Abstract
Purpose
The aim of this study was to compare a negative pressure drain with a natural drain in order to determine whether a negative pressure drainage tube causes an increase in the drainage volume.
Materials and Methods
Sixty-two patients who underwent total thyroidectomy for papillary thyroid carcinoma (PTC) were enrolled in the study between March 2010 and August 2010 at Gyeongsang National University Hospital. The patients were prospectively and randomly assigned to two groups, a negative pressure drainage group (n=32) and natural drainage group (n=30). Every 3 hours, the volume of drainage was checked in the two groups until the tube was removed.
Results
The amount of drainage during the first 24 hours postoperatively was 41.68±3.93 mL in the negative drain group and 25.3±2.68 mL in the natural drain group (p<0.001). After 24 additional hours, the negative drain group was 35.19±4.26 mL and natural drain groups 21.53±2.90 mL (p<0.001). However, the drainage at postoperative day 3 was not statistically different between the two groups. In addition, the vocal cord palsy and temporary and permanent hypocalcemia were not different between the two groups.
With an improvement of surgical instruments1 and development of anti-hemorrhagic sprays for surgical areas,2 attempts have been made to avoid the insertion of a drainage tube after a total thyroidectomy. However, concerns about the safety and risks of not inserting a drainage tube have made this a controversial procedure for many years.3-8 In general, there are several advantages to placing a negative suction drain after a thyroidectomy: the dead space that develops after surgery is reduced, repositioning of the flaps is facilitated, and the recovery of the patient is faster.9-11 The insertion of a drainage tube is also recommended since hematomas or seromas may develop after surgery, although the incidence of early hemorrhage is as low as approximately 0.3 to 1.0%.
Another pertinent factor regarding the insertion of a drainage tube is the timing of the removal of a closed suction drain inserted after surgery, which becomes important in determining the hospitalization period. If a drainage tube is not inserted, the hospitalization period could be shortened, and the discomfort of patients due to the insertion and removal of the tube is reduced.12
However, seromas or hematomas could be formed, and aspiration or compression treatments are required in patients when drainage tubes were not inserted. In fact, it has been reported that seromas or hematomas develop in 4 out of 37 patients (10.8%) in whom a drainage tube was not inserted after total thyroidectomy with central neck dissection, and that all of them required aspiration and compression treatment.4 On the other hand, increased scarring and infection due to the drainage tubes themselves have been reported. Thus, the effectiveness of inserting a drainage tube remains controversial.3
With a recent development of several surgical instruments, numerous surgeons have become interested in having no drainage after thyroid surgery. However, studies to date have been limited because the volume that drains spontaneously after surgery could not be predicted. Thus, no drain thyroid surgery has been performed on the basis of personal experience of surgeons.
In this study, we measured drainage volume every 3 hours after surgery in patients who received total thyroidectomy without central neck dissection for papillary thyroid carcinoma in order to assess whether a negative pressure drainage tube increases the drainage volume.
The protocol for this prospective clinical study was approved by the Institutional Review Board (GNUHIRB-2010-023), Gyeongsang National Medical School, Jinju, Korea. A study flowchart is shown in Fig. 1. From May 2009 to August 2010, 149 consecutive patients who visited our outpatient clinic with thyroid papillary carcinoma were enrolled in this study (Fig. 1).
The inclusion criteria were patients older than 20 years of age diagnosed with papillary thyroid carcinoma or suspicious papillary thyroid carcinoma by a preoperative fine needle aspiration test and confirmed by a postoperative pathologic diagnosis. The long axis of papillary thyroid carcinoma had to be shorter than 1 cm measured by ultrasonography, and all the enrolled patients provided written informed consent to enroll in the study.
The exclusion criteria included the presence of any of the following: history of head and neck malignancy, history of radiation therapy in the head and neck area, drugs affecting thyroid function, and thyroiditis detected by presurgical tests that may affect drainage. Of the 149 patients, 87 did not meet the eligibility criteria and were excluded from the study.
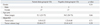
