Abstract
Purpose
The purpose of this study was to evaluate whether neo-adjuvant hormonal therapy (NHT) prior to radical retropubic prostatectomy (RRP) for prostate cancer (PCa) is beneficial in terms of surgical outcomes and for preventing or delaying biochemical recurrence via single-surgeon case series study.
Materials and Methods
Fifty-three men underwent RRP by a single surgeon. The patients were divided into two groups according to whether or not NHT was performed prior to RRP. The study was analyzed retrospectively. We evaluated clinical parameters, surgical parameters, and biochemical recurrence rate. Group 1 (n=34) was treated with RRP only, while Group 2 (n=19) underwent RRP along with NHT.
Results
There were no significant differences in clinical, operation-related and pathological factors between the two groups (p>0.05). There was also no significant difference in biochemical recurrence rate between the two groups at the last follow-up, although Group 2 tended to have a lower PCa recurrence rate than Group 1 and the initial prostate-specific antigen (PSA) level was significantly higher in Group 2 than Group 1 (p=0.0496).
Conclusion
The present single-surgeon case series study revealed a trend toward a lower rate of PCa recurrence in NHT+RRP treated patients compared to those treated with RRP alone, but this did not reach statistical significance, despite the fact that NHT+RRP patients exhibited higher serum PSA levels preoperatively. Prospective studies with a longer duration of observation and a greater number of patients would be helpful in evaluating NHT more definitively.
Debate continues regarding the best treatment option for locally limited or locally advanced prostate cancer (PCa). Recently, several risk criteria for PCa prognosis or recurrence were published,1-3 such as Damico's classification, which can be used to make treatment decisions.4 It is considered to be more difficult to control PCa in intermediate or high risk patients with mono-therapy, such as surgery or radiation therapy,5,6 for whom combination of hormonal therapy and surgery is suggested.7-9
The administration of neo-adjuvant or adjuvant hormonal therapy in addition to radical retropubic prostatectomy (RRP) remains controversial.10 To our knowledge, there is no definite methodological standard for administering these hormonal therapies, at least in east Asian countries. Moreover, neo-adjuvant hormonal therapy (NHT) is assumed to entail greater cost,11 and has also been reported to make surgery more difficult because of adhesion or inflammation.12 However, Watson and Soloway12 found pre-surgical NHT to be beneficial for PCa control by suppressing biochemical recurrence. Further studies of this kind are needed to reach a definite consensus or establish guidelines for NHT. Messing, et al.13 likewise reported that immediate androgen deprivation treatment in men with lymph node-positive prostate cancer who have undergone radical prostatectomy (RP) and pelvic lymphadenectomy demonstrated significantly improved overall survival, prostate-cancer-specific survival and progression-free survival compared to the RP-only group. On the other hand, Van Poppel14 reported that adding NHT to RP seemed to have the potential to downstage PCa disease, but did not show a survival benefit over RP alone in patients with localised PCa.
It is well known that PCa varies among different races, and data from western countries are not necessarily applicable to Asian countries.15 The results of NHT studies therefore need to be independently investigated in racially distinct countries or regions to establish the relative value of its clinical application.
In this study, we investigated the efficacy of NHT in RRP via a retrospective study, looking not only at cancer control but at operative results and complications, in a series of cases performed by a single, non-senior surgeon in order to eliminate skill variations among surgeons as a confounding factor.
We retrospectively analyzed the medical records of 53 consecutive PCa patients who were treated with RRP by the Department of Urology, Akashi Municipal Hospital between July 2007 and July 2010. All patients were diagnosed with localized or locally advanced PCa and underwent RRP. All RRPs were performed by a single surgeon with 4 years of urological clinical experience at the initiation of this study. The data were gathered and analyzed retrospectively. The decision to perform NHT was left to the discretion of the physicians in the outpatient department. NHT comprised androgen blockade with a luteinizing hormone-releasing hormone analogue, such as leuprorelin acetate, along with monthly Leuplin® (Takeda Pharmaceutical Co., Ltd., Osaka, Japan) injections and daily administration of an antiandrogen (bicalutamide 80 mg, Casodex®, AstraZeneca K.K., Osaka, Japan) as a rule. RRP included bilateral pelvic lymphadenectomy. All RRPs were performed via a retrograde approach and one patient underwent a unilateral nerve sparing procedure. Autologous blood transfusion was performed as a rule (800 mL) unless severe anemia was noted preoperatively. Urethral catheters were removed postoperatively after confirmation that no urine was leaking by cystography. A total of 34 patients (Group 1, 64.2%) underwent RRP only, and 19 patients (Group 2, 35.8%) were treated with RRP and a median of 3 months of NHT.
