Abstract
Purpose
Acute pancreatitis is one of the potentially lethal complications that occurs after cardiac surgery. We tried to identify risk factors for and the prognosis of acute pancreatitis after cardiac valve surgery with cardiopulmonary bypass.
Materials and Methods
We retrospectively analyzed a database of consecutive patients who underwent cardiac valve surgery with cardiopulmonary bypass between January 2005 and April 2010 at our institution. Patients were classified as having acute pancreatitis based on serum lipase concentration and clinical symptoms (lipase ≥180 U/L or ≥60 U/L with relevant symptoms).
Results
Of the 986 patients who underwent cardiac valve surgery with cardiopulmonary bypass, 58 (5.9%) patients developed post-operative pancreatitis. Post-operative hospital stay was significantly longer (29.7±45.6 days vs. 12.4±10.7 days, p=0.005) and in-hospital mortality rate was higher (15.5% vs. 2.0%, p<0.001) in patients with post-operative pancreatitis than those without. Hypertension, chronic kidney disease, and peri-operative use of norepinephrine were identified as independent risk factors for developing pancreatitis after cardiac valve surgery.
Conclusion
We found that acute pancreatitis after cardiac valve surgery requires longer hospitalization and increases the in-hospital mortality rate. Clinicians should be aware that patients could develop pancreatitis after cardiac valve surgery, especially in patients with hypertension and chronic kidney disease treated with norepinephrine.
Gastrointestinal complications after cardiovascular surgery are important for the prognosis of patients.1-6 However, the management of gastrointestinal complications is often difficult, and mortality can occur in severe cases. The most common complications are gastroduodenal ulcers, enterocolitis, and ischemic colitis. To manage these complications, procedures such as endoscopy or transfusion may be needed, and longer post-operative hospital stays and higher costs can be incurred. In order to prevent gastrointestinal complications and decrease their associated morbidity and mortality, there have been many studies regarding their incidence, risk factors, and management.
Acute pancreatitis is an inflammatory disorder with a variety of etiologies, including obstruction (gallstone, malignancy, surgery, and endoscopic retrograde cholangiopancreatography), vascular insufficiency, and toxic agents (alcohol, azathioprine, etc.). The widespread pathophysiological mechanisms are involved in the inflammatory process and lead to a variety of systemic complications.7 There is no effective way to manage acute pancreatitis except conservative treatment, and the outcome depends on its severity and the presence of organ failure. Therefore, it has been emphasized for many years to predict disease severity at an early stage and to apply intense treatment in severe cases.7
After cardiac surgery, acute pancreatitis is a potentially fatal complication leading to high mortality.1,2,6,8,9 While the significance is well recognized, several of its indicators remain controversial. The incidence of acute pancreatitis varies depending on the type of surgery and diagnostic criteria, ranging from 0.05% to 19%.5,6,8-12 Additionally, asymptomatic hyperamylasemia is more frequently seen in 24% to 85% of patients after cardiac surgery.10,11,13-15 Even all patients do not progress to symptomatic pancreatitis, hyperamylasemia alone may be associated with higher post-operative mortality.10,11 However, we do not know much about what is important in the development of symptomatic or asymptomatic pancreatitis and how they affect the clinical outcomes of cardiac surgery.
Therefore, we evaluated the incidence, risk factors, and clinical implications of acute pancreatitis after cardiac valve surgery with cardiopulmonary bypass (CPB) at our institution.
We retrospectively analyzed the database of all patients who underwent cardiac valve surgery with CPB between January 2005 and April 2010 at Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. Demographic, clinical, and laboratory data were collected from medical records that were documented at the time of treatment. These data included gender, age, co-morbidities (hypertension, diabetes mellitus, and chronic kidney disease), drug history, smoking history, pre-operative ejection fraction by echocardiography, peri-operative use of norepinephrine, serum amylase and lipase concentrations on post-operative day 2, duration of CPB, presence of post-operative complications, post-operative hospital stay, and in-hospital mortality. The diagnostic criteria for post-operative pancreatitis was an elevated serum lipase concentration (≥180 U/L) three-fold greater than the upper limit of normal concentration, or the presence of relevant symptoms and/or signs (abdominal pain, abdominal distention, nausea, vomiting and ileus) together with serum lipase concentration greater than the upper limit of normal concentration (≥60 U/L) on the second day after surgery.16 When post-operative pancreatitis was diagnosed, patients were conservatively treated with bowel rest and/or proteinase inhibitor according to the severity. The Institutional Review Board of Severance Hospital, Yonsei University approved this retrospective study.
