Abstract
Purpose
Continuous cardiac monitoring in a stroke unit (SU) may improve detection of atrial fibrillation (AF), and SU care may improve the rate of anticoagulation by better adherence to a standardized treatment protocol in patients with AF. We investigated the effects of the SU on the detection of AF and the rate of warfarin therapy in patients with AF.
Materials and Methods
Acute stroke patients who had been admitted before or after the opening of the SU were included in our study. SU patients were monitored continuously with electrocardiography. Rates of AF and warfarin therapy were compared between patients admitted to the SU (SU group) and those admitted to the general ward (GW) prior to the opening of the SU (GW group).
Results
Total 951 patients had been admitted to the GW prior to the opening of the SU (from January 2000 to November 2002), and 2349 patients to the SU (from January 2003 to December 2008). AF was found in 149 patients (15.7%) in the GW group and in 487 (20.7%) in the SU group. Most of AF detected during admission was paroxysmal AF (84.8%). The frequency of newly detected AF was higher in the SU group than the GW group (2.5% vs. 0.7%, p=0.001). The rate of anticoagulation consideration was also higher in the SU group.
Organized stroke care in a stroke unit (SU) constitutes a standardized protocol for acute evaluation and management by a coordinated, multidisciplinary stroke team.1 The essential part of the intensive SU model includes monitoring of physical and neurological status,2 and care in the SU is known to improve the outcome of stroke patients.3 However, there are several issues that are not clearly resolved yet. First, it is still unknown why care in the SU improves the outcomes of stroke patients.4 Second, there are controversies regarding the necessity of continuous cardiac monitoring in the SU.5,6
Stroke patients with atrial fibrillation (AF) have a higher stroke recurrence rate than those without AF. This is assumed to be due to a high embolic risk, a low detection rate of paroxysmal AF, and/or inadequate anticoagulation with vitamin-K antagonists.7 Continuous cardiac monitoring in the SU may increase the detection of AF. In addition, better use of a standardized protocol and quality improvement activities in the SU may improve the rate of anticoagulation therapy in patients with AF. The aim of this study was to investigate the effects of SU on the detection of AF that had not been recognized at admission and on the use of warfarin therapy in patients with AF.
We included acute cerebral infarction or transient ischemic attack (TIA) who had been admitted to the neurology department within 7 days after symptoms onset. Data were analyzed retrospectively using a stroke registry and medical records. This study was approved by the Institutional Review Board of Severance Hospital, Yonsei University Health System.
Admission to the SU required adherence with the written admission criteria,8 including stroke within three days after symptom onset, recurrent TIA, thrombolytic treatment, progressive stroke, impending brain herniation, and scheduled or performed cerebral digital subtraction angiography or cerebral artery angioplasty/stent. Among them, patients with acute cerebral infarction or TIA who had been admitted within 7 days after symptoms onset were included.
In all SU patients, electrocardiography (ECG), pulse rate, respiration rate, and oxygen saturation were continuously monitored. Blood pressure and body temperature were monitored on an hourly basis. Patient neurological status was monitored using the National Institute of Health Stroke Scale (NIHSS). After stabilization of neurological symptoms, the patients were transferred to the general ward (GW) or discharged according to the predetermined discharge criteria of the SU.8
All patients took standard 12-lead ECG at admission. The patient's previous history of AF and results of the standard 12-lead ECG at admission were reviewed. During the SU stay, a standard 12-lead ECG was performed immediately when AF was suspected based on ECG monitoring by continuous inspection of trained nurses or physicians. In the GW, follow-up standard ECG was also performed when arrhythmia was detected or suspected during admission. AF was classified as paroxysmal if episodes terminated spontaneously in less than seven days. All other types of AF were classified as persistent/permanent.
The treatment protocol was the same both before and after the opening of the SU. The standard treatment protocol in acute ischemic stroke patients with AF includes oral anticoagulation. Therefore, all patients with AF who were enrolled in our study should have been treated with warfarin, except patients with contraindications for anticoagulation. Whether the patient was prescribed warfarin at discharge was reviewed. If the medical records illustrated reasons of why the patient should not receive anticoagulants, the patient was regarded as being considered for anticoagulation. We investigated both rates for anticoagulation rate and anticoagulation consideration.
The frequencies of AF which were documented at admission and during hospitalization were compared between patients admitted to the SU (SU group) and those admitted to the GW prior to the opening of the SU (GW group). The anticoagulation rates of AF were also compared between the SU and GW groups. The SPSS for Windows (version 18.0, SPSS Inc., Chicago, IL, USA) was used for statistical analyses. The independent samples t-test and the Pearson χ2 test were used for comparisons between the GW group and the SU group. Significance was set at p<0.05.
Prior to the opening of the SU (from January 2000 to November 2002), 951 patients with acute cerebral infarction or TIA were admitted to the neurology department, within 7 days after symptom onset. After the opening of the SU (from January 2003 to December 2008), 3016 acute stroke patients were admitted within 7 days after symptoms onset. Of these 3016 patients, 2349 (77.9%) stayed in the SU during their hospitalization. The remaining patients were not admitted to the SU due to unavailability of bed in the SU or presentation to the hospital later than 3 days after symptom onset. The mean duration of hospitalization was 10.4±9.0 days in the GW group, and 9.6±9.3 days in the SU group (stayed for 4.9±2.5 days in the SU). There was no significant difference in the duration of hospitalization between the GW group and SU group (p=0.073).