Ultimately, 62 patients who had undergone a total thyroidectomy performed by a single surgeon were included in the study. The patients whose hemostasis procedure in the thyroid resection area was completed were divided into two groups: 32 patients in the natural drainage group and 30 patients in the negative pressure drainage group. Selection was made by surgical coordinators, using a random number table, and a single blind procedure. The patients' age, gender, tumor size, and thyroid size were not statistically different between the two groups (Table 1). The thyroid size was determined by weighing surgically extracted specimen prior to fixation in formalin. At the time of thyroid surgery, identical surgical instruments, including a general electrocautery, were used, however, Harmonic scalpels and postsurgical fibrin sealants were not used. We separately ligated the branches of the upper thyroid artery and middle thyroid vein. Furthermore, hemostasis of other small blood vessels was achieved with bipolar electrocautery. After completion of the hemostasis and irrigation procedure, a Jackson-Pratt drain (Sewoon Medical Co., Cheonan, Korea) with a 7 mm lumen was inserted and connected to a 100 mL drainage tube (Evacuator Barovac, 100 mL, Sewoon Medical Co., Cheonan, Korea) prior to the completion of the surgery in both groups. After sequentially suturing the strap muscle, subcutaneous tissues, and the skin, all wound drainage was collected in a drainage bag. The drainage tube of the natural drainage group was clamped with forceps and the volume was measured every 3 hours by loosening the forceps for 1 minute. For the negative pressure drainage group, drainage tubes were inserted by the method identical to that of the natural drainage group, and the suction tube was clamped with forceps for 1 minute and the drainage volume was measured every 3 hours. The rest of the treatments for the two groups were identical. The drainage tube was removed when 24-hour drainage volume was less than 20 mL for 2 consecutive days. Patients without medical problems were discharged on the day of removal of the drainage tubes or the next day. The drainage volumes of the natural two groups (measured every 3 hours) as well as total drainage volumes for initial 24, 48, and 72 hours postoperatively were analyzed with the paired t-test method using SPSS version 18.0. (SPSS Inc., Chicago, IL, USA). A p value <0.05 was considered to be statistically significant.
The use of a negative pressure drainage tube significantly increased the initial drainage volume after a thyroidectomy (Figs. 2 and 3). In the negative pressure drainage group, the drainage volume measured every 3 hours was shown to be larger than that of the natural drainage group (Fig. 2). During the initial 24 hours from the time of completion of surgery, the drainage volume in the negative pressure drainage group was 41.68±3.93 mL, and that in the natural drainage group was 25.3±2.68 mL, which was 40.1% smaller with a statistically significant difference (p<0.001). The sum of the drainage volumes at 48 hours postoperatively for the negative pressure drainage group was 35.19±4.26 mL, and that of the natural drainage group was 21.53±2.90 mL, a 38.8% reduction (p<0.001). However, the difference in the drainage volumes on days 3 and 4 postoperatively was not statistically significant.
After surgery, the two groups were examined during hospitalization period as well as 2 weeks and 3 months after surgery in outpatient clinics, and hematomas, seromas, and inflammation were not observed in the surgical area. Transient hypocalcemia and vocal cord palsy were detected, however, the patients recovered within 3 month and there was no statistical significance (Table 2).
As thyroid ultrasonography screening tests become generalized, thyroid carcinoma is being diagnosed earlier, and cases of thyroidectomy are rapidly on the rise. Factors that affect the drainage volume after thyroid surgery are body mass index of patients, surgical techniques (whether electrocautery was used, etc.), lymph nodes dissection, and placement of drainage tubes. In addition to studies on patient factors, numerous studies have been done on drainage tubes, which are controlled by surgeons during the surgical procedure.10,13 At the time of thyroid surgery, Harmonic scalpels (Ethicon Endo-Surgery, Cincinnati, OH, USA), endoscopes, or robots are used, and drainage tubes are not inserted in some cases. Nevertheless, to prevent hematomas and remove serous fluid, closed suction tubes have generally been inserted in many countries. In the United States, the majority of patients receive no drain, and they are discharged the next day after total thyroidectomy. It probably decreases the length of hospital stay.
Conventionally, the drainage tube is removed when the drainage volume decreases to less than 20 to 30 mL per day, and the patient is discharged, and follow-ups are performed in outpatient clinics. The drainage volume is an important factor that determines hospitalization period. Thus, shortening the hospital stay by reducing the drainage volume not only decreases the medical cost to patients, but it also decreases the discomfort of patients and their guardians.
Nonetheless, the installation of drainage tubes after thyroid surgery is still controversial. Ardito, et al.12 stated the necessity of conventional installation of thyroid drainage tubes after analyzing surgical findings of 1000 cases of thyroid surgery. In contrast, Ariyanayagam, et al.14 retrospectively analyzed the outcomes of 250 cases of thyroid surgery in which drainage tubes were not installed, and recommended that the placement of drainage tubes was not required. Pothier15 performed meta-analyses and reported that after thyroid surgery, the development of early or late hematomas or seromas in the neck was not different between drainage and no drainage groups. The results showed that the incidence of complications between drainage and no drainage groups was not statistically different, nor was it between the drainage group with suction drainage tubes and the group with Penrose drainage tubes.3 Numerous studies have focused on the installation of drainage tubes after thyroid surgery, but none has yet reported drainage volumes under conditions without negative drainage tubes.