Continuous variables are presented as mean±standard deviation and were compared using the Wilcoxon rank-sum test. Intergroup comparisons of categorical variables were performed by Pearson χ2 test or Fisher's exact test. To identify independent factors associated with the development of post-operative pancreatitis, explanatory items were selected using univariate analysis, followed by multivariate logistic regression analysis. We applied a backward stepwise selection procedure beginning with variables that exhibited a p value less than 0.05 in univariate analysis. Adjusted odds ratios (AOR) were calculated to measure the degree of associations, and Hosmer-Lemeshow goodness-of-fit analyses were used to calibrate multivariate logistic regression. We considered p values less than 0.05 as statistically significant and all statistical tests were 2-sided. Statistical analyses were performed using SPSS 18.0 for Windows (SPSS Inc., Chicago, IL, USA).
A total 986 consecutive patients, 460 males (46.7%) and 526 females (53.3%), underwent cardiac valve surgery with CPB during the study period, and their mean age was 56.9±14.8 years. Two-thirds of the patients (669 patients) underwent single valve surgery, and one-third (317 patients) underwent double valve surgery. The post-operative hospital stay was 13.4±15.6 days and the in-hospital mortality rate was 2.8% (28 of 986 patients).
Fulfilling the above-mentioned criteria in the methods section, 58 patients (5.9%) were diagnosed with post-operative pancreatitis, of whom 27 patients developed isolated hyperlipasemia and 31 patients developed symptomatic hyperlipasemia. Alcohol or drug induced pancreatitis was ruled out by preoperative history taking, and acute pancreatitis by gallstone or pancreatic neoplasm was not identified during the follow-up period in these patients. The most common symptoms in these patients were abdominal pain (16 of 58 patients, 27.6%) and nausea and vomiting (13 of 58 patients, 22.4%), followed by fever (11 of 58 patients, 19.0%). Pleural effusion was the most common accompanying complication (17 of 58 patients, 29.3%), followed by acute renal failure (15 of 58 patients, 25.9%), infection (11 of 58 patients, 19.0%) and upper gastrointestinal bleeding (6 of 58 patients, 10.3%).
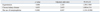
Comparative analysis of clinical data on the development of post-operative pancreatitis revealed that there is no significant difference in age, gender, history of diabetes, smoking history, type of surgery, or mean CPB time. Hypertension (46.6% vs. 24.8%) and chronic kidney disease (13.8% vs. 2.7%) were more common in patients with post-operative pancreatitis (p<0.001). Preoperative ejection fraction was lower in patients with post-operative pancreatitis (58.0±12.9%) than those without post-operative pancreatitis (60.6±12.2%), but the difference was not statistically significant (p=0.116). Patients with post-operative pancreatitis were more frequently treated with norepinephrine during peri-operative period (70.7% vs. 26.1%, p<0.001). The serum amylase was 523.9±470.1 U/L in patients with post-operative pancreatitis and 224.8±308.1 U/L in those without post-operative pancreatitis (p<0.001).
Patients with post-operative pancreatitis had a longer post-operative hospital stay (29.7±45.6 days vs. 12.4±10.7 days, p=0.005) and a higher in-hospital mortality rate (15.5% vs. 2.0%; p<0.001) than those without post-operative pancreatitis. The odds ratio of in-hospital mortality being associated with post-operative pancreatitis was 8.787 [95% confidence interval (CI); 3.780-20.428]. Table 1 summarizes the patients' clinical data and outcomes of cardiac valve surgery.