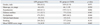
Hypertension was more common in the SU group than in the GW group. Dyslipidemia was more common and the baseline NIHSS score was higher in the GW group than in the SU group. The remaining demographics, including classic risk factors for stroke, were not different between the groups (Table 1).
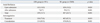
AF was observed in 149 patients (15.7%) in the GW group and in 487 patients (20.7%) in the SU group (p=0.001). The frequency of AF documented at admission was higher in the SU group than in the GW group (Table 2). AF was newly detected during hospitalization in 7 patients (0.7%) in the GW group and in 59 patients in the SU group (2.5%, p=0.001) (Table 2).
Most AF detected during admission was paroxysmal AF (56 of 66 newly detected AF, 84.8%), and there was no difference in the types of AF between the two groups [paroxysmal AF, 7 of 7 in the GW group (100%) vs. 49 of 59 in the SU group (83.1%)] (p=0.583).
The rate of warfarin therapy was higher in the SU group (82.5%) than in the GW group (73.8%) (p=0.019). The rate of consideration for anticoagulation was also higher in the SU group than in the GW group (Table 2). The most common reason that stroke survivors did not receive anticoagulation treatment despite consideration was intracerebral hemorrhage and large hemorrhagic transformation (Table 3).
The benefit of SU care is well-known, and the effects are long-lasting.9 However, the precise reason of why SU care improves patient outcome is not yet clear.4 In this study, detection of AF and the rate of anticoagulation in stroke patients with AF increased after the opening of the SU, contributing to improved long-term outcome due to better prevention of recurrent strokes.
Although the SU care is one treatment supported by the highest level of evidence, models are not uniform among hospitals and countries. Common stroke-model components include multidisciplinary team care, evidence-based management protocol and early rehabilitation.10 However, controversies exist regarding the necessity of continuous monitoring of vital signs, including ECG.2,5,8 Our findings suggest that continuous ECG monitoring in SU is helpful for improved detection of AF.
Although current clinical guidelines recommend anticoagulation therapy as a standard preventive strategy for secondary prevention in stroke patients with AF, compliance with such guidelines is reportedly not satisfactory.7,11,12 In the present study, anticoagulation rate was higher in the SU group than the GW group, despite of same treatment protocol between the two groups. The increased rate of anticoagulation consideration in the SU group suggested that care in SUs improved compliance with treatment protocols, which supports the usefulness of SU care.
In our study, about 85% of newly detected AF was the paroxysmal type. Anticoagulation is required for patients with paroxysmal AF as well as those with persistent or permanent AF, because the incidences of ischemic stroke are similar between those types of AF.13 Although AF is easily diagnosed using routine ECG at admission, paroxysmal AF may not appear on an isolated ECG recording.14 Almost 30% of newly detected AF cases were reported as paroxysmal AF in patients with acute ischemic stroke.15 Detection of a paroxysmal AF may improve as the duration of ECG monitoring increases.16 ECG recording for 24 hours increases the detection of previously unrecognized AF in up to 2% of stroke patients.17 Our findings demonstrated that the increased frequency of AF during ECG monitoring in the SU was due to improved detection of paroxysmal AF. Although Holter monitoring for 24 hours or for a few days may be performed in stroke patients who are not admitted to the SU but in the GW, routine implementation of those evaluation in stroke patients in the GW is not easy in clinical practice. In this regard, continuous ECG monitoring in the SU during acute stage of infarction is more practical. Continuous ECG monitoring in the SU may have additional benefits of real time detection of other cardiac disease, including acute myocardial infarction as well as AF.
There are several limitations in this study. First, we did not use automatic system to detect paroxysmal AF in SU. If automatic detect system was available, detection rate of AF might be higher than that in this study. Second, the SU group included about 78% of acute stroke patients who were admitted during the study period while the GW group included all acute stroke patients. Some of patients who were not admitted to the SU were due to presentation to a hospital later than 3 days after symptom onset. This might affect the results of comparison between the groups, although it might be a little. Third, hypertension was more common in the SU group. The higher frequency of AF upon admission in the SU group may partly be due to the higher frequency of hypertension in this group. Nevertheless, our findings demonstrated that detection of AF and the rate of anticoagulant use in stroke patients with AF increased after the opening of a SU. Stroke-unit care may contribute to improved long-term outcomes due to better prevention of recurrent stroke in patients with AF. Our findings support the benefit of continuous cardiac monitoring in the SU.
Figures and Tables
ACKNOWLEDGEMENTS
The authors would like to thank our biostatistician, Hye Sun Lee, M.S., for her assistance in our statistical analyses.This work was supported by a grant from the Korea Health 21 R&D Project, Ministry of Health & Welfare, Republic of Korea (A102065).
References
1. Stroke Unit Trialists' Collaboration. Organised inpatient (stroke unit) care for stroke. Cochrane Database Syst Rev. 2007. CD000197.
2. Treib J, Grauer MT, Woessner R, Morgenthaler M. Treatment of stroke on an intensive stroke unit: a novel concept. Intensive Care Med. 2000. 26:1598–1611.

