Abstract
Purpose
Our aim to assess clinical significance of the relation between inferior mesenteric vein ligation and collateral blood supply (meandering mesenteric artery) to the splenic flexure with elaboration more in anatomical landmarks and technical tips.
Materials and Methods
We review the literature regarding the significance of the collateral vessels around inferior mesenteric vein (IMV) root and provide our prospective operative findings, anatomical landmarks and technical tips. We analyzed the incidence and pattern of anatomic variation of collateral vessels around the IMV.
Results
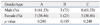
A total of 30 consecutive patients have been prospectively observed in a period between June 25-2012 and September 7-2012. Nineteen males and eleven females with mean age of 63 years. Major colorectal procedures were included. There were three anatomical types proposed, based on the relation between IMV and the collateral vessel. Type A and B in which either the collateral vessel crosses or runs close to the IMV with incidence of 43.3% and 13.3%, respectively, whereas type C is present in 43.3%. There was no definitive relation between the artery and vein. No intra or postoperative ischemic events were reported.
Conclusion
During IMV ligation, inadvertent ligation of Arc of Riolan or meandering mesenteric artery around the IMV root "in type A&B" might result in compromised blood supply to the left colon, congestion, ischemia and different level of colitis or anastomotic dehiscence. Therefore, careful dissection and skeletonization at the IMV root "before ligation if necessary" is mandatory to preserve the collateral vessel for the watershed area and to avoid further injury.
Colonic ischemia has been reported to be one of the most serious surgical complications and can lead to major morbidity and mortality. Different levels of ischemia might be noticed either during the operation or at the postoperative period. There are multiple factors which can lead to this circumstances, while technical ones must be addressed because it is preventable.
Our experience with colonic ischemia has recently been addressed by Park, et al.1 He reported 10 cases over a period of 5 years. He found that the only independent significant prognostic factor for ischemia was found to be cardiovascular disease. Anatomical and technical factors were not evaluated during that time.
Therefore, careful study of anatomy and ways of how to apply it in surgical practice is paramount in the prevention of ischemic events.
Variability of splenic flexure blood supply has been described in different ways among literatures: usually, venous drainage from the left colon and splenic flexure formed by several branches that join the inferior mesenteric vein (IMV). IMV is located close to the ligament of Treitz and passes below lower border of the pancreas to join the splenic vein. Moreover, IMV has variable ways of drainage. Usually, it drains into splenic vein, but it may directly join the superior mesenteric vein (SMV) or at the confluence between SMV and splenic vein (Fig. 1).2
There is no specifically distinct artery to splenic flexure, and anatomic variation and collateral pathways are common. In the usual situation, the inferior mesenteric artery (IMA) originates from left anterolateral aspect of the abdominal aorta around the L3-4 levels and supplies the colon from the mid-transverse portion to the rectum. Initially, the vessel has an inferior course of several centimeters and then yields to the left colic artery, which is the first or highest branch of the IMA, and travels adjacent to the inferior mesenteric vein. Usually, it runs upward and may reach the splenic flexure where it bifurcates in 85% of cases.3,4 The ascending branch of left colic artery makes anastomosis with the left branch of the middle colic artery in the splenic flexure region. The anastomotic branches close to the bowel named as an artery of Drummond.
Jean Riolan first described a tortuous collateral vessel so called arc of Riolan or meandering mesenteric artery, which is located centrally within the mesentery and forms a communication between the middle colic and left colic arteries in a region, where there are usually no major blood vessels. It is present in about 7-10% of population.4,5 Kachlik and Baca6 in his anatomical study found that the marginal artery in the left colic flexure forms an arch called Riolan's arcade or Haller's anastomosis in 95% of cases. Those collateral vessels suggested to be an enlargement of a normally existing collateral vessel due to occlusion of either the superior mesenteric artery (SMA) or IMA.7,8
Generally, the marginal artery is sufficient for left colic circulation after ligation of the IMA, however, patency of ascending branch of the left colic artery might be primordial at the splenic flexure.9
Variability of the collateral blood supply to the splenic flexure and its relation to the IMV make it a part of our concern during colorectal surgical procedure. Knowledge of their anatomy is prerequisite for surgeons to choose adequate techniques and to avoid injury to them.
Inferior mesenteric vein ligation is indicated in certain circumstances during low anterior resection (LAR) to gain more medial mobilization. Meandering mesenteric artery or arc of Riolan may cross the IMV at the lower border of the pancreas or run close to it before it goes toward splenic flexure. Ligation of the IMV at this level without careful attention to the collateral vessels can affect the splenic flexure blood supply and might lead to variable degrees of left colonic congestion and ischemia.
Our aim in this study is to assess clinical significance of the relation between inferior mesenteric vein ligation and collateral blood supply to the splenic flexure with more elaboration in anatomical landmarks and technical tips.
This is a prospective observational study. We assessed the anatomical blood supply around the IMV before ligation intra-operatively and attempted to provide our technical tips to preserve the blood supply to the splenic flexure.
