Abstract
Purpose
Imaging features and clinical characteristics of degenerated leiomyoma in patients referred for uterine fibroid embolization (UFE) were analyzed to assess the incidence of degenerated leiomyoma.
Materials and Methods
Patients referred for UFE between 2008 and 2009 were retrospectively analyzed (n=276). Patients ranged in age from 27 to 51 years (mean 38.0 years). All patients underwent screening MRI with contrast enhancement. Medical histories and clinical symptoms were evaluated.
Results
Among the 276 patients who underwent MRI, 14 (5.1%) showed degenerated leiomyomas. Symptoms were abdominal pain (n=4, 26.7%), menorrhagia (n=5, 35.7%) and bulk-related symptoms (n=5, 35.7%) and no symptoms (n=5, 35.7%). Of the 14 patients with degenerated leiomyomas, 5 (42.9%) had a history of pregnancy in the past two years. For T1-weighted imaging (T1WI), a high signal intensity (SI) of the leiomyoma was the most common finding (n=9, 64.3%) and a hyperintense rim (n=4, 28.6%) was the second most common. On T2-weighted imaging (T2WI), a low SI of the leiomyoma was found in six patients (42.9%), a high SI in four (28.6%) and a heterogeneous SI in four (28.6%) patients. Conservative management was performed in 11 (78.6%) patients, surgery in 3 (21.4%) and uterine artery embolization in one (7.1%) patient.
Conclusion
The incidence of degeneration of leiomyoma in patients referred for UFE was 5.1%. Patients presented with variable clinical symptoms with or without a history of pregnancy. MR imaging showed a high SI on T1WI and various SIs on T2WI without contrast enhancement. An understanding of the degeneration of leiomyomata is essential when considering UFE.
Uterine leiomyomas, the most common solid tumor of the female genital tract, develops in 20-40% of women during their reproductive years.1 Degeneration of leiomyoma occurs secondary to a loss of blood supply and is usually attributable to rapid growth associated with pregnancy. It can cause severe pain not relieved by sedation as well as fever or leukocytosis. Degeneration of a leiomyoma is treated pain medication or surgical intervention. Uterine fibroid embolization (UFE) was established as an alternative to a hysterectomy for the treatment of symptomatic leiomyomas.2-5 However, patients with degenerated leiomyoma are more likely to have a poor response to UFE, and it is often difficult to differentiate symptoms and ultrasonographic findings in patients with degenerated leiomyoma from those in patients with non-degenerated leiomyomas.6,7 Therefore, being aware of any existing degenerated leiomyoma before performing UFE is mandatory. The aim of this study was to assess the incidence, imaging features and clinical characteristics of degenerated leiomyoma in patients who were referred for UFE.
The Institutional Review Board at Severance Hospital of Yonsei University approved this study. A retrospective analysis of 276 patients referred for UFE between 2008 and 2009 was performed. All patients underwent transvaginal or transabdominal ultrasound and uterine leiomyomas were primarily diagnosed by gynecologists. Patients ranged in age from 27 to 51 years (mean 38.0 years). The mean follow-up period was 9.7 months (range: 5-16 months).
All patients underwent a preoperative MRI (1.5-T Signa HD/HDx; GE Healthcare, Waukesha, WI, USA) of the pelvis. Axial and sagittal fast spin echo T2-weighted imaging (T2WI; TR/effective TE, 4400/120; matrix size, 384×224; field of view, 300×300 mm; section thickness, 5 mm) and contrast-enhanced sagittal T1-weighted imaging (T1WI) were performed in all cases. An enhanced MRI (TR/TE, 766/9; flip angle 90°; matrix size, 256×160; field of view, 300×300 mm; section thickness, 5 mm) was performed 2 min after intravenous infusion of the 10 mL gadolinium contrast agent (Dotarem, Guerbet, Villapente, France). Degenerated leiomyoma was defined as a leiomyoma showing inhomogenous signal intensity (SI) on T2WI with irregular, peripheral, minimal or absent enhancement compared with that of myometrium.8
SI was defined as either high, greater than the SI of the normal myometrium; intermediate, equal to the SI of the normal myometrium; or low, less than the SI of the normal myometrium. Imaging features of the degenerated leiomyoma were analyzed.
We evaluated patient information related to medical history and clinical symptoms and signs.
Menorrhagia, dysmenorrhea and bulk-related symptoms such as urinary frequency or sensations of pelvic heaviness, were analyzed. In one patient who needed uterine artery embolization, a coaxial 3-F microcatheter (MicroFerret; Cook, Bloomington, IN, USA) was advanced distally into the uterine artery through the right femoral artery and embolization was performed with 250-355 and 355-500 µm size of non-spherical polyvinyl alcohol particles (Contour; Boston Scientific, Natick, MA, USA).
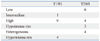
Demographics and clinical characteristics of the patients of the patients are summarized in Table 1.
Among 276 patients who with MRI data, 14 (5.1%) showed degenerated leiomyomas. The size of the degenerated leiomyomas ranged from 5.2 cm to 15.5 cm (mean 7.7 cm). Nine patients had leiomyomas less than 8 cm in size while only three patients had leiomyomas larger than 10 cm.
MR imaging features of the degenerated leiomyomas from all 14 patients are summarized in Table 2. Completely degenerated leiomyomas without any contrast enhancement were noted in 11 patients while a partial viable rim of the degenerated leiomyomas was seen in three patients. On T1WI, a high SI of the leiomyoma was the most common finding (n=9, 64.3%) and a hyperintense rim (n=4, 28.6%) was the second most common. On T2WI, a low SI of the leiomyoma was found in six patients (42.9%), a high SI in four (28.6%) including a hypointense rim in three of those patients. A heterogeneous SI was found in four (28.6%) patients. A follow-up study was performed in five patients by MRI (n=1) or US (n=4). The mean diameter of the leiomyoma decreased from 7.3 cm to 6.7 cm at follow-up. Four (80.0%) out of the five patients showed a decrease in the leiomyoma size (Fig. 1), while no significant interval change in the size of the uterine leiomyoma was noted in the remaining patient.