3. Rudd AG, Hoffman A, Irwin P, Lowe D, Pearson MG. Stroke unit care and outcome: results from the 2001 National Sentinel Audit of Stroke (England, Wales, and Northern Ireland). Stroke. 2005. 36:103–106.
6. Steiner T. Stroke unit design: intensive monitoring should be a routine procedure. Stroke. 2004. 35:1018–1019.

7. Waldo AL, Becker RC, Tapson VF, Colgan KJ. NABOR Steering Committee. Hospitalized patients with atrial fibrillation and a high risk of stroke are not being provided with adequate anticoagulation. J Am Coll Cardiol. 2005. 46:1729–1736.

8. Choi HY, Cho HJ, Kim SH, Han SW, Nam HS, Lee JY, et al. Organization and operation of stroke unit. Korean J Stroke. 2006. 8:171–178.
9. Fuentes B, Díez-Tejedor E, Ortega-Casarrubios MA, Martínez P, Lara M, Frank A. Consistency of the benefits of stroke units over years of operation: an 8-year effectiveness analysis. Cerebrovasc Dis. 2006. 21:173–179.

10. Kwan J, Hand P, Dennis M, Sandercock P. Effects of introducing an integrated care pathway in an acute stroke unit. Age Ageing. 2004. 33:362–367.

11. McBride D, Brüggenjürgen B, Roll S, Willich SN. Anticoagulation treatment for the reduction of stroke in atrial fibrillation: a cohort study to examine the gap between guidelines and routine medical practice. J Thromb Thrombolysis. 2007. 24:65–72.

12. Glazer NL, Dublin S, Smith NL, French B, Jackson LA, Hrachovec JB, et al. Newly detected atrial fibrillation and compliance with antithrombotic guidelines. Arch Intern Med. 2007. 167:246–252.

13. Friberg L, Hammar N, Rosenqvist M. Stroke in paroxysmal atrial fibrillation: report from the Stockholm Cohort of Atrial Fibrillation. Eur Heart J. 2010. 31:967–975.

14. Liao J, Khalid Z, Scallan C, Morillo C, O'Donnell M. Noninvasive cardiac monitoring for detecting paroxysmal atrial fibrillation or flutter after acute ischemic stroke: a systematic review. Stroke. 2007. 38:2935–2940.

15. Lin HJ, Wolf PA, Benjamin EJ, Belanger AJ, D'Agostino RB. Newly diagnosed atrial fibrillation and acute stroke. The Framingham Study. Stroke. 1995. 26:1527–1530.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download