Univariate regression analyses indicated that hypertension (p<0.001), chronic kidney disease (p<0.001), and the use of norepinephrine (p<0.001) were significantly associated with post-operative pancreatitis. According to multivariate regression analysis, hypertension (AOR=2.263, 95% CI; 1.290-3.969), chronic kidney disease (AOR=2.653, 95% CI; 1.080-6.516), and the use of norepinephrine (AOR=6.047, 95% CI; 3.334-10.968) were identified as independent risk factors for post-operative pancreatitis (Table 2). The p value calculated by the Hosmer-Lemeshow χ2 statistic was 0.389, and the model showed no evidence of a lack of fit.
We identified that post-operative pancreatitis adversely affected clinical outcomes of cardiac valve surgery by increasing hospital stay and mortality. Previous studies reported that splanchnic ischemia during cardiac surgery might cause pancreatic cellular injury,8-10,15 and several risk factors have also been suggested.8-10 However, there is a lack of data for the clinical implications. Patients with acute pancreatitis often require one or more days of fasting for bowel rest depending on the severity as well as additional time in the hospital to evaluate and treat other associated complications such as pleural effusion, acute renal failure, infection, gastrointestinal bleeding, and acute cholecystitis.9-11 Patients with post-operative pancreatitis may take more time to recover from surgery and sometimes do not recover because acinar cell injury results from local injury, systemic inflammation, and subsequent multi-organ failure. This implies that physicians should carefully monitor these patients for the development of acute pancreatitis after surgery.
Post-operative pancreatitis occurs unpredictably and may be difficult to diagnose. According to an autopsy study, the diagnosis of pancreatitis was sometimes missed because of the absence of pain, tenderness, and hyperamylasemia.8 Considering isolated hyperamylasemia may have the potential to deteriorate the clinical course of patients and increase the risk of mortality,11 careful attention to pancreatic injury should be given in asymptomatic patients, especially after cardiac surgery. Due to the diagnosis of acute pancreatitis being largely based on clinical presentation with the assistance of laboratory findings,17 we assumed that some cases of asymptomatic pancreatitis were missed and its influence on clinical progress might be ignored. To identify the existence of postoperative pancreatitis, we checked the serum lipase concentration in all patients after cardiac valve surgery. Even though amylase is the most commonly used serum marker for diagnosing acute pancreatitis, it is neither specific nor sensitive for detecting pancreatic cellular injury because post-operative hyperamylasemia may result from an increased production of either pancreatic or salivary type amylase11,14,15 and decreased clearance of amylase.18 In contrast, lipase is a more sensitive and specific biomarker that is done as a single laboratory test for acute pancreatitis.16,19-21 Lipase increased earlier and to a greater extent than total amylase, and the peak activities of lipase and pancreatic type amylase in the serum have shown significant correlation.14 In addition, serum lipase remains elevated for a longer period of time than serum amylase.22 When the serum lipase level was elevated three times greater than the upper limit of normal level, the diagnostic accuracy of acute pancreatitis was improved.19
Compared to previous studies, we detected a slightly higher incidence of acute pancreatitis after cardiac valve surgery (5.9%). Perez, et al.9 reported that acute pancreatitis occurred in 39 of 10249 (0.6%) cardiac surgery cases, and other studies reported similar incidences.6,10,11 We may explain the difference in the incidence as follows. Firstly, the diagnostic criteria of acute pancreatitis in other studies were more restrictive than those in our study. Perez, et al.9 defined acute pancreatitis as the presence of relevant symptoms together with elevated serum amylase and lipase level. The other studies included serum isoamylase or urine amylase to diagnose acute pancreatitis,10,11 and even computed tomography imaging was included to make a diagnosis.6,11 At our hospital, we uniformly checked serum amylase and lipase of all patients on the second day of cardiac valve surgery and defined the criteria more extensively. We defined the criteria in this manner because acute pancreatitis may occur without symptoms or elevation of pancreatic enzyme8 and asymptomatic pancreatic injury presenting isolated hyperamylasemia or hyperlipasemia can affect clinical outcomes after surgery. Therefore, we were able to detect more cases of post-operative pancreatitis including even asymptomatic patients.11 Secondly, the incidence of gastrointestinal complications differs depending on the type of