Abstract
Purpose
Intravenous lipid emulsions have been used to treat the systemic toxicity of local anesthetics. The goal of this in vitro study was to examine the effects of lipid emulsions on the norepinephrine-mediated reversal of vasodilation induced by high doses of levobupivacaine, ropivacaine, and mepivacaine in isolated endothelium-denuded rat aorta, and to determine whether such effects are associated with the lipid solubility of local anesthetics.
Materials and Methods
The effects of lipid emulsions (0.30, 0.49, 1.40, and 2.61%) on norepinephrine concentration-responses in high-dose local anesthetic (6×10-4 M levobupivacaine, 2×10-3 M ropivacaine, and 7×10-3 M mepivacaine)-induced vasodilation of isolated aorta precontracted with 60 mM KCl were assessed. The effects of lipid emulsions on local anesthetic- and diltiazem-induced vasodilation in isolated aorta precontracted with phenylephrine were also assessed.
Results
Lipid emulsions (0.30%) enhanced norepinephrine-induced contraction in levobupivacaine-induced vasodilation, whereas 1.40 and 2.61% lipid emulsions enhanced norepinephrine-induced contraction in both ropivacaine- and mepivacaine-induced vasodilation, respectively. Lipid emulsions (0.20, 0.49 and 1.40%) inhibited vasodilation induced by levobupivacaine and ropivacaine, whereas 1.40 and 2.61% lipid emulsions slightly attenuated mepivacaine (3×10-3 M)-induced vasodilation. In addition, lipid emulsions attenuated diltiazem-induced vasodilation. Lipid emulsions enhanced norepinephrine-induced contraction in endothelium-denuded aorta without pretreatment with local anesthetics.
Conclusion
Taken together, these results suggest that lipid emulsions enhance the norepinephrine-mediated reversal of local anesthetic-induced vasodilation at toxic anesthetic doses and inhibit local anesthetic-induced vasodilation in a manner correlated with the lipid solubility of a particular local anesthetic.
Intravenous lipid emulsions have been used to treat systemic toxicity induced by local anesthetics including bupivacaine, levobupivacaine, ropivacaine, and mepivacaine.1-6 High doses of local anesthetics (levobupivacaine: 3×10-4 M, ropivacaine: 10-3 M, and mepivacaine: 10-2 M) induce inhibition of voltage-operated calcium channel-induced contraction, which may contribute to cardiovascular collapse.7-9 Recently, we reported that lipid emulsions reverse high-dose local anesthetic-induced vasodilation through the attenuation of local anesthetic-mediated inhibition of voltage-operated calcium channel-induced contraction in isolated rat aorta.7 The magnitude of the reversal of this vasodilation is strongly correlated with the lipid solubility of the particular local anesthetic.7 The combined treatment with lipid emulsion and epinephrine (for reversal of cardiac arrest due to the systemic toxicity of bupivacaine) produces a sustained and transient improvement of the hemodynamic profile compared with lipid emulsion alone.10-12 However, at epinephrine doses exceeding 10 µg/kg, the combined treatment impairs the hemodynamic profile compared with lipid emulsion alone.13 In addition, norepinephrine is a potent peripheral vasopressor, eliciting its primary effect on alpha-1 adrenoceptors, and appears to be most useful among the several vasopressors used for treatment of cardiovascular collapse induced by toxic doses of bupivacaine in rats.14,15 However, the effects of lipid emulsions on norepinephrine concentration-response curves in vasodilation induced by high-dose aminoamide local anesthetics remain unknown. Therefore, the goal of this in vitro study was to examine the effects of lipid emulsions on the norepinephrine-mediated reversal of severe vasodilation induced by high doses of local anesthetics in isolated endothelium-denuded rat aorta, and to determine whether these effects are associated with the lipid solubility of the particular local anesthetic. Based on a previous study, we tested the hypothesis that lipid emulsions enhance the norepinephrine-evoked contractile response of high-dose aminoamide local anesthetic-induced vasodilation in a manner correlated with the lipid solubility of the local anesthetic.7
All experimental procedures and protocols were approved by the Institutional Animal Care and Use Committee at Gyeongsang National University (September, 2010). All experimental procedures were performed in accordance with the Guide for the Care and Use of Laboratory Animals prepared by the National Academy of Sciences.