Therefore, in order to accurately measure actual drainage volume after thyroid surgery, we inserted drainage tubes and measured the volume every 3 hours after surgery. In our study, for the control group, although negative pressure tubes were inserted similarly to the negative pressure patient group, the tubes were clamped with forceps to prevent the effect of negative pressure on the surgical areas through the drainage tubes. To avoid the effect of negative pressure as much as possible, the system was designed to remove the retained fluid every 3 hours after surgery and to measure it at consistent times. Moreover, during the design stage of the study, patients who received anterior lymph node dissection were excluded from the study to reduce errors in the increase of drainage volume.
Our results showed that the volume of drainage in the natural drainage group at 24 and 48 hours postoperatively was smaller than that in the negative pressure drainage group. In particular, the drainage volume of the natural drainage group during the first 24 hours postoperatively was 25.3±2.68 mL, which was slightly more than the standard drainage of 20 mL. The irrigation procedure with saline in the surgical areas prior to the insertion of the drainage tubes postoperatively or the drainage tube themselves may have increased the drainage volume in some cases.
Nevertheless, our study may not have accurately measured the entire natural drainage volume after surgery, and the negative pressure could be the only factor that determines the difference in drainage volumes between the groups. The results of our study, however, show that the drainage volume increased by approximately 30% in the negative pressure drainage group. The major cause could be osmotic pressure due to negative pressure in the closed cavity. In addition, the insertion of drainage tube itself may increase the drainage volume by inducing inflammation. Therefore, the drainage volumes of the first and second days postoperatively were comparable to the removal by drainage tubes (20 to 30 mL/day), therefore, surgery without drainage tubes may be possible in patients who receive a total thyroidectomy only. It has also been suggested that in patients who receive a total thyroidectomy and anterior lymph node dissection simultaneously, the drainage volume is increased depending on the range of lymph node dissection, and thus, surgery without drainage tubes may not be safe.
Numerous studies on lymph node dissection and drainage volume have already been done in entire surgical fields. As surgical range for lymph nodes increases, the risk of inaccurate treatment of adjacent structures generally increases, consequently increasing the drainage volume as lymphovascular injury increases. Numerous studies on wound healing in relation to the pressure from negative pressure drainage tubes and the recovery of patients have also been done. In particular, in patients who underwent lymph node dissection, negative pressure drainage tubes with low pressure or appropriate pressure are helpful in lymph node sealing; however, high pressure drainage tubes interfere with lymph node sealing and increase drainage volume.5,9,10,13,14
Recently, an interest in no drainage thyroidectomy has been increasing. However, if the advantages of such a procedure do not guarantee the safety of patients, the results can not be beneficial. In several previous studies, the use of fibrin sealants after thyroidectomy has been shown to reduce or avoid the use of drainage tubes. In these studies, however, patients were limited to those who received a partial resection, who received only a parathyroidectomy, or who were mixed with patients who received a total thyroidectomy, and thus, careful interpretation and clinical application are important.3,6,16,17 If a total thyroidectomy is performed by a surgeon with abundant experience, no drainage surgery is considered to be relatively safe.
Our results suggest that in the cases of total thyroidectomy only, the drainage volume tended to be smaller than that of conventional surgery where drainage tubes were installed.
In conclusion, during initial 24 and 48 hours after a total thyroidectomy, the drainage volume increased by approximately 30%, in the negative pressure drainage group, compared to the natural drainage group.
Figures and Tables
 | Fig. 2The amount of surgical wound drainage was compared at every 3 hours between a natural drain group (n=30) and a negative drain group (n=32) of patients who received total thyroidectomy. The amount of drainage during the postoperative every 3 hours significantly increased in a negative drain group within first 24 hour (*p<0.05, independent t-test). |
 | Fig. 3The amount of surgical wound drainage was compared at every 24 hours between a natural drain group (n=30) and a negative drain group (n=32) of patients who received total thyroidectomy. The amount of drainage during the first and second 24 hours significantly increased in a negative drain group (*p<0.05, Student t-test). |
References
1. Miccoli P, Berti P, Dionigi G, D'Agostino J, Orlandini C, Donatini G. Randomized controlled trial of harmonic scalpel use during thyroidectomy. Arch Otolaryngol Head Neck Surg. 2006. 132:1069–1073.