cardiovascular surgery. This study focused on cardiac valve surgery, while other studies included various types of cardiovascular surgery such as coronary artery bypass grafting, aortic surgery, or correction of congenital heart disease.2,6,8,9,13-15 Cardiac valve surgery may be more susceptible to acute pancreatitis than coronary bypass surgery due to hemodynamic problems that result in splanchnic ischemia.10 Thromboemboli detached from prosthetic valves may result in vascular ischemia, which may represent a common pathway for pancreatitis in patients after cardiac valve surgery.14 Another possible reason may be that CPB time in our study was rather long (132.4±50.8 min) compared with that in other studies (83.5-124 min).10,13,23 Prolonged CPB is associated with higher incidence of complications2,9,10 because long duration of CPB causes prolonged reduction in pancreatic blood flow, resulting in pancreatic acinar cell injury.3 For these reasons, our data showed higher incidence of post-operative pancreatitis.
The main pathogenic mechanism for post-operative pancreatitis may be pancreatic injury by inadequate splanchnic perfusion.24 The pancreas is particularly susceptible to hypoxia, therefore factors including splanchnic ischemia may be predicting factors for post-operative pancreatitis. In our study, we identified that hypertension and the use of norepinephrine are associated with the development of acute pancreatitis after cardiac valve surgery. Impaired homeostasis in hypertensive patients prevents proper reaction to hemodynamic instability during the peri-operative period and leads to splanchnic ischemia. Norepinephrine also increases sympathetic vasoconstriction of the mesenteric vasculature,25 and this may result directly in pancreatic cellular injury. Likewise, previous studies demonstrate that cardiac dysfunction and low cardiac output were significant risk factors,10 and patients with post-operative pancreatitis in our study had lower pre-operative ejection fraction than patients without pancreatitis without a statistical difference. We suggest that ejection fraction did not represent vasodynamic status as properly as cardiac output because it did not reflect the systemic volume status. Therefore, indicators properly representing vasodynamic status should be assessed before surgery.
Our study has several limitations. First, although the data were obtained prospectively, the analyses were performed retrospectively, which may have affected the study due to the limitations of such an investigational design. Radiologic evaluation was not routinely performed in all the patients who were suspected of having acute pancreatitis, therefore the severity of pancreatic injury could not be measured objectively. Moreover, we did not check the preoperative serum level of amylase and lipase, which meant that the possibility that patients already had hyperlipasemia before surgery could not be excluded. Furthermore, it was not clearly determined whether systemic or local complications that occurred in postoperative pancreatitis patients were caused by pancreatitis or by other problems. However, these complications could be associated with other ischemic causes that might have induced acute pancreatitis. Further prospective studies are needed to identify the causal relationship between these complications and pancreatitis.
In conclusion, post-operative pancreatitis after cardiac valve surgery occurred frequently and affected the clinical outcome of patients. Especially, patients with hypertension or chronic kidney disease and those who were treated with norepinephrine during the peri-operative period were more susceptible to pancreatitis. Checking serum lipase is a simple and reasonable method to detect acute pancreatitis in patients after cardiac valve surgery. Therefore, we suggest that clinicians assess risk factors for acute pancreatitis before cardiac valve surgery and remain vigilant for signs and symptoms after surgery. Further studies regarding prevention and early management of acute pancreatitis in this setting are warranted.
References
1. Krasna MJ, Flancbaum L, Trooskin SZ, Fitzpatrick JC, Scholz PM, Scott GE, et al. Gastrointestinal complications after cardiac surgery. Surgery. 1988. 104:773–780.
2. D'Ancona G, Baillot R, Poirier B, Dagenais F, de Ibarra JI, Bauset R, et al. Determinants of gastrointestinal complications in cardiac surgery. Tex Heart Inst J. 2003. 30:280–285.
3. Sanisoglu I, Guden M, Bayramoglu Z, Sagbas E, Dibekoglu C, Sanisoglu SY, et al. Does off-pump CABG reduce gastrointestinal complications? Ann Thorac Surg. 2004. 77:619–625.