Preparation of aortic rings for tension measurements was performed as described previously.7 Male Sprague Dawley rats weighing 250-300 g were anesthetized by intramuscular injection of Zoletil 50 (15 mg/kg, Virbac Laboratories, Carros, France). The descending thoracic aorta was dissected, and surrounding connective tissue and fat were removed under microscopic guidance in a Krebs solution bath (118 mM NaCl, 4.7 mM KCl, 1.2 mM MgSO4, 1.2 mM KH2PO4, 2.4 mM CaCl2, 25 mM NaHCO3, and 11 mM glucose). The aortas were cut into 2.5-mm rings, suspended on Grass isometric transducers (FT-03, Grass Instrument, Quincy, MA, USA) under a 3.0-g resting tension in a 10-mL Krebs bath at 37℃, and aerated continuously with 95% O2 and 5% CO2 to maintain a 7.35-7.45 pH range. The rings were equilibrated for 120 min, changing the bath solution every 30 min. The endothelium was removed from some aortic rings by inserting a 25-gauge needle into the lumen of the rings and gently rubbing the ring for a few seconds. Once phenylephrine (10-8 M)-induced contraction had stabilized, endothelial denudation was confirmed by the observation of less than a 10% relaxation induced by acetylcholine (10-5 M). Each ring was used for only one concentration-response curve induced by norepinephrine, local anesthetics (i.e., levobupivaciane, ropivacaine, and mepivacaine), lipid emulsion (SMOFlipid® 20% emulsion: Fresenius Kabi Korea, Seoul, Korea), and diltiazem. The Krebs solution also contained the nitric oxide synthase inhibitor Nw-nitro-L-arginine methyl ester (10-4 M) to prevent release of endogenous nitric oxide from residual endothelium.7-9,16 The contactile response induced by isotonic KCl (60 mM) was measured for endothelium-denuded aorta, which was used for only norepinephrine concentration-response curves in aorta with resting tension, and used as a reference value.
The first series of experiments assessed the effects of lipid emulsions on the norepinephrine concentration-response curves in high-dose local anesthetic-induced vasodilation of endothelium-denuded aorta precontracted with 60 mM KCl. Local anesthetic (levobupivacaine, ropivacaine, and mepivacaine) treatment of isolated endothelium-denuded rat aorta produces vasoconstriction at low doses and vasodilation at high doses.7,17 Lipid emulsion also reverses high-dose local anesthetic-induced vasodilation in a manner dependent on the lipid solubility of local anesthetics.7 Thus, based on previous studies and lipid emulsion concentrations, which did not significantly affect high-dose local anesthetic-induced vasodilation in the preliminary experiment, both high-dose local anesthetic concentrations to produce vasodilation and lipid emulsion concentrations were chosen in our in vitro experiment.7,17 After administering high doses of local anesthetics [6×10-4 M levobupivacaine (levobupivacaine group), 2×10-3 M ropivacaine (ropivacaine group), and 7×10-3 M mepivacaine (mepivacaine group)] to produce stable and sustained vasodilation in endothelium-denuded aorta precontracted with isotonic 60 mM KCl, high-dose local anesthetic-induced vasodilated aortas were treated with or without lipid emulsions (0.30, 0.49, 1.40, and 2.16%) for 5 min before the addition of norepinephrine. In the levobupivacaine group, levobupivacaine (6×10-4 M)-induced vasodilated aortas were treated with or without 0.3% lipid emulsion. In the ropivacaine group, ropivacaine (2×10-3 M)-induced vasodilated aortas were treated with or without lipid emulsions (0.49 and 1.40%). In the mepivacaine group, mepivacaine (7×10-3 M)-induced vasodilated aortas were treated with or without lipid emulsions (1.40 and 2.61%). In addition, the effects of lipid emulsions on norepinephrine-induced contraction in endothelium-denuded aorta with resting tension and without local anesthetics were assessed. Lipid emulsions (0.30 and 0.49%) were added directly to the organ bath for 20 min before the addition of norepinephrine (10-9 to 10-6 M). Incremental concentrations of norepinephrine (10-9 to 10-4 M) were cumulatively added to the organ bath to generate norepinephrine concentration-response curves in endothelium-denuded aorta with toxic-dose local anesthetic-induced vasodilation (6×10-4 M levobupivacaine, 2×10-3 M ropivacaine, and 7×10-3 M mepivacaine) in the presence or absence of lipid emulsions. Subsequent concentrations of norepinephrine were added after the previous concentration produced a sustained and stable response for 5 min.
The effects of lipid emulsions on local anesthetic concentration-response curves in endothelium-denuded aorta precontracted with phenylephrine were assessed. The lipid emulsion was added directly to the organ bath for 20 min before the addition of phenylephrine. After phenylephrine (10-7 M)-induced contractions had stabilized, incremental concentrations of local anesthetics [levobupivacaine: 10-6 to 3×10-4 M (levobupivaciane group), ropivacaine: 10-6 to 10-3 M (ropivacaine group), and mepivacaine: 10-5 to 10-2 M (mepivacaine group)] were added to the organ bath to generate local anesthetic-induced concentration-response curves. In addition, the effects of lipid emulsions on the phenylephrine-induced precontracted aorta without local anesthetics were assessed. After phenylephrine (10-7 M)-induced contraction stabilized, the lipid emulsions (0.20, 0.49, 1.40, and 2.61%) were added directly to the organ bath to produce cumulative lipid emulsion concentration-response curves.