2. Patel M, Garg R, Rice DH. Fibrin glue in thyroid and parathyroid surgery: is under-flap suction still necessary? Ear Nose Throat J. 2006. 85:530–532.

3. Hurtado-López LM, López-Romero S, Rizzo-Fuentes C, Zaldívar-Ramírez FR, Cervantes-Sánchez C. Selective use of drains in thyroid surgery. Head Neck. 2001. 23:189–193.

4. Karayacin K, Besim H, Ercan F, Hamamci O, Korkmaz A. Thyroidectomy with and without drains. East Afr Med J. 1997. 74:431–432.
5. Lee SW, Choi EC, Lee YM, Lee JY, Kim SC, Koh YW. Is lack of placement of drains after thyroidectomy with central neck dissection safe? A prospective, randomized study. Laryngoscope. 2006. 116:1632–1635.

6. Peix JL, Teboul F, Feldman H, Massard JL. Drainage after thyroidectomy: a randomized clinical trial. Int Surg. 1992. 77:122–124.
7. Ruark DS, Abdel-Misih RZ. Thyroid and parathyroid surgery without drains. Head Neck. 1992. 14:285–287.

9. Bui TD, Huerta S, Gordon IL. Negative pressure wound therapy with off-the-shelf components. Am J Surg. 2006. 192:235–237.

10. Chintamani , Singhal V, Singh J, Bansal A, Saxena S. Half versus full vacuum suction drainage after modified radical mastectomy for breast cancer-a prospective randomized clinical trial [ISRCTN24484328]. BMC Cancer. 2005. 5:11.
11. Khanna J, Mohil RS, Chintamani , Bhatnagar D, Mittal MK, Sahoo M, et al. Is the routine drainage after surgery for thyroid necessary? A prospective randomized clinical study [ISRCTN63623153]. BMC Surg. 2005. 5:11.
12. Ardito G, Revelli L, Guidi ML, Murazio M, Lucci C, Modugno P, et al. [Drainage in thyroid surgery]. Ann Ital Chir. 1999. 70:511–516.
13. Sanabria A, Carvalho AL, Silver CE, Rinaldo A, Shaha AR, Kowalski LP, et al. Routine drainage after thyroid surgery--a meta-analysis. J Surg Oncol. 2007. 96:273–280.

14. Ariyanayagam DC, Naraynsingh V, Busby D, Sieunarine K, Raju G, Jankey N. Thyroid surgery without drainage: 15 years of clinical experience. J R Coll Surg Edinb. 1993. 38:69–70.
15. Pothier DD. The use of drains following thyroid and parathyroid surgery: a meta-analysis. J Laryngol Otol. 2005. 119:669–671.

16. Singh B, Lucente FE, Shaha AR. Substernal goiter: a clinical review. Am J Otolaryngol. 1994. 15:409–416.

17. Wihlborg O, Bergljung L, Mårtensson H. To drain or not to drain in thyroid surgery. A controlled clinical study. Arch Surg. 1988. 123:40–41.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download