We showed our operative pictures during IMV dissection and ligation in open, laparoscopic and robotic left colon and rectal resection at Severance Hospital Yonsei University College of Medicine. Literature review for postoperative colorectal ischemia was done through the PubMed and Google search website. SPSS system (Statistical Product and Service Solutions version 18 for Windows; SPSS Inc., Chicago, IL, USA) was used for calculation, and p value of 0.5 was considered significant.
Between June 25-2012 and September 7-2012, a total of 30 consecutive patients was prospectively and intraoperatively observed. Out of 30 patients; 19 were males and 11 females. The ages ranged between 42 and 83 years with mean age of 63.
Out of the 30 patients, 14 (46.6%) had LAR, 11 (36.6%) had anterior resection, 2 (6.6%) had total colectomy (TC), 2 (6.6%) had left colectomy and 1 (3.3%) had abdominoperineal resection. Operative technique included laparoscope in 19 patients (63.3%) and robotic procedure in 6 patients (20%). The remaining 5 patients (16.6%) received open procedure.
We observed that most of the collateral vessel was artery and vein run beside each other to supply the splenic flexure. Regardless of the name of those collateral vessels, we think that its location and relation to the inferior mesenteric vein are technically more important for colorectal surgical procedures.
The collateral vessel (meandering mesenteric artery or arc of Riolan) observed and classified around the IMV was as follows:
Type A: the artery emerges from the right side of the IMV, passes at the lower border of the pancreas, and crosses the inferior mesenteric vein at that level (Fig. 2).
Type B: the artery runs close to IMV until the lower border of the pancreas (Fig. 3).
Type C: no collateral artery related to the IMV (Fig. 4).
Type A and C were observed equally in 13 patients each (43.3%), while type B was observed in 4 patients (13.3%) (Fig. 5). Overall, we noticed that the IMV was related with collateral vessels in 17 patients (56.6%). No statistically significant gender-related anatomical type predominance was observed (Table 1).
In all cases, IMV ligation has been done with careful skeletonization, and we avoided injury to collateral vessels except 4 cases; 2 of them had TC and others had left hemicolectomy. No intra- or postoperative colonic ischemia has been noticed.
Understanding the anatomy and applying appropriate technique accordingly are mandatory for improving the quality of surgery and patient outcome. The arc of Riolan is an inconstantly situated artery, that courses medial to the mesenteric border of the colon, where it courses radially through the mid portion of the mesenteric arcade, near the inferior mesenteric vein.6 This vessel connects either superior and inferior mesenteric trunk or, more frequently, their branches in the mesentery, close to its root, never in its peripheral margin. It runs close to the inferior mesenteric vein, bending along the duodenojejunal flexure and traversing Treitz ligament anteriorly.
Left colic artery bifurcates mostly at Griffith's point (watershed area), which is located at splenic flexure where the left branch of the middle colic and ascending branch of left colic are joining together. This area receives a poor blood supply, and it is susceptible to damage and ischemia during surgical procedure. For this reason, considerable care must be taken not to disrupt the bifurcation of the left colic artery that replaces in a sense the function of the marginal artery in this area.2,10 In fact, a few authors describe more than one set of communications in the splenic flexure area. Moskowitz, et al.11 described the meandering artery of Moskowitz, which courses along the base of the colonic mesentery, and represents a connection between the proximal branch of the middle colic artery and the ascending branch of the left colic artery.4
Adding Villemin arcade to the Riolan and Drummond at the splenic flexure level has also been noticed by others,12 however, in our opinion it is the same artery of Mosckowitz with just different names.
Moreover, Pikkieff13 proposed the following types of communication between the IMA and SMA that forms the arc of Riolan:
1) connection between the accessory middle colic artery and the left colic artery-5.7%
2) communication between the middle colic artery and the left colic artery-3%
3) anastomosis between trunks of both mesenteric arteries-0.3%
4) vessel connecting superior mesenteric artery and left colic artery-0.3%
Discussion about different names and anatomic location of those vessels is somehow confusing. Gourley and Gering7 discussed more specific terminology of the collateral blood vessels to avoid the confusion, and concluded that the use of the vague historic term "arc of Riolan" should be discarded for more precise term "meandering mesenteric artery". However, clinical application for those collaterals is by far the corner stone for all surgical procedure.
Angiography is certainly a useful diagnostic tool to evaluate vascular patterns of the colon. However, Lin and Chaikof14 found that collateral vessels may not be clearly visible on angiography, however, these vessels might increase in size in response to an ischemic stimulus to increase the blood flow. Moreover, Horton and Fishman9 found that a 3 dimensions (3D) multi-detector row CT can provide a non-invasive accurate evaluation of mesenteric vasculature.