Symptoms noted were abdominal pain (n=4, 26.7%) including acute onset of pain (n=2), menorrhagia (n=5, 35.7%) and bulk-related symptoms (n=5, 35.7%) such as pelvic heaviness and palpable mass. Five (35.7%) patients had no symptoms. Of the 14 patients with leiomyomas, five (42.9%) had a history of pregnancy in the past two years. Observation with or without conservative management was performed in 10 (71.4%) patients, surgery in three (21.4%) and uterine artery embolization in one (7.1%) patient. Of the three patients who had surgery, two underwent myomectomy and one had a hysterectomy. Those patients had either bulk-related symptoms (n=2) due to a huge leiomyoma, or pain (n=1) for more than a week that was not relieved by analgesics. One patient underwent uterine artery embolization due to heavy bleeding, and the MRI revealed combined adenomyosis as well as the degenerated leiomyoma. For that patient, the three-month follow-up MRI after embolization revealed complete necrosis of the adenomyosis but little interval change in the volume of the degenerated leiomyoma. Symptoms in one patient who had menorrhagia had spontaneously resolved at the six-month follow-up.
The process of leiomyoma degeneration usually begins when the leiomyoma grows so large that the nearby blood vessels can no longer supply it with oxygen and nutrients. Degeneration of the leiomyoma results in a variable and often heterogeneous appearance, with minimal or irregular enhancement. Degeneration is categorized as hyaline, cystic, red or calcific. The most common type of degeneration is hyaline; it accounts for approximately 60% of all degeneration and produces a low SI on T2WI, without contrast enhancement.9,10 Cystic degeneration occurs in approximately 4% of leiomyomas and typically occurs after hyaline degeneration.10
Red degeneration is a hemorrhagic infarction of the uterine leiomyoma, which is a well known complication, especially during pregnancy. Red degeneration occurs in 8% of tumors complicating pregnancy, although the prevalence is about 3% of all uterine leiomyoma.11 Our data indicated that about 42.9% of patients had been pregnant in the previous two years. The mechanism of red degeneration is suggested to begin with venous obstruction at the periphery of the lesion, which induces hemorrhagic infarction and extensive necrosis that involves the entire lesion.
As leiomyoma enlarge, they may outgrow their blood supply, resulting in degeneration, thus degeneration occurs primarily in large leiomyomas. However, our study demonstrated that the majority of patients in whom degeneration was found had leiomyomas less than 8 cm in size; it was even detected in leiomyomas as small as 5.2 cm. One possible explanation seems to come from the widespread use of MRI, which allows an early, precise diagnosis of degenerated leiomyomas.
Pain is the most frequent sign of uterine leiomyoma degeneration. Pain is often severe and localized to the site of the leiomyoma. Severe pain associated with leiomyoma degeneration often lasts for two to four weeks. In addition to pelvic pain, degeneration may cause a low-grade fever and a temporary elevation in the white blood cell count. In some cases, a degenerating uterine leiomyoma may cause menorrhagia, which can also result in a drop in hemoglobin levels. Symptoms of patients with degenerated leiomyomas in our data were abdominal pain including acute onset of pain, menorrhagia, and bulk-related symptoms. These symptoms are similar to those of non-degenerated leiomyomas except acute onset of abdominal pain, which is unusual. A degenerating uterine leiomyoma is often misdiagnosed, frequently being confused with subacute salpingo-oophoritis. A pedunculated subserosal leiomyoma can undergo torsion ischemic necrosis, which is associated with pain similar to that of adnexal torsion.
Degenerating leiomyoma have various nonspecific MRI appearances ranging from medium to high SI on T1WI to a heterogeneous, mostly high SI in the area of degeneration on T2WI.9,12,13 Kawakami, et al.11 reported that red degeneration of uterine leiomyoma had a hyperintense rim on T1WI and a hypointense rim on T2WI. Microscopic examination revealed numerous dilated thrombosed vessels filled with red blood cells at the periphery and these red blood cells in the thrombosed vessels have abundant levels of intracellular methemoglobin, which is known to appear as a hyperintense signal on T1WI and a hypointense signal on T2WI.
The incidence of degeneration of leiomyoma in patients referred for UFE in our study was 5.1%, with the majority of them having undergone conservative treatment. Most patients were initially recommended to undergo surgery after consultation with gynecologists, but these patients wanted a minimally invasive surgery to preserve their uteri. Rest and sedation are recommended in most cases. The pain of red degeneration usually resolves within ten days and supportive treatment is required for this period only. Follow-up ultrasounds or MRIs in our data demonstrated spontaneous reductions in size of the leiomyoma with concurrent improvement of symptoms. Meanwhile, surgery may be needed in some patients with intractable pain. One patient in our study elected to undergo myomectomy for severe pain not controlled with medication, which lasted more than one week. Degenerated leiomyomas are known for their contraindication for UFE due to the likely poor response, as they may already have undergone hemorrhagic necrosis. However, a patient in our study underwent uterine artery embolization for bleeding because of concurrent adenomyosis. The patient's symptoms were significantly improved after embolization, but the volume of the degenerated leiomyoma demonstrated little change.
A limitation of the present study was the relatively small number of patients; therefore, and further studies are needed with larger study populations.
In summary, the incidence of degeneration of leiomyoma in patients referred for UFE was 5.1%. Patients presented with variable clinical symptoms with or without a history of pregnancy. MR imaging showed a high SI on T1WI and various SIs on T2WI without contrast enhancement. The majority of patients can be managed using conservative treatments; however, surgery or uterine artery embolization may be required in some patients. An understanding of the incidence and imaging features and clinical characteristics of the degeneration of leiomyoma is essential when considering UFE.
Figures and Tables
 | Fig. 1A 31-year-old woman who had a normal spontaneous vaginal delivery one year prior. (A) The T1-weighted axial image revealed a 7.0×8.3×6.7 cm leiomyoma (arrows) on the posterior wall of the uterus showing high signal intensity. (B) The T2-weighted sagittal image revealed a heterogenous signal intensity of the leiomyoma. (C) Contrast enhancement was not observed on the gadolinium-enhanced T1-weighted axial image corresponding to B. (D) The follow-up MRI at 18 months demonstrated a 7.4×5.7×6.5 cm leiomyoma, which represents a 29.7% decrease (143 cc from 204 cc) in leiomyoma volume without any treatment. |
References
1. Buttram VC Jr, Reiter RC. Uterine leiomyomata: etiology, symptomatology, and management. Fertil Steril. 1981. 36:433–445.

