Abstract
Purpose
To verify the effect of a newly-developed cylindrical type forearm brace, which was designed to give focal counterforce perpendicularly on the muscle belly of the wrist extensor.
Materials and Methods
The dominant hands of 24 (12 males, 12 females) healthy subjects were tested. Two types of forearm braces (focal cylindrical type and broad pneumatic type) were examined. The braces were applied at the extensor carpi radialis brevis, 5 to 7 cm distal to the lateral epicondyle. Two surface electrodes were attached to the proximal and distal parts of the brace. By quantitative electromyography, the mean amplitudes of voluntary extensor carpi radialis brevis contraction before and after applying each brace were recorded and analyzed.
Results
The mean amplitudes of the focal cylindrical brace and broad pneumatic brace were reduced significantly compared to no brace (p<0.05), with a larger reduction for the cylindrical brace than the pneumatic brace (p<0.05). There was no significant difference between the proximal and distal mean amplitudes with each brace.
Lateral epicondylitis, or tennis elbow, causes pain at the origin of the wrist extensor muscle through overuse, not only in racquet sports players but also in individuals who perform repeated wrist extension and prehension activities.1,2 There are many studies of the pathophysiology of lateral epicondylitis, and it was recently established that pain occurs due to a failure of the reparative process after repeated microtrauma-induced tendon injury rather than due to active inflammation.3-5 The absence of inflammatory cells in the wrist extensor tendon tissue of patients with lateral epicondylitis has been described by several other studies.6,7
The symptoms of lateral epicondylitis can improve after 8 to 12 months without specific treatment. However, several conservative treatment methods, including physical modalities (ultrasound, iontophoresis, etc.), friction massage, strengthening exercise, forearm brace, corticosteroid or botulinum injection, and extracorporeal shock wave therapy have been applied and their effectiveness proven.8-11 Surgical treatment, such as releasing or lengthening of the extensor origin, debridement of the extensor origin and decompression can be considered in the case of failure of conservative treatment. Conservative treatment has been improved in terms of its effect, but involves controversy regarding its durability. The short-term effects of steroid injection have been improved, but show a high recurrence rate. Sölveborn, et al.12 reported that most patients suffering lateral epicondylitis experience a recurrence of symptoms after steroid injection within three months. Price, et al.13 reported a 50% recurrence rate. Recently, combination therapy involving resting, exercise, and a forearm brace has been preferred for basic treatment of lateral epicondylitis. A forearm brace is applied to the proximal part of the muscle belly of the wrist extensor, and makes a pseudo-origin on the wrist extensor by exerting counterforce. This pseudo-origin reduces tensile stress at the region of the teno-osseous junction, which helps patients to extend their wrist or grasp their hand without pain.
Stonecipher and Catlin14 stated that subjects would have better grip strength when wearing a counterforce brace because of the increased cutaneous sensory stimulation by the brace to the underlying muscles. Wadsworth, et al.15 supported this theory and found a significant increase in wrist extension strength in subjects with tennis elbow after applying the brace. However, Anderson and Rutt16 reported that the forearm muscle strength would decrease when wearing a forearm counterforce brace because compression of the counterforce brace over the musculotendinous unit would restrict the expansion of the muscles, thus impeding on the tendon movement and force production capacity. Common types of current forearm braces create counterforce by applying compression to the broad area of the writer extensor muscle belly. Many braces of this type have been shown to be less effective when applied to patients.17,18 We suspected that existing braces could not reduce tensile stress at the proximal part of the brace because of inappropriate counterforce on the muscle belly. We therefore made a new cylindrical type of forearm brace that can produce intensive counterforce perpendicularly to the focal area of muscle belly.
This study aimed to verify the effect of this new cylindrical type brace compared to existing braces by measuring quantitative electromyographic activity on the muscle belly at before and after applying the braces.
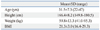