To investigate whether lipid emulsion-mediated attenuation of local anesthetic-induced vasodilation is a non-specific action associated with entrapment of lipid-soluble drug by lipid emulsion, we assessed the effects of lipid emulsions on diltiazem, a relatively lipid-soluble calcium channel antagonist, which induced vasodilation in endothelium-denuded aorta precontracted with 10-7 M phenylephrine.18 After phenylephrine (10-7 M)-induced contractions had stabilized in endothelium-denuded aorta pretreated with or without lipid emulsions (1.40 and 2.61%) for 20 min, incremental concentrations of diltiazem (10-8 to 3×10-4 M) were added to the organ bath to produce diltiazem concentration-response curves.
All drugs were of the highest commercially available purity. Norepinephrine, diltiazem, Nw-nitro-L-arginine methyl ester, phenylephrine, and acetylcholine were obtained from Sigma Aldrich (St. Louis, MO, USA). Levobupivacaine and ropivacaine were donated by Abbott Korea (Seoul, Korea) and AstraZeneca Korea (Seoul, Korea), respectively. Mepivacaine was donated by Hana Pharmaceutical Co., Ltd. (Gyeonggi-do, Korea). Lipid emulsion (SMOFlipid® 20% emulsion) was donated by Fresenius Kabi Korea (Seoul, Korea). All drug concentrations are expressed as the final molar concentration or as the final percentage of lipid emulsion in the organ bath. Unless otherwise stated, all other drugs were dissolved and diluted in distilled water.
Data are expressed as the mean±standard deviation (SD). Vascular responses induced by norepinephrine, local anesthetics, lipid emulsion, and diltiazem in endothelium-denuded aorta precontracted with isotonic 60 mM KCl or 10-7 M phenylephrine are expressed as the percent change from baseline precontraction induced by isotonic 60 mM KCl or 10-7 M phenylephrine. Contractile responses to norepinephrine in endothelium-denuded aorta with resting tension are expressed as a percentage of the maximum contraction in response to isotonic 60 mM KCl. The effects of lipid emulsions on cumulative concentration-response curves induced by norepinephrine, local anesthetics, and diltiazem and on phenylephrine-induced precontraction were analyzed with two-way analysis of variance followed by the Bonferroni post-test. p-values less than 0.05 were considered significant.
There was no significant difference in high-dose local anesthetic (6×10-4 M levobupivacaine, 2×10-3 M ropivacaine, and 7×10-3 M mepivacaine)-induced vasodilation (baseline tension) between lipid emulsion-pretreated aortas and controls before the addition of norepinephrine. Lipid emulsions (0.30%) enhanced norepinephrine-induced contraction in vasodilated aortas induced by 6×10-4 M levobupivacaine (p<0.05 vs. control at 3×10-8 to 10-4 M norepinephrine) (Fig. 1A). Lipid emulsion (0.49%) did not significantly alter norepinephrine-induced contraction during ropivacaine (2×10-3 M)-induced vasodilation, but 1.40% lipid emulsion enhanced norepinephrine-induced contraction during ropivacaine-induced vasodilation (p<0.05 vs. control at 3×10-7 to 10-4 M norepinephrine) (Fig. 1B). During mepivacaine (7×10-3 M)-induced vasodilation, 1.40% lipid emulsion did not significantly alter norepinephrine-induced contraction, whereas 2.61% lipid emulsion enhanced norepinephrine-induced contraction (p<0.05 vs. control at 3×10-6 to 10-4 M norepinephrine) (Fig. 1C). In addition, lipid emulsions (0.30 and 0.49%) enhanced norepinephrine-induced contraction in endothelium-denuded aortas without pretreatment with local anesthetics (p<0.01 vs. control at 3×10-9 and 10-8 M norepinephrine) (Fig. 2).
In endothelium-denuded aortas precontracted with 10-7 M phenylephrine, 0.20 and 0.49% lipid emulsions attenuated levobupivacaine-induced vasodilation in a concentration-dependent manner (p<0.05 vs. control at 10-4 and 3×10-4 M levobupivacaine) (Fig. 3A). Lipid emulsion at 0.20% had no effect on ropivacaine-induced vasodilation, whereas 0.49 and 1.40% lipid emulsions attenuated ropivacaine-induced vasodilation (p<0.05 vs. control at 10-4 to 10-3 M ropivacaine) in a concentration-dependent manner (Fig. 3B). However, 1.40 and 2.61% lipid emulsions slightly attenuated 3×10-3 M mepivacaine-induced vasodilation (p<0.001 vs. control) (Fig. 3C). In addition, the lipid emulsion (0.20 to 2.61%) itself had no effect on phenylephrine-induced contraction (Fig. 4).
Lipid emulsions (1.40 and 2.61%) attenuated diltiazem-induced vasodilation in endothelium-denuded aortas precontracted with 10-7 M phenylephrine in a concentration-dependent manner (p<0.05 vs. control) (Fig. 5).
Taken together, these results suggest that lipid emulsions enhance norepinephrine-induced vasoconstriction in high-dose local anesthetic-induced vasodilation and inhibit local anesthetic-induced vasodilation. This effect appears to be correlated with the lipid solubility of a particular local anesthetic.