2. Goodwin SC, McLucas B, Lee M, Chen G, Perrella R, Vedantham S, et al. Uterine artery embolization for the treatment of uterine leiomyomata midterm results. J Vasc Interv Radiol. 1999. 10:1159–1165.

3. Walker WJ, Pelage JP. Uterine artery embolisation for symptomatic fibroids: clinical results in 400 women with imaging follow up. BJOG. 2002. 109:1262–1272.

4. Spies JB, Cooper JM, Worthington-Kirsch R, Lipman JC, Mills BB, Benenati JF. Outcome of uterine embolization and hysterectomy for leiomyomas: results of a multicenter study. Am J Obstet Gynecol. 2004. 191:22–31.

5. Pron G, Bennett J, Common A, Wall J, Asch M, Sniderman K. Ontario Uterine Fibroid Embolization Collaboration Group. The Ontario Uterine Fibroid Embolization Trial. Part 2. Uterine fibroid reduction and symptom relief after uterine artery embolization for fibroids. Fertil Steril. 2003. 79:120–127.

6. Omary RA, Vasireddy S, Chrisman HB, Ryu RK, Pereles FS, Carr JC, et al. The effect of pelvic MR imaging on the diagnosis and treatment of women with presumed symptomatic uterine fibroids. J Vasc Interv Radiol. 2002. 13:1149–1153.

7. Burn PR, McCall JM, Chinn RJ, Vashisht A, Smith JR, Healy JC. Uterine fibroleiomyoma: MR imaging appearances before and after embolization of uterine arteries. Radiology. 2000. 214:729–734.

8. Yamashita Y, Torashima M, Takahashi M, Tanaka N, Katabuchi H, Miyazaki K, et al. Hyperintense uterine leiomyoma at T2-weighted MR imaging: differentiation with dynamic enhanced MR imaging and clinical implications. Radiology. 1993. 189:721–725.

9. Okizuka H, Sugimura K, Takemori M, Obayashi C, Kitao M, Ishida T. MR detection of degenerating uterine leiomyomas. J Comput Assist Tomogr. 1993. 17:760–766.

10. Ueda H, Togashi K, Konishi I, Kataoka ML, Koyama T, Fujiwara T, et al. Unusual appearances of uterine leiomyomas: MR imaging findings and their histopathologic backgrounds. Radiographics. 1999. 19 Spec No:S131–S145.

11. Kawakami S, Togashi K, Konishi I, Kimura I, Fukuoka M, Mori T, et al. Red degeneration of uterine leiomyoma: MR appearance. J Comput Assist Tomogr. 1994. 18:925–928.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download