in the pelvic mucosa, 2 points with continuous inflammation along the pelvic mucosa, 3 points with focal inflammation from the pelvic mucosa to the renal medulla, and 4 points with diffuse inflammation to the renal medulla).
For statistical analysis, SPSS version 11.5 (SPSS Inc., Chicago, IL, USA) was used. ANOVA test was performed for comparison of the number of lactobacillus or E. coli, histopathological findings, the incidence and the score of cystitis and pyelonephritis between LB I, II and control groups. For the comparison of the number of lactobacillus and E. coli CFU/mL after experimental E. coli UTI, Wilcoxon signed rank test was used. p value less than 0.05 was determined to be statistically significant.
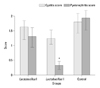
The numbers of lactobacillus CFUs in the stools of infant rats were 3.5×108±6.6×107 CFU/mL in the LB I group, 4.1×108±2.5×108 CFU/mL in the LB II group, and 1.7×107± 7.3×106 CFU/mL in the control group (p>0.05). The numbers of lactobacillus CFUs in the urines of infant rats were 2930±314.4 CFU/mL in the LB I group, 5892±370.5 CFU/mL in the LB II group, and 1658±361.1 CFU/mL in the control group (p>0.05) (Fig. 2).
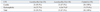
The incidence of cystitis was 95.5% (21/22) in the LB I group, 87.5% (21/24) in the LB II group, and 100% (20/20) in the control group (p>0.05). The incidence of pyelonephritis was 16.7% (4/24) in the LB II group, which was significantly lower than 75.0% (15/20) of the control group (p=0.015) (Table 1).
The cystitis score of the LB II group (1.25±0.98) was lower than those of the LB I group (1.5±0.78) and control group (1.8±1.06) (p>0.05) (Fig. 3). The pyelonephritis score of the LB II group (0.33±0.68) was significantly lower than those of the LB I group (1.31±1.21) and control group (1.95±1.72) (p=0.006) (Fig. 3).
In preventing infantile UTI, postnatal development of genitourinary lactobacilli is considered very important. Indeed, lactobacilli in the maternal vagina are the first source of lactobacilli of newborn infants. While passing through the birth canal, maternal vaginal lactobacilli are transferred to the sterile neonate's gut for the first time.12 Lactobacilli in breast milk are the second important source of infant's gut lactobacilli.13 Approximately 6 days after birth, the number of CFU/mL of lactobacillus in the feces of breast-fed infants was 1000 times more than that of enterobacteriae, but 10 times less in the feces of bottle-fed infants.14 Probiotic lactobacilli, supplied during pregnant and lactating period, were proved to colonize the infant's gut.15,16 These vertically transmitted lactobacilli are transferred from gut to genitourinary tract.17
Many earlier studies demonstrated that the number of urogenital lactobacilli is significantly decreased in infants with UTI18 as well as in woman with urethritis and recurrent UTI.7-9,19-22 Antimicrobial activities of lactobacillus strains against uropathogens have been studied in many in vitro tests.23-26 Lactobacillus strains imped the adherence of uropathogens by secreting biosurfactants,23 compete with uropathogens in the binding site on vaginal epithelial cells,24 and inhibit the growth of uropathogens by secreting hydrogen peroxide, lactate, bacteriocin, and other antimicrobial molecules.25 They also enhance the local immunity of the intestinal mucosa, and improve the innate immunity and cell-mediated immunity by activating monocytes.26
The preventive effects of intravesically instilled lactobacilli against UTI have been proven in adult animal models with different strains and different dosages.4-6 When L. casei GR1 (5×109 CFU/mL), isolated from healthy adult women, was intravesically instilled to adult rats and was then swabbed twice weekly for 21 days onto the introitus before challenge with an uropathogen suspension (E. coli, K. pneumoniae, P. aerusinosa), experimental UTI was prevented in 84% of the animals.4 L. casei shirota strain (1×108 CFU/day), when administered intraurethrally to a mouse 24 hours prior to the induction of experimental E. coli, dramatically inhibited E. coli growth and inflammatory responses in the urinary tract.5 Furthermore, intraurethral instillation of the indigenous L. murinus strain (1×108 CFU/mL) also significantly prevented Proteus mirabilis ascending UTI in a mouse model.6
In the present study, intravesically instilled lactobacilli to infant rats showed the significant preventive effect against experimental pyelonephritis, whereas orally administered lactobacilli to pregnant and lactating mother rats did not prevent the infection of their infant rats. This might be due to insufficient increase of lactobacillus colonization in their stools and urines. Further studies are necessary to find ideal lactobacillus strains and an optimal oral dosage that are compatible with preventive effect of intravesically instilled lactobacillus.
Figures and Tables
Fig. 1
Inhibitory zone (diameter, mm) at different dosage of lactobacilllus mixture against standard E. coli (ATCC 25922). The optimal dosage (CFU/mL) for maximal inhibition was dertermined as 1×1010 CFU/mL.
References
1. Usein CR, Damian M, Tatu-Chiţoiu D, Căpuşă C, Făgăraş R, Mircescu G. Comparison of genomic profiles of Escherichia coli isolates from urinary tract infections. Roum Arch Microbiol Immunol. 2003. 62:137–154.
2. Redondo-Lopez V, Cook RL, Sobel JD. Emerging role of lactobacilli in the control and maintenance of the vaginal bacterial microflora. Rev Infect Dis. 1990. 12:856–872.