4. Musleh GS, Patel NC, Grayson AD, Pullan DM, Keenan DJ, Fabri BM, et al. Off-pump coronary artery bypass surgery does not reduce gastrointestinal complications. Eur J Cardiothorac Surg. 2003. 23:170–174.

5. Mangi AA, Christison-Lagay ER, Torchiana DF, Warshaw AL, Berger DL. Gastrointestinal complications in patients undergoing heart operation: an analysis of 8709 consecutive cardiac surgical patients. Ann Surg. 2005. 241:895–901.
6. Achouh PE, Madsen K, Miller CC 3rd, Estrera AL, Azizzadeh A, Dhareshwar J, et al. Gastrointestinal complications after descending thoracic and thoracoabdominal aortic repairs: a 14-year experience. J Vasc Surg. 2006. 44:442–446.

8. Haas GS, Warshaw AL, Daggett WM, Aretz HT. Acute pancreatitis after cardiopulmonary bypass. Am J Surg. 1985. 149:508–515.

9. Perez A, Ito H, Farivar RS, Cohn LH, Byrne JG, Rawn JD, et al. Risk factors and outcomes of pancreatitis after open heart surgery. Am J Surg. 2005. 190:401–405.

10. Fernández-del Castillo C, Harringer W, Warshaw AL, Vlahakes GJ, Koski G, Zaslavsky AM, et al. Risk factors for pancreatic cellular injury after cardiopulmonary bypass. N Engl J Med. 1991. 325:382–387.

11. Rattner DW, Gu ZY, Vlahakes GJ, Warshaw AL. Hyperamylasemia after cardiac surgery. Incidence, significance, and management. Ann Surg. 1989. 209:279–283.
12. Colon R, Frazier OH, Kahan BD, Radovancevic B, Duncan JM, Lorber MI, et al. Complications in cardiac transplant patients requiring general surgery. Surgery. 1988. 103:32–38.
13. Wan S, Arifi AA, Chan CS, Ng CS, Wan IY, Lee TW, et al. Is hyperamylasemia after cardiac surgery due to cardiopulmonary bypass? Asian Cardiovasc Thorac Ann. 2002. 10:115–118.

14. Kazmierczak SC, Van Lente F. Incidence and source of hyperamylasemia after cardiac surgery. Clin Chem. 1988. 34:916–919.

15. Nys M, Venneman I, Deby-Dupont G, Preiser JC, Vanbelle S, Albert A, et al. Pancreatic cellular injury after cardiac surgery with cardiopulmonary bypass: frequency, time course and risk factors. Shock. 2007. 27:474–481.

16. Banks PA, Freeman ML. Practice Parameters Committee of the American College of Gastroenterology. Practice guidelines in acute pancreatitis. Am J Gastroenterol. 2006. 101:2379–2400.

17. Moossa AR. Current concepts. Diagnostic tests and procedures in acute pancreatitis. N Engl J Med. 1984. 311:639–643.

18. Paajanen H, Nuutinen P, Harmoinen A, Pöyhönen M, Pitkänen O, Nordback I, et al. Hyperamylasemia after cardiopulmonary bypass: pancreatic cellular injury or impaired renal excretion of amylase? Surgery. 1998. 123:504–510.

19. Sutton PA, Humes DJ, Purcell G, Smith JK, Whiting F, Wright T, et al. The role of routine assays of serum amylase and lipase for the diagnosis of acute abdominal pain. Ann R Coll Surg Engl. 2009. 91:381–384.

20. Smotkin J, Tenner S. Laboratory diagnostic tests in acute pancreatitis. J Clin Gastroenterol. 2002. 34:459–462.

21. Treacy J, Williams A, Bais R, Willson K, Worthley C, Reece J, et al. Evaluation of amylase and lipase in the diagnosis of acute pancreatitis. ANZ J Surg. 2001. 71:577–582.

22. Orebaugh SL. Normal amylase levels in the presentation of acute pancreatitis. Am J Emerg Med. 1994. 12:21–24.

23. Klar E, Messmer K, Warshaw AL, Herfarth C. Pancreatic ischaemia in experimental acute pancreatitis: mechanism, significance and therapy. Br J Surg. 1990. 77:1205–1210.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download