Some of the earliest studies concluded that the spatial resolution of 3D gadolinium-enhanced magnetic resonant angiography was too low for delineation and assessment of the small distal branches and inferior mesenteric artery. New magnetic resonant angiography (MRA) scanners equipped with stronger gradients and parallel imaging techniques can partially overcome this problem.15-17
Catheter angiography is still superior to CT angiography and 3D Gd-MRA because of its excellent in-plane spatial resolution of 0.3×0.3 mm2.2,18 In our opinion, a specific comparison studies between diagnostic modalities for better visualization of inferior mesenteric artery and its collateral vessels are still scarce in literature.
The incidence of colonic ischemia after ligation of the inferior mesenteric artery ranges between 0.45-24%,19-21 and Park, et al.1 reported to be 0.83%. However, the collateral vessels to the left colon area are clinically significant, and injury to those vessels has been reported to be a risk factor for vascular compromise during colorectal, vascular or other abdominal surgery.
Although it is uncommon among skillful surgeon, nevertheless, it is still reported by them, suggesting that the cause of ischemia and congestion is multifactorial and it may be due to medical, drugs or other surgical factors.22
The patients usually present with fever, tachycardia, abdominal pain, and bloody diarrhea. Depending on the site and type of anastomosis, patients can have either localized or generalized peritonitis. Passage of a full-thickness infarcted colonic segment (so-called "cast"), not accompanied by any features of acute peritonitis, is a very rare and might be a main advertising manifestation of acute colonic ischemia, and patients with colonic cast are diagnosed with subacute colonic ischemia several weeks after surgery.23,24
Leukocytosis and disturbed acid-base balance might be seen in the laboratory work up. Progression and deterioration to shock, especially in elderly, are common and can lead to serious morbidity and mortality. Strong clinical suspicion and radiological investigation such as CT scan and colonoscopy can confirm the diagnosis.
In the present study, we discussed the anatomical landmarks, which need to be recognized during colorectal procedure, especially at the time of IMV ligation. Based on the relation of the collateral vessel to the IMV, 3 types of classification have been proposed. Among them, type A and C are most common. The marginal artery of Drummond sometimes runs just medial to the IMV, especially in the case of short mesentery at the splenic flexure area.
In our surgical practice, we occasionally need to ligate the IMV at the lower border of the pancreas to gain more medial mobilization and tension-free anastomosis which is important to prevent vascular compromise and leak at the anastomotic site.
Our recommendations during IMV ligation to gain more medial mobilization at the level of the lower border of the pancreas are to carefully check the anatomy at that area. Therefore, we call this area "a critical zone of IMV". This zone is triangular in shape, formed by the IMV, lower border of the pancreas and the left colic artery (Fig. 6). This zone is not always empty, and might have a meandering mesenteric artery or arc of Riolan at the lower border of the pancreas (type A) or the collateral vessel runs very close to IMV (type B). Thus, skeletonization of the IMV at where you want to divide is recommended to exclude any adherent marginal or collateral vessels for type B (Fig. 3). The division of IMV for type A should be below the collateral artery (Fig. 2). If the arterial ligation at that level is mandatory, temporary clamp can be applied to the artery and assess the bowel color. If any changes occur, avoid the ligation as possible or modify your resection margin.
Our proposed technical tips for ligation of the IMV might be helpful during left colorectal procedures such as anterior or LAR in terms of preservation of collateral blood supply to the anastomotic area or stoma site.
In case of IMA ligation or left colic artery atherosclerosis, the splenic flexure will depend on the arc of Riolan or the arterial branch from the middle colic. If this is also injured at the lower border of the pancreas or during medial mobilization of the mesentery, you might have left colonic congestion or variable degrees of ischemia which might not be prominent or seen very well during the procedure, but might be seen postoperatively as an anastomotic failure, leak or stricture.
Parc, et al.25 found that the Riolan arcade dysfunction might be responsible for the high rate of digestive fistula after colocolic anastomosis subsequent to transverse colon resection, and Einstein, et al.26 also showed the significance of the collateral vessels and found that inadvertent ligation of the arc of Riolan during aortic or abdominal surgery in the setting of significant stenosis of the SMA, may result in necrosis of the left colon and small intestine. Indeed, a prominent artery often heralds underlying vascular occlusive disease that merits for investigation before the ligation of the IMA.
Retrograde flow from the IMA to the SMA through the arc of Riolan is the sign of SMA insufficiency, and the ligation of the IMA under these conditions could lead to proximal enteric ischemia.27
Not only the anastomotic site can be affected, but also the stoma integrity and vascularity. Indeed, Cima and Bilings27 concluded that the stoma circulation should not be based on the marginal artery of Drummond, which it might be narrow or absent at the splenic flexure.
After reviewing of literatures for the recommendations on how to deal with those collateral vessels, Sakorafas, et al.4 recommended that surgeons must abandon their plans for a major (high) mesenteric resection or the meandering mesenteric artery when the meandering mesenteric artery is discovered during left colon operation. Necrosis of the right colon and the entire small intestine may occur if the flow