The study cohort consisted of 24 healthy people (12 males, 12 females) with a mean age of 31.5±7.3, a mean height of 166.4±8.2 cm, and weight of 59.8±13.3 kg (Table 1). All subjects' were right handed. Subjects who had disease or surgery history in their upper extremities and those with weakness or pain around the elbow were excluded. All participants received a satisfactory explanation of the study's object and methods. This study was initiated after receiving approval from the Institutional Review Board at our hospital.
Two types of forearm braces were applied to subjects: 1) an existing pneumatic type white-colored armband brace that produces counterforce with a 4 cm wide and 5 cm long aircast, and 2) a new type black-colored armband brace with a 1 cm diameter and 5 cm long cylindrical hard-rubber (Fig. 1). Both braces can be applied by velcro but rubber of the cylindrical brace contacts with narrow part of the forearm, while aircast of pneumatic brace contacts widely. The muscle activity of the wrist extensor was measured three times: before applying the brace, and after applying each brace. The commercially available quantitative electromyographic (qEMG) device Datalog® (Biometrics Ltd., Gwent, UK) was used to measure muscle activity. This device has an analogue-digital converter with 110 dB of common-mode rejection ratio, and a band pass filter of 10-1000 Hz. The raw EMG signal was rectified and smoothed using a root mean square (RMS) procedure. The mean amplitude (µV) of the RMS EMG signal was used to quantify the level of EMG activity during the contraction of the wrist extensor. The subject applied the brace on the proximal edge, measured at 5 to 7 cm distal to the lateral epicondyle, thus producing pressure to the muscle belly of the extensor carpi radialis brevis (ECRB). EMG activity was recorded for the ECRB of the dominant side by surface electrode. Two surface electrodes were attached to the distal and proximal parts of the brace-applied area on the ECRB. The examiner determined the location of the ECRB manually by palpation and manual muscle testing. The ground reference was attached to wrist of the non-dominant side using a wrist band. Each subject performed three measurements from no brace to applying cylindrical brace. The degree of compression by brace was submaximal amount not to make a discomfort to subject. To minimize the bias, subjects recorded degrees of pain produced by applying first brace with graded pain scale and applied next brace at same degree of graded pain scale. The starting position was standardized, with subjects sitting on a chair and the tested arm supported by the desk, with the elbow in 30 to 40 degree extension, forearm in pronation, and grasping the 3 kg dumbbell. Then EMG activity was recorded while the subject was lifting the dumbbell for four seconds by extending the wrist to the full range of motion (Fig. 2). The subject lifted the dumbbell four times in each measurement at 10 second intervals and we recorded the mean EMG activity from these four times. The resting time between each measurement was three minutes.
SPSS software (version 15.0.0, SPSS Inc., Chicago, IL, USA) was used for all analyses. Differences in EMG activity of the proximal and distal parts of the ECRB between the without brace condition and with each brace were analyzed using Wilcoxon's signed ranks test. Differences in the degree (%) of EMG activity reduction between each brace, and between the proximal and distal part from the brace area, were also analyzed using Wilcoxon's signed ranks test. Statistical significance was assumed to be at p<0.05.
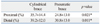
Mean amplitudes of RMS EMG signal of EMG activity levels with the cylindrical brace were 0.196±0.07 at proximal and 0.177±0.06 at distal, and with the pneumatic brace were 0.231±0.08 at proximal and 0.201±0.06 at distal. Mean amplitudes of RMS EMG signal without the forearm brace (0.316±0.12 at proximal, 0.293±0.09 at distal) were significantly larger than those with either brace (p<0.05) (Table 2).
Although both braces significantly decreased the EMG activities at ECRB, the degrees of reduction were different. The mean percentage of reduction in EMG activity after applying the cylindrical brace (35.7±14.4% at proximal, 39.2±12.0% at distal) was significantly larger than with the pneumatic brace (24.8±13.0% at proximal, 30.8±13.0% at distal, p<0.05) (Table 3). There was no significant difference in degree of EMG reduction between proximal area and distal area with both braces.