Cardiac toxicity induced by bupivacaine inhibits sodium and L-type calcium channels.19 Levobupivacaine (10-5 M) exerts inhibitory effects on cardiac electrical activity and L-type calcium channels in isolated cardiac myocytes, leading to decreased cardiac output.20 Vasoconstriction induced by levobupivacaine, ropivacaine, and mepivacaine is dependent on calcium influx via voltage-operated calcium channels.8,9,21 However, high doses of levobupivacaine (3×10-4 M) and mepivacaine (3×10-3 and 10-2 M) attenuate voltage-operated calcium channel-induced contraction compared with control.8,9 In agreement with previous reports, high doses of levobupivacaine (6×10-4 M), ropivacaine (2×10-3 M), and mepivacaine (7×10-3 M) attenuated vasoconstriction induced by voltage-operated calcium channel activation (Fig. 1).7-9 Relatively low concentration (0.30%) of lipid emulsion enhanced norepinephrine-induced contraction in the vasodilation induced by 6×10-4 M levobupivacaine, whereas lipid emulsions at 1.40 and 2.61%, which are considered to be relatively high concentrations compared with 0.3% lipid emulsion used in this study, enhanced norepinephrine-induced contraction in the vasodilation induced by ropivacaine (2×10-3 M) and mepivacaine (7×10-3 M), respectively. The decreasing order of lipid solubility (logarithm of octanol/buffer partition coefficient at pH 7.40) of local anesthetics is as follows: levobupivacaine (2.539), ropivacaine (2.060), and mepivacaine (1.322).22 Considering the lipid solubilities of the local anesthetics, the minimum concentration of lipid emulsion (levobupivacaine: 0.30%, ropivacaine: 1.40%, and mepivacaine: 2.61%) that is required to enhance norepinephrine-induced vasoconstriction in vasodilated aorta induced by high doses of local anesthetics was inversely correlated with the lipid solubility of the local anesthetics. One of the suggested underlying mechanisms regarding lipid emulsions used for treatment of local anesthetic systemic toxicity is the "lipid sink theory", in which lipid-soluble local anesthetics move from tissues to lipids.23 Thus, as lipid emulsions are able to extract more local anesthetic with a high lipid solubility (e.g., levobupivacaine) than a local anesthetic with a low lipid solubility (e.g., mepivacaine), a relatively low concentration of lipid emulsion may be sufficient to enhance norepinephrine-induced vasoconstriction in levobupivacaine-induced vasodilation compared with mepivacaine-induced vasodilation. Consistent with a previous report suggesting that long-chain fatty acids stimulate voltage-operated calcium channels, lipid emulsions themselves increased norepinephrine-induced contraction of endothelium-denuded isolated aorta without local anesthetics, which may be associated with the stimulatory effects of lipid emulsions on voltage-operated calcium channels activated by norepinephrine (Fig. 2).24 This lipid emulsion-mediated voltage-operated calcium channel activation may be associated with a potential mechanism responsible for lipid emulsion therapy of local anesthetic systemic toxicity other than the "lipid sink theory".25 Lipid emulsion-mediated enhancement of norepinephrine-induced contraction (Fig. 2) may partially contribute to norepinephrine-mediated reversal of toxic-dose local anesthetic-induced vasodilation post-treated with lipid emulsion. In particular, lipid emulsion (2.61%)-mediated enhanced reversal of toxic-dose mepivacaine-induced vasodilation (Fig. 1C) may be due to lipid emulsion-mediated enhancement of norepinephrine-induced contraction via voltage-operated calcium channels activation. In previous in vivo studies involving cardiac arrest due to toxic doses of bupivacaine, a combined treatment with lipid emulsion and epinephrine provided better recovery than treatment with epinephrine alone.10,12 In addition, a previous in vivo study reported that norepinephrine, combined with a potent alpha-1 adrenoceptor agonistic effect and a less potent beta-1 adrenoceptor agonistic effect among various vasopressors, may be the best choice for treatment of bupivacaine-induced cardiac arrest when all others factors associated with overall recovery are considered.15 As suggested in previous in vivo studies, in terms of vascular tone recovery from severe arterial vasodilation caused by local anesthetic systemic toxicity, the combination of lipid emulsion and norepinephrine may contribute to better survival after cardiovascular collapse induced by toxic doses of levobupivacaine.10,12,15,19 However, further study of the effects of lipid emulsions on vasopressor-induced contraction of isolated vessels without local anesthetics or vasopressor-mediated reversal of toxic-dose local anesthetic-induced vasodilation in conditions of metabolic acidosis, which is commonly encountered after cardiovascular collapse due to local anesthetic systemic toxicity, is needed. In addition to "lipid sink theory", the possible mechanisms associated with lipid emulsion treatment of local anesthetic and other drug intoxication include improved fatty acid metabolism, membrane effects, cytoprotection, inotropic effects, and pharmacokinetic effects, and therefore, further research on the impact of lipid emulsion on vascular and cardiac physiology is needed.25,26