We evaluated patients' age, body mass index (BMI), prostate biopsy Gleason score (GS), initial serum prostate-specific antigen (PSA) values, pathological parameters, post-surgical parameters, and biochemical recurrence rate for comparison between the two groups. Surgical parameters included operation time and intraoperative blood loss. Intraoperative blood loss included urine volume after cutting between the prostate and urethra during the surgical procedure. Pathological parameters included margin and capsule status, Gleason scoring and T stage classification of the surgical specimens. Post-surgical parameters included duration of catheterization and surgery-related complications. The median follow-up duration was 33 months.
As follow-up evaluations, we measured serum PSA every 2-3 months for 1 year postoperatively and every 3 months thereafter as a rule. Biochemical recurrence was defined as a serum PSA level of 0.2 ng/mL or greater on the consecutive evaluations.
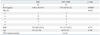
The patients were divided into two groups, administration of NHT before surgery or surgery only. Group 1 (n=34) was treated with RRP only and Group 2 (n=19) underwent RRP along with NHT. Detailed data are shown in Table 1. Although there were no significant differences in age (p=0.746), prostate biopsy (PBx) GS (p=0.6311) and BMI (p=0.713), Group 2 exhibited significantly higher preoperative or pre-NHT PSA values (p=0.0496) (Table 1).
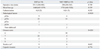
Group 1 and Group 2 showed no significant differences in surgical time (p=0.749), operative blood loss (p=0.339), pathological stage (p=0.9019), margin status (p=0.692), capsule status (p=0.774), surgical specimen GS (p=0.4285), and mean catheterization time (p=0.292) (Table 2). The two groups were also equally balanced for pathologic stage. Pelvic lymph node dissection showed no lymph node metastasis in any of the patients.
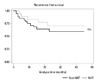
Fig. 1 shows the proportion of men without biochemical recurrence (PSA failure) during the follow-up period among the patients treated by RRP alone and those treated by RRP along with NHT. During the follow-up period, PSA recurrence-free survival tended to be higher for Group 2 (NHT+RRP) than Group 1 (RRP alone), even though this difference was not statistically significant (log-rank test, p=0.3552). The mean biochemical recurrence free period was 18.9±2.47 months in the RRP only group and 25.5±3.28 months in the NHT+RRP group. However, there was no significant difference in positive margin rates (chi-square test, p=0.6922). Some postoperative complications were recorded including one postoperative lymphocele in Group 1. There were no anastomotic strictures or rectovesical fistulas, and there were no mortalities in this series. No patients experienced severe hepatic dysfunction, renal failure, gastrointestinal reactions, or cardiovascular effects.
There are several management options for early or intermediate stage PCa and management should be selected through informed consent with patients based on definite evidence.16,17 Though there are no evidence-based guidelines for the treatment of PCa of these stages that take into consideration differences in PCa characteristics among races,18 there are several PCa risk categorizations, such as Damico's classification, Kattan score or Partin tables,4,19,20 and therapeutic strategies should be selected according to these classifications.
Especially in locally limited or advanced PCa, surgical management plays a major role and there are several surgical procedures available for which to address margin detachment, for instance nerve sparing (unilateral or bilateral), intrafascial, interfascial or extended approaches.21,22 In Japan, RRP is often performed by residents or non-senior surgeons as a common urological surgery;23 therefore, surgeries may not be performed in an established and uniform manner, and may be also changed or modified according to risk criteria.23 This fact could be one reason why it is better to combine surgical management with hormonal therapy.24 However, it remains controversial as to whether neo-adjuvant or adjuvant hormonal therapy (AHT) is better, or how long it should last.25 In Japan, NHT rather than AHT is generally performed with surgery26 and there are several reports as to the efficacy of NHT.25,27 However, not enough evidence has been accumulated for the establishment of guidelines that would be demographically specific to our country. According to Partin nomograms,20 patients with a GS of 6 and PSA >6 ng/mL are considered to involve a greater than 37% possibility of extraprostatic extension, 4% of seminal vesicle invasion, and 1% of lymph node metastasis. Our 19 cases with NHT+RRP based on analyses of prostatectomy specimens included 7 cases with a GS of 6, but 6 out of those 7 cases had PSA >6 ng/mL, suggesting NHT may be helpful in about 40% of these patients. Meanwhile, regarding GS, there are several reports of discrepancy between PBx and prostatectomy samples, as observed in our cases.28