3. Reid G, Bruce AW. Probiotics to prevent urinary tract infections: the rationale and evidence. World J Urol. 2006. 24:28–32.

4. Reid G, Chan RC, Bruce AW, Costerton JW. Prevention of urinary tract infection in rats with an indigenous Lactobacillus casei strain. Infect Immun. 1985. 49:320–324.

5. Asahara T, Nomoto K, Watanuki M, Yokokura T. Antimicrobial activity of intraurethrally administered probiotic Lactobacillus casei in a murine model of Escherichia coli urinary tract infection. Antimicrob Agents Chemother. 2001. 45:1751–1760.

6. Fraga M, Scavone P, Zunino P. Preventive and therapeutic administration of an indigenous Lactobacillus sp. strain against Proteus mirabilis ascending urinary tract infection in a mouse model. Antonie Van Leeuwenhoek. 2005. 88:25–34.

7. Reid G, Bruce AW, Taylor M. Instillation of Lactobacillus and stimulation of indigenous organisms to prevent recurrence of urinary tract infection. Microecol Ther. 1995. 23:32–45.
8. Uehara S, Monden K, Nomoto K, Seno Y, Kariyama R, Kumon H. A pilot study evaluating the safety and effectiveness of Lactobacillus vaginal suppositories in patients with recurrent urinary tract infection. Int J Antimicrob Agents. 2006. 28:Suppl 1. S30–S34.

9. Stapleton AE, Au-Yeung M, Hooton TM, Fredricks DN, Roberts PL, Czaja CA, et al. Randomized, placebo-controlled phase 2 trial of a Lactobacillus crispatus probiotic given intravaginally for prevention of recurrent urinary tract infection. Clin Infect Dis. 2011. 52:1212–1217.

10. Lee SJ, Shim YH, Cho SJ, Lee JW. Probiotics prophylaxis in children with persistent primary vesicoureteral reflux. Pediatr Nephrol. 2007. 22:1315–1320.

11. Abad CL, Safdar N. The role of lactobacillus probiotics in the treatment or prevention of urogenital infections--a systematic review. J Chemother. 2009. 21:243–252.

12. Matsumiya Y, Kato N, Watanabe K, Kato H. Molecular epidemiological study of vertical transmission of vaginal Lactobacillus species from mothers to newborn infants in Japanese, by arbitrarily primed polymerase chain reaction. J Infect Chemother. 2002. 8:43–49.

13. Martín R, Langa S, Reviriego C, Jimínez E, Marín ML, Xaus J, et al. Human milk is a source of lactic acid bacteria for the infant gut. J Pediatr. 2003. 143:754–758.

14. Rinne M, Kalliomaki M, Arvilommi H, Salminen S, Isolauri E. Effect of probiotics and breastfeeding on the bifidobacterium and lactobacillus/enterococcus microbiota and humoral immune responses. J Pediatr. 2005. 147:186–191.

15. Hall MA, Cole CB, Smith SL, Fuller R, Rolles CJ. Factors influencing the presence of faecal lactobacilli in early infancy. Arch Dis Child. 1990. 65:185–188.

16. Sanz Y. Gut microbiota and probiotics in maternal and infant health. Am J Clin Nutr. 2011. 94:6 Suppl. 2000S–2005S.

17. Morelli L, Zonenenschain D, Del Piano M, Cognein P. Utilization of the intestinal tract as a delivery system for urogenital probiotics. J Clin Gastroenterol. 2004. 38:6 Suppl. S107–S110.

18. Lee JW, Shim YH, Lee SJ. Lactobacillus colonization status in infants with urinary tract infection. Pediatr Nephrol. 2009. 24:135–139.

19. Bruce AW, Chadwick P, Hassan A, VanCott GF. Recurrent urethritis in women. Can Med Assoc J. 1973. 108:973–976.
20. Marrie TJ, Swantee CA, Hartlen M. Aerobic and anaerobic urethral flora of healthy females in various physiological age groups and of females with urinary tract infections. J Clin Microbiol. 1980. 11:654–659.

21. Gupta K, Stapleton AE, Hooton TM, Roberts PL, Fennell CL, Stamm WE. Inverse association of H2O2-producing lactobacilli and vaginal Escherichia coli colonization in women with recurrent urinary tract infections. J Infect Dis. 1998. 178:446–450.

22. Kirjavainen PV, Pautler S, Baroja ML, Anukam K, Crowley K, Carter K, et al. Abnormal immunological profile and vaginal microbiota in women prone to urinary tract infections. Clin Vaccine Immunol. 2009. 16:29–36.

23. Velraeds MM, van der Mei HC, Reid G, Busscher HJ. Inhibition of initial adhesion of uropathogenic Enterococcus faecalis by biosurfactants from Lactobacillus isolates. Appl Environ Microbiol. 1996. 62:1958–1963.

24. Zárate G, Nader-Macias ME. Influence of probiotic vaginal lactobacilli on in vitro adhesion of urogenital pathogens to vaginal epithelial cells. Lett Appl Microbiol. 2006. 43:174–180.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download