Lipid emulsions attenuate both vasoconstriction and vasodilation induced by levobupivacaine in isolated rat aorta.7 Similar to a previous report, pretreatment with lipid emulsions (0.20, 0.49, and 1.40%) attenuated the vasodilation induced by high concentrations of levobupivacaine and ropivacaine in a concentration-dependent manner, whereas pretreatment with 1.40 and 2.61% lipid emulsions slightly attenuated 3×10-3 M mepivacaine-induced vasodilation (Fig. 3).7 The increasing order of minimum concentrations of lipid emulsions required to attenuate local anesthetic-induced vasodilation is as follows: levobupivacaine: 0.20%, ropivacaine: 0.49%, and mepivacaine: 1.40%. Considering lipid solubility, the minimum concentration of lipid emulsions that is required to produce an inhibitory effect on local anesthetic-induced vasodilation appears to be inversely correlated with the lipid solubility of a particular local anesthetic.22 In addition, lipid emulsions themselves had no effect on phenylephrine-induced contraction (Fig. 4), suggesting that lipid emulsion-mediated attenuation of local anesthetic-induced vasodilation does not appear to be associated with the lipid emulsion-mediated enhancement of phenylephrine-induced contraction. As diltiazem is a relatively lipid-soluble calcium channel antagonist (octanol/water partition coefficient: 19.4), we used diltiazem in this study.18,27 We examined the effects of lipid emulsions on diltiazem-induced vasodilation to investigate whether the lipid emulsion-mediated attenuation of local anesthetic-induced vasodilation is a non-specific action indicating binding of lipid-soluble drug by lipid emulsions. As lipid emulsions (1.40 and 2.61%) attenuated the vasodilation induced by diltiazem in a concentration-dependent manner, these results suggest that lipid emulsion-mediated attenuation of local anesthetic-induced vasodilation is in fact non-specific binding of lipophilic drug by lipid emulsions.
The limitations of this study are as follows: 1) the clinical relevance of lipid emulsion-mediated enhancement of norepinephrine-induced vasoconstriction in vasodilation induced by high doses of local anesthetics must be tempered by the fact that aortas, regarded as a conduit vessel, were used in this in vitro experiment, whereas small resistance arterioles control organ blood flow; and 2) as vasoconstriction induced by levobupivacaine and mepivacaine is attenuated by endothelial nitric oxide release in endothelium-intact aorta, endothelial nitric oxide in an in vivo model may slightly modify lipid emulsion-mediated enhancement of norepinephrine-induced contraction obtained in this study which used endothelium-denuded aortas.7-9 Even with these limitations, because the high concentrations of levobupivacaine (6×10-4 M), ropivacaine (2×10-3 M), and mepivacaine (7×10-3 M) used in this experiment exceed the plasma concentrations of local anesthetics (levobupivacaine: 1.7 to 6.2×10-5 M, ropivacaine: 1.3 to 2.3×10-5 M, and mepivacaine: 1.8×10-5 M) that induce convulsions, cardiac arrest, loss of verbal contact, and agitation in animals and humans due to systemic toxicity of the local anesthetics, the combination treatment of lipid emulsion and norepinephrine may be more effective than treatment with only norepinephrine in terms of vascular tone recovery from severe arterial vasodilation and cardiac depression due to systemic toxicity induced by the accidental intravascular injection of local anesthetics.19,28-30 In addition, in terms of recovery of vascular tone affected by local anesthetic-induced vascular collapse, the combined treatment of lipid emulsion and norepinephrine may provide better reversal of vasodilation induced by toxic doses of levobupivacaine compared to vasodilation induced by toxic doses of mepivacaine. Intralipid® (Fresenius Kabi AB, Uppsala, Sweden) 20%, which is commonly used for the treatment of local anesthetic systemic toxicity, is an lipid emulsion composed entirely of long-chain triglyceride, whereas SMOFlipid® 20%, which is an lipid emulsion that was used in the current in vitro study, is composed of both long- (61) and medium-chain (39) triglycerides.31 In addition, the formulation of SMOFlipid® 20% contains 6% soybean oil, 6% medium-chain triglycerides, 5% olive oil, 3% fish oil, 0.02% tocopherol, 1.2% purified egg phospholipids, 2.5% glycerol, and water for injection.31 In this study, the minimum concentration (0.2 and 0.3%) of lipid emulsion required to enhance norepinephrine-mediated contraction of toxic-dose levobupivacaine-induced vasodilation and to inhibit levobupivacaine-induced vasodilation seems to be within average plasma concentration (final triglyceride concentration: 1%) achieved after intravenous infusion of the Intralipid® 20% used for treatment of toxic-dose bupivacaine-induced asystole in rats.32 However, further research regarding the appropriate dosing regimen for several kinds of lipid emulsions to reverse high-dose local anesthetic-induced vasodilaton is needed.