Lateral epicondylitis can be classified into four types: tenoperiosteal, muscular, tendinous, and supracondylar. The tenoperiosteal type is most common at the ECRB.19 Repetitive degenerative change and recovery of the tenoperiosteal type may cause weakness and rupture of the common wrist extensor origin. Degenerative change in a tendon typically involves degeneration of collagen fiber, fibroblastic proliferation of vessels, mixoid and hyaline degeneration, and is classified as tendinosis rather than tendonitis.
There are more than 40 methods for treatment of lateral epicondylitis. Studies of surgical treatments have shown acceptable results.20-23 Treatment with a forearm brace is widely used because it does not need large-scale or costly equipment and does not cause side effects, unlike medications or injections, and can be continuously applied at low cost during activities of daily living. There have been several studies into the effect and appropriate application method of the forearm brace. Luginbühl, et al.17 reported that symptoms improved spontaneously as time went by, rather than due to specific action of the forearm brace and strengthening exercise. Ng and Chan24 reported that a forearm brace could increase the pain threshold during passive stretching of the wrist extensor by affecting proprioception of the wrist joint. Some studies have demonstrated that a forearm brace can decrease the pain of patients with lateral epicondylitis through a decrease of tension in the origin of the wrist extensor.25,26
In this study, EMG activity in the proximal and distal areas was significantly reduced after applying both braces compared to initial activities without brace. This may be achieved through the mechanism by which they perform a role in the new origin of ECRB. If the compressed area of the brace performs the role of new origin correctly, EMG activity in the distal area should not be decreased. However, EMG activities in the distal area were decreased with both the cylindrical and pneumatic braces. That suggests the pseudo-origin created by the brace has a limited role at the true teno-osseous junction. The performance of the pseudo-origin might be better as compressing pressure increased, but excessive compression could be uncomfortable and painful when applied for a long period. The main purpose of a forearm brace for lateral epicondylitis is relief of pain around the muscle origin. We evaluated EMG activities to compare the effect of two braces, and found that the reduction of EMG activity was larger with a cylindrical brace than a pneumatic brace. We made a new cylindrical type brace that could more effectively function as a pseudo-origin than existing braces, which are ineffective because their counterforce is diffused to a broadly compressed area. Results showed that the cylindrical type brace decreased tensile force to the muscle origin area more than did the pneumatic type brace. Although the role of pseudo-origin was not appropriate, this new cylindrical type brace decreased proximal EMG activity by attenuating proximal loading with damping and lever effect of counterforce. We think that the counterforce was produced better by focal concentrated compression of cylindrical type brace rather than broadly dispersed compression of pneumatic type brace. Reducing muscle activity of wrist extensor more effectively may be the meaning of reducing pain more effectively because previous studies insisted forearm brace could relieve pain by pseudo-origin and it was supported by verifying reduction of electromyographic activity.14,15,26,27 We thus expect that the cylindrical type brace may be more effective for pain relief when clinically applied. We need to examine actual effect of pain reduction with the cylindrical type brace in patient suffering by lateral epicondylitis.
The limitation of this study is that its subjects were healthy people without lateral epicondylitis. Also, the strength of counterforce was not constant in all subjects because the amount of compression was decided by subjective judgment of the maximal compression until uncomfortable pain began to occur. Further randomized controlled study with a larger number of patients and which uses more objective parameters is needed to properly verify the effect of cylindrical type forearm braces.
EMG activities of the wrist extensor at the proximal and distal areas from a brace-applied location were reduced by both cylindrical and pneumatic type forearm braces. However, the cylindrical type brace decreased the EMG activity of the wrist extensor more effectively than the pneumatic type brace did. Further studies are needed to evaluate clinical effect of the cylindrical brace to patients with lateral epicondylitis.
References
1. Faro F, Wolf JM. Lateral epicondylitis: review and current concepts. J Hand Surg Am. 2007. 32:1271–1279.