The lack of efficacy studies on NHT can be also attributed to variation among RRPs in regards to the large anatomical variation of not only prostate or peri-prostatic fascia but also of individual patients' pelvic bone shape,29,30 which makes studies more complicated. Our data showed that the NHT group had significantly higher PSA (p=0.0496) than the RRP only group; however, they tended to have a lower PCa recurrence ratio than the RRP only group. Unfortunately, the number of patients and observation duration of the present study after RRP were not large enough to conduct conclusive evaluations and statistical analyses. Though direct comparison requires caution, You, et al.31 demonstrated the efficacy of NHT in high risk PCa and Sumitomo, et al.32 reported the effectiveness of NHT in both high and intermediate risk PCa patients. However, Tanaka, et al.23 found no significant effect for NHT, reflecting the variability of current reports.
Basically, hormonal therapy induces apoptosis and decreases the number of viable PCa cells;33 however, the apoptotic cells can result in atrophic and even fibrotic prostates,34 which could complicate surgery.12 Specifically, inflammation caused by this apoptotic change might make surgical exfoliation of tissues difficult by causing adhesion between the prostate and prostate capsule or prostate capsule and peri-prostatic fascia.35 Regarding the effects of NHT on operative procedures in RRP, Yang, et al.36 stated that a mean of 3 months of NHT led to longer surgical times than those required for the RRP-alone group, while Selli and Milesi25 reported that NHT did not cause any adverse surgical events. Our data did not show that NHT led to increased surgical time or greater intraoperative blood loss. These results could be useful for surgeons, but further large-scale prospective studies are warranted in order to draw more definitive conclusions on NHT.
Though NHT is recognized to inhibit positive margin status,12 some authors have concluded that NHT had no effect on suppressing biochemical recurrence or overall survival.27 The discrepant results may be interpreted as follows: 1) if proliferation of PCa in the marginal portion of the prostate is inhibited by induction of apoptosis via NHT, the surgical margin is likely to be diagnosed as negative; but 2) if even a very small volume of viable PCa cells is located just outside the surgical margin, these could proliferate after surgery and serum PSA may increase afterward.37 Accordingly, we suggest that NHT should be continued until serum PSA level drops below a measurable level prior to surgery to prevent biochemical recurrence. However, it is hard to know whether biochemical recurrence could still occur even if this is done, and the question might be answerable after definitive prospective studies.
We would like to emphasize the limitations of this study. First, the number of patients is too small to draw definitive conclusions. An analysis of power in this population size may be uncertain for statistical significance. Next, the study was of a retrospective nature, and a prospective study with comparable patient backgrounds should be performed. Third, the follow-up duration was not long enough to definitely evaluate PSA recurrence. These issues should be addressed in future prospective study.
In conclusion, this single-surgeon study showed that NHT prior to RRP tended to offer a higher ratio of PSA-free survival than RRP alone, but the difference did not reach statistical significance in the small population size, although the NHT plus RRP patient group had significantly higher serum PSA levels preoperatively and thus were at a potentially higher risk of PCa recurrence. In addition, NHT did not complicate surgical procedures by longer surgical times or extra blood loss. In the future, we plan to perform a prospective study in patients with the same background to further improve risk categorization.
Figures and Tables
Fig. 1
Kaplan-Meier curves for prostate-specific antigen (PSA) recurrence free survival until PSA failure according to treatment regimen Group 1: RRP only (shown as non-NHT) and Group 2: NHT before RRP plus RRP (shown as NHT). Biochemical recurrence rate does not show any significant difference between 2 arms. Log-rank test, p=0.3552. n.s., not significant; NHT, neo-adjuvant hormonal therapy; RRP, radical retropubic prostatectomy.
References
1. Fujikawa K, Sasaki M, Arai Y, Yamabe H, Ogawa O, Yoshida O. Prognostic criteria in patients with prostate cancer: Gleason score versus volume-weighted mean nuclear volume. Clin Cancer Res. 1997. 3:613–618.
2. Chautard D, Cellier P, Dalifard I, Pabot du Chatelard P, Chaussis F, Vielle B, et al. [Biochemical monitoring of prostate cancer treated exclusively by radiotherapy: prognostic value of pretreatment PSA, PSA nadir and PSA half-life]. Prog Urol. 2002. 12:421–428.
3. Kawamorita N, Saito S, Ishidoya S, Ito A, Saito H, Kato M, et al. Radical prostatectomy for high-risk prostate cancer: biochemical outcome. Int J Urol. 2009. 16:733–738.

4. D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998. 280:969–974.
5. Quaranta BP, Marks LB, Anscher MS. Comparing radical prostatectomy and brachytherapy for localized prostate cancer. Oncology (Williston Park). 2004. 18:1289–1302.
6. Maluta S, Dall'oglio S, Nadalini L. Treatment for intermediate and high-risk prostate cancer: controversial issues and the role of hyperthermia. Int J Hyperthermia. 2010. 26:765–774.

7. Milecki P, Kwias Z, Martenka DJ. Radiotherapy combined with hormonal therapy (RT-HT) in prostate cancer patients with low, intermediate, and high risk of biochemical recurrence: perspective and therapeutic gain analysis. Neoplasma. 2007. 54:7–15.
8. Ide H, Nakashima J, Kono H, Kikuchi E, Nagata H, Miyajima A, et al. Prognostic stratification in patients who received hormonal therapy for prostate-specific antigen recurrence after radical prostatectomy. Jpn J Clin Oncol. 2010. 40:177–180.

9. Mendenhall WM, Henderson RH, Hoppe BS, Nichols RC, Mendenhall NP. Androgen Deprivation Therapy and Definitive Radiotherapy for Prostate Cancer. Am J Clin Oncol. 2011. [Epub ahead of print].

10. Kumar S, Shelley M, Harrison C, Coles B, Wilt TJ, Mason MD. Neo-adjuvant and adjuvant hormone therapy for localised and locally advanced prostate cancer. Cochrane Database Syst Rev. 2006. CD006019.

11. Konski A, Watkins-Bruner D, Brereton H, Feigenberg S, Hanks G. Long-term hormone therapy and radiation is cost-effective for patients with locally advanced prostate carcinoma. Cancer. 2006. 106:51–57.

12. Watson R, Soloway MS. Is there a role for induction androgen deprivation prior to radical prostatectomy? Hematol Oncol Clin North Am. 1996. 10:627–641.

13. Messing EM, Manola J, Yao J, Kiernan M, Crawford D, Wilding G, et al. Immediate versus deferred androgen deprivation treatment in patients with node-positive prostate cancer after radical prostatectomy and pelvic lymphadenectomy. Lancet Oncol. 2006. 7:472–479.

14. Van Poppel H. Neoadjuvant and adjuvant hormone therapy: how and when? Eur Urol Suppl. 2008. 7:747–751.

15. Peters N, Armstrong K. Racial differences in prostate cancer treatment outcomes: a systematic review. Cancer Nurs. 2005. 28:108–118.
16. Jani AB, Hellman S. Early prostate cancer: clinical decision-making. Lancet. 2003. 361:1045–1053.

17. Marusić G, Vojinov S, Levakov I. [Treatment of locally advanced prostatic cancer]. Med Pregl. 2010. 63:689–695.

18. Abraham N, Wan F, Montagnet C, Wong YN, Armstrong K. Decrease in racial disparities in the staging evaluation for prostate cancer after publication of staging guidelines. J Urol. 2007. 178:82–87.

19. Kattan MW, Zelefsky MJ, Kupelian PA, Scardino PT, Fuks Z, Leibel SA. Pretreatment nomogram for predicting the outcome of three-dimensional conformal radiotherapy in prostate cancer. J Clin Oncol. 2000. 18:3352–3359.

20. Partin AW, Mangold LA, Lamm DM, Walsh PC, Epstein JI, Pearson JD. Contemporary update of prostate cancer staging nomograms (Partin Tables) for the new millennium. Urology. 2001. 58:843–848.

21. Lawrentschuk N, Trottier G, Kuk C, Zlotta AR. Role of surgery in high-risk localized prostate cancer. Curr Oncol. 2010. 17:Suppl 2. S25–S32.

22. Neill MG, Louie-Johnsun M, Chabert C, Eden C. Does intrafascial dissection during nerve-sparing laparoscopic radical prostatectomy compromise cancer control? BJU Int. 2009. 104:1730–1733.

23. Tanaka N, Fujimoto K, Hirayama A, Torimoto K, Okajima E, Tanaka M, et al. Risk-stratified survival rates and predictors of biochemical recurrence after radical prostatectomy in a Nara, Japan, cohort study. Int J Clin Oncol. 2011. 16:553–559.

24. Spahn M, Weiss C, Bader P, Ströbel P, Gerharz EW, Kneitz B, et al. Long-term outcome of patients with high-risk prostate cancer following radical prostatectomy and stage-dependent adjuvant androgen deprivation. Urol Int. 2010. 84:164–173.

25. Selli C, Milesi C. Neoadjuvant androgen deprivation before radical prostatectomy. A review. Minerva Urol Nefrol. 2004. 56:165–171.
26. Hachiya T, Akakura K, Saito S, Shinohara N, Sato K, Harada M, et al. A retrospective study of the treatment of locally advanced prostate cancer by six institutions in eastern and north-eastern Japan. BJU Int. 2005. 95:534–540.

27. Shelley MD, Kumar S, Wilt T, Staffurth J, Coles B, Mason MD. A systematic review and meta-analysis of randomised trials of neo-adjuvant hormone therapy for localised and locally advanced prostate carcinoma. Cancer Treat Rev. 2009. 35:9–17.

28. Divrik RT, Eroglu A, Sahin A, Zorlu F, Ozen H. Increasing the number of biopsies increases the concordance of Gleason scores of needle biopsies and prostatectomy specimens. Urol Oncol. 2007. 25:376–382.

29. Matikainen MP, von Bodman CJ, Secin FP, Yunis LH, Vora K, Guillonneau B, et al. The depth of the prostatic apex is an independent predictor of positive apical margins at radical prostatectomy. BJU Int. 2010. 106:622–626.

30. Mason BM, Hakimi AA, Faleck D, Chernyak V, Rozenblitt A, Ghavamian R. The role of preoperative endo-rectal coil magnetic resonance imaging in predicting surgical difficulty for robotic prostatectomy. Urology. 2010. 76:1130–1135.

31. You D, Jeong IG, Kim CS. Role of radical prostatectomy for high-risk prostate cancer. Korean J Urol. 2010. 51:589–595.

32. Sumitomo M, Hayashi M, Watanabe T, Tsugawa M, Noma H, Yamaguchi A, et al. Efficacy of short-term androgen deprivation with high-intensity focused ultrasound in the treatment of prostate cancer in Japan. Urology. 2008. 72:1335–1340.

33. Petraki CD, Sfikas CP. Histopathological changes induced by therapies in the benign prostate and prostate adenocarcinoma. Histol Histopathol. 2007. 22:107–118.
34. Polito M, Muzzonigro G, Minardi D, Montironi R. Effects of neoadjuvant androgen deprivation therapy on prostatic cancer. Eur Urol. 1996. 30:Suppl 1. 26–31.

35. Maldonado-Valadez R, Teber D, Erdogru T, Safi KC, Frede T, Rassweiler J. The impact of neoadjuvant hormonal therapy on the outcome of laparoscopic radical prostatectomy: a matched pair analysis. J Urol. 2006. 175:2092–2096.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download