In conclusion, these results suggest that lipid emulsions enhance norepinephrine-mediated reversal of vasodilation induced by toxic does of local anesthetics in isolated endothelium-denuded aorta in a manner correlated with the lipid solubility of the local anesthetic. In addition, lipid emulsion-mediated augmentation of norepinephrine-induced contraction (Fig. 2) may be associated with a novel mechanism responsible for lipid emulsion therapy other than the "lipid sink theory".25 The magnitude of lipid emulsion-mediated attenuation of local anesthetic-induced vasodilation may be correlated with the lipid solubility of the local anesthetics, which is due to the non-specific binding of lipid-soluble drugs by lipid emulsions.
Figures and Tables
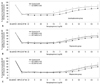 | Fig. 1Effects of lipid emulsions (LEs: 0.30, 0.49, 1.40, and 2.61%) on the norepinephrine concentration-response curves in high-dose levobupivacaine (LBV, A)-, ropivacaine (RPV, B)-, and mepivacaine (MPV, C)-induced vasodilation of isolated endothelium-denuded aorta precontracted with 60 mM KCl. Data are the means±SD expressed as the percentage of the maximal contraction induced by isotonic 60 mM KCl [100%=3.20±0.30 g (n=6) and 100%=2.96±0.35 g (n=6) for endothelium-denuded rings with control and 0.30% LE, respectively, in A; 100%=3.44±0.26 g (n=7), 100%=3.35±0.36 g (n=5), and 100%=3.30±0.22 g (n=7) for endothelium-denuded rings with control, 0.49% LE and 1.40% LE, respectively, in B; 100%=3.29±0.50 g (n=5), 100%=3.00±0.56 g (n=5), and 100%=3.08±0.19 g (n=5) for endothelium-denuded rings with control, 1.40% LE and 2.61% LE, respectively, in C]. N indicates the number of rats from which descending thoracic aortic rings were derived. *p<0.05, †p<0.01, and ‡p<0.001 versus control. SD, standard deviation. |
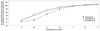 | Fig. 2Effects of lipid emulsions (LEs: 0.30 and 0.49%) on the norepinephrine concentration-response curves of isolated endothelium-denuded aorta without local anesthetics. Data are the means±SD expressed as the percentage of the maximal contraction induced by isotonic 60 mM KCl [100%=2.93±0.36 g (n=5), 100%=3.00±0.42 g (n=5), and 100%=2.74±0.44 g (n=5) for endothelium-denuded rings with control, 0.30% LE and 0.49% LE, respectively]. N indicates the number of rats from which descending thoracic aortic rings were derived. *p<0.001 and †p<0.01 versus control. SD, standard deviation. |
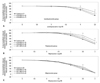 | Fig. 3The effects of lipid emulsions (LEs: 0.20, 0.49, 1.40, and 2.61%) on local anesthetic (levobupivacaine: A, ropivacaine: B, and mepivacaine: C)-induced concentration-response curves in isolated endothelium-denuded aorta precontracted with 10-7 M phenylephrine. Data are the means±SD expressed as the percentage of the maximal contraction induced by phenylephrine [10-7 M; 100%=2.99±0.34 g (n=7), 100%=3.09±0.35 g (n=5), and 100%=3.11±0.49 g (n=7) for endothelium-denuded rings with control, 0.20% LE and 0.49% LE, respectively, in A; 100%=3.42±0.43 g (n=6), 100%=3.30±0.38 g (n=5), 100%=3.50±0.40 g (n=6), and 100%=3.30±0.29 g (n=5) for endothelium-denuded rings with control, 0.20% LE, 0.49% LE, and 1.40% LE, respectively, in B; 100%=3.43±0.20 g (n=5), 100%=3.48±0.77 g (n=5), 100%=3.54±0.40 g (n=5), and 100%=3.46±0.36 g (n=5) for endothelium-denuded rings with control, 0.49% LE, 1.40% LE, and 2.61% LE, respectively, in C]. N indicates the number of rats from which descending thoracic aortic rings were derived. *p<0.05, †p<0.01, and ‡p<0.001 versus control. A: §p<0.001 versus 0.2% LE. B: §p<0.001 versus 0.49% LE. C: §p<0.001 versus 0.49% LE. SD, standard deviation. |
 | Fig. 4The lipid emulsion concentration-response curves in endothelium-denuded aorta precontracted with 10-7 M phenylephrine. Data are the means±SD expressed as the percentage of the maximal contraction induced by 10-7 M phenylephrine [100%=2.78±0.46 g (n=8) and 100%=2.68±0.45 g (n=8) for endothelium-denuded aortic rings with time-matched control and lipid emulsion, respectively]. N indicates the number of isolated descending thoracic aortic rings. SD, standard deviation. |
 | Fig. 5Effects of lipid emulsions (LEs: 1.40 and 2.61%) on diltiazem concentration-response curves in endothelium-denuded aorta precontracted with 10-7 M phenylephrine. Data are the means±SD expressed as the percentage of the maximal contraction induced by phenylephrine [10-7 M; 100%=2.64±0.44 g (n=6), 100%=2.51±0.22 g (n=5), and 100%=2.59±0.46 g (n=5) for endothelium-denuded rings with control, 1.40% LE, and 2.61% LE, respectively]. N indicates the number of rats from which descending thoracic aortic rings were derived. *p<0.05, †p<0.01 and ‡p<0.001 versus control. §p<0.05 and ∥p<0.01 versus 1.40% LE. SD, standard deviation. |
ACKNOWLEDGEMENTS
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science, and Technology (KRF-2011-0006783).
Notes
References
1. Charbonneau H, Marcou TA, Mazoit JX, Zetlaoui PJ, Benhamou D. Early use of lipid emulsion to treat incipient mepivacaine intoxication. Reg Anesth Pain Med. 2009; 34:277–278.