2. Jobe FW, Ciccotti MG. Lateral and Medial Epicondylitis of the Elbow. J Am Acad Orthop Surg. 1994. 2:1–8.

3. Regan W, Wold LE, Coonrad R, Morrey BF. Microscopic histopathology of chronic refractory lateral epicondylitis. Am J Sports Med. 1992. 20:746–749.

5. Bales CP, Placzek JD, Malone KJ, Vaupel Z, Arnoczky SP. Microvascular supply of the lateral epicondyle and common extensor origin. J Shoulder Elbow Surg. 2007. 16:497–501.

6. Alfredson H, Ljung BO, Thorsen K, Lorentzon R. In vivo investigation of ECRB tendons with microdialysis technique--no signs of inflammation but high amounts of glutamate in tennis elbow. Acta Orthop Scand. 2000. 71:475–479.

7. Galliani I, Burattini S, Mariani AR, Riccio M, Cassiani G, Falcieri E. Morpho-functional changes in human tendon tissue. Eur J Histochem. 2002. 46:3–12.

8. Kalichman L, Bannuru RR, Severin M, Harvey W. Injection of botulinum toxin for treatment of chronic lateral epicondylitis: systematic review and meta-analysis. Semin Arthritis Rheum. 2011. 40:532–538.

9. Bisset L, Paungmali A, Vicenzino B, Beller E. A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia. Br J Sports Med. 2005. 39:411–422.

10. Meyer NJ, Pennington W, Haines B, Daley R. The effect of the forearm support band on forces at the origin of the extensor carpi radialis brevis: a cadaveric study and review of literature. J Hand Ther. 2002. 15:179–184.

11. Assendelft WJ, Hay EM, Adshead R, Bouter LM. Corticosteroid injections for lateral epicondylitis: a systematic overview. Br J Gen Pract. 1996. 46:209–216.
12. Sölveborn SA, Buch F, Mallmin H, Adalberth G. Cortisone injection with anesthetic additives for radial epicondylalgia (tennis elbow). Clin Orthop Relat Res. 1995. (316):99–105.

13. Price R, Sinclair H, Heinrich I, Gibson T. Local injection treatment of tennis elbow--hydrocortisone, triamcinolone and lignocaine compared. Br J Rheumatol. 1991. 30:39–44.

14. Stonecipher DR, Catlin PA. The effect of a forearm strap on wrist-extensor strength*. J Orthop Sports Phys Ther. 1984. 6:184–189.

15. Wadsworth C, Nielsen DH, Burns LT, Krull JD, Thompson CG. Effect of the counterforce armband on wrist extension and grip strength and pain in subjects with tennis elbow. J Orthop Sports Phys Ther. 1989. 11:192–197.

16. Anderson MA, Rutt RA. The effects of counterforce bracing on forearm and wrist muscle function. J Orthop Sports Phys Ther. 1992. 15:87–91.

17. Luginbühl R, Brunner F, Schneeberger AG. No effect of forearm band and extensor strengthening exercises for the treatment of tennis elbow: a prospective randomised study. Chir Organi Mov. 2008. 91:35–40.

18. Chan HL, Ng GY. Effect of counterforce forearm bracing on wrist extensor muscles performance. Am J Phys Med Rehabil. 2003. 82:290–295.

19. Cyriax JH. The pathology and treatment of tennis elbow. J Bone Joint Surg. 1936. 18:921–940.
20. Verhaar J, Walenkamp G, Kester A, van Mameren H, van der Linden T. Lateral extensor release for tennis elbow. A prospective long-term follow-up study. J Bone Joint Surg Am. 1993. 75:1034–1043.

21. Rayan GM, Coray SA. V-Y slide of the common extensor origin for lateral elbow tendonopathy. J Hand Surg Am. 2001. 26:1138–1145.

22. Das D, Maffulli N. Surgical management of tennis elbow. J Sports Med Phys Fitness. 2002. 42:190–197.
23. Tasto JP, Cummings J, Medlock V, Hardesty R, Amiel D. Microtenotomy using a radiofrequency probe to treat lateral epicondylitis. Arthroscopy. 2005. 21:851–860.

24. Ng GY, Chan HL. The immediate effects of tension of counterforce forearm brace on neuromuscular performance of wrist extensor muscles in subjects with lateral humeral epicondylosis. J Orthop Sports Phys Ther. 2004. 34:72–78.

25. Groppel JL, Nirschl RP. A mechanical and electromyographical analysis of the effects of various joint counterforce braces on the tennis player. Am J Sports Med. 1986. 14:195–200.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download