2. Schaeffer E, Rayaud L, Landy C, Boulland P, Favier JC. [Local anaesthetics intoxication, during ultrasound-guided axillary plexus block, treated by Intralipide]. Ann Fr Anesth Reanim. 2010; 29:929–930.
3. Sakai T, Manabe W, Kamitani T, Takeyama E, Nakano S. [Ropivacaine-induced late-onset systemic toxicity after transversus abdominis plane block under general anesthesia: successful reversal with 20% lipid emulsion]. Masui. 2010; 59:1502–1505.
4. Dix SK, Rosner GF, Nayar M, Harris JJ, Guglin ME, Winterfield JR, et al. Intractable cardiac arrest due to lidocaine toxicity successfully resuscitated with lipid emulsion. Crit Care Med. 2011; 39:872–874.

5. Weinberg G, Ripper R, Feinstein DL, Hoffman W. Lipid emulsion infusion rescues dogs from bupivacaine-induced cardiac toxicity. Reg Anesth Pain Med. 2003; 28:198–202.

6. Foxall G, McCahon R, Lamb J, Hardman JG, Bedforth NM. Levobupivacaine-induced seizures and cardiovascular collapse treated with Intralipid. Anaesthesia. 2007; 62:516–518.

7. Ok SH, Sohn JT, Baik JS, Kim JG, Park SS, Sung HJ, et al. Lipid emulsion reverses Levobupivacaine-induced responses in isolated rat aortic vessels. Anesthesiology. 2011; 114:293–301.

8. Baik JS, Sohn JT, Ok SH, Kim JG, Sung HJ, Park SS, et al. Levobupivacaine-induced contraction of isolated rat aorta is calcium dependent. Can J Physiol Pharmacol. 2011; 89:467–476.

9. Sung HJ, Choi MJ, Ok SH, Lee SH, Hwang IJ, Kim HS, et al. Mepivacaine-induced contraction is attenuated by endothelial nitric oxide release in isolated rat aorta. Can J Physiol Pharmacol. 2012; 90:863–872.

10. Li B, Yan J, Shen Y, Li B, Hu Z, Ma Z. Association of sustained cardiovascular recovery with epinephrine in the delayed lipid-based resuscitation from cardiac arrest induced by bupivacaine overdose in rats. Br J Anaesth. 2012; 108:857–863.

11. Harvey M, Cave G, Prince G, Lahner D. Epinephrine injection in lipid-based resuscitation from bupivacaine-induced cardiac arrest: transient circulatory return in rabbits. Anesth Analg. 2010; 111:791–796.

12. Liu L, Xia Y, Chen Y, Wang Q, Shi T, Wang F, et al. The comparative effects of lipid, epinephrine, and their combination in the reversal of bupivacaine-induced asystole in the isolated rat heart. Anesth Analg. 2012; 114:886–893.

13. Hiller DB, Gregorio GD, Ripper R, Kelly K, Massad M, Edelman L, et al. Epinephrine impairs lipid resuscitation from bupivacaine overdose: a threshold effect. Anesthesiology. 2009; 111:498–505.
14. Hollenberg SM. Vasoactive drugs in circulatory shock. Am J Respir Crit Care Med. 2011; 183:847–855.

15. Heavner JE, Pitkänen MT, Shi B, Rosenberg PH. Resuscitation from bupivacaine-induced asystole in rats: comparison of different cardioactive drugs. Anesth Analg. 1995; 80:1134–1139.
16. Ok SH, Bae SI, Shim HS, Sohn JT. Dexmedetomidine-induced contraction of isolated rat aorta is dependent on extracellular calcium concentration. Korean J Anesthesiol. 2012; 63:253–259.

17. Sung HJ, Ok SH, Sohn JY, Son YH, Kim JK, Lee SH, et al. Vasoconstriction potency induced by aminoamide local anesthetics correlates with lipid solubility. J Biomed Biotechnol. 2012; 2012:170958.

18. Cassidy SL, Lympany PA, Henry JA. Lipid solubility of a series of drugs and its relevance to fatal poisoning. J Pharm Pharmacol. 1988; 40:130–132.

19. Cox B, Durieux ME, Marcus MA. Toxicity of local anaesthetics. Best Pract Res Clin Anaesthesiol. 2003; 17:111–136.

20. Zapata-Sudo G, Trachez MM, Sudo RT, Nelson TE. Is comparative cardiotoxicity of S(-) and R(+) bupivacaine related to enantiomer-selective inhibition of L-type Ca(2+) channels? Anesth Analg. 2001; 92:496–501.

21. Sung HJ, Sohn JT, Park JY, Hwang EM, Baik JS, Ogawa K. Direct effect of ropivacaine involves lipoxygenase pathway activation in rat aortic smooth muscle. Can J Anaesth. 2009; 56:298–306.

22. Strichartz GR, Sanchez V, Arthur GR, Chafetz R, Martin D. Fundamental properties of local anesthetics. II. Measured octanol:buffer partition coefficients and pKa values of clinically used drugs. Anesth Analg. 1990; 71:158–170.
23. Ozcan MS, Weinberg G. Update on the use of lipid emulsions in local anesthetic systemic toxicity: a focus on differential efficacy and lipid emulsion as part of advanced cardiac life support. Int Anesthesiol Clin. 2011; 49:91–103.

24. Huang JM, Xian H, Bacaner M. Long-chain fatty acids activate calcium channels in ventricular myocytes. Proc Natl Acad Sci U S A. 1992; 89:6452–6456.

25. Weinberg GL. Lipid emulsion infusion: resuscitation for local anesthetic and other drug overdose. Anesthesiology. 2012; 117:180–187.
26. Waring WS. Intravenous lipid administration for drug-induced toxicity: a critical review of the existing data. Expert Rev Clin Pharmacol. 2012; 5:437–444.

27. Montiel V, Gougnard T, Hantson P. Diltiazem poisoning treated with hyperinsulinemic euglycemia therapy and intravenous lipid emulsion. Eur J Emerg Med. 2011; 18:121–123.

28. Groban L. Central nervous system and cardiac effects from long-acting amide local anesthetic toxicity in the intact animal model. Reg Anesth Pain Med. 2003; 28:3–11.

29. Santos AC, Arthur GR, Pedersen H, Morishima HO, Finster M, Covino BG. Systemic toxicity of ropivacaine during ovine pregnancy. Anesthesiology. 1991; 75:137–141.

30. Tanoubi I, Vialles N, Cuvillon P, Ripart J. [Systemic toxicity with mepivacaine following axillary block in a patient with terminal kidney failure]. Ann Fr Anesth Reanim. 2006; 25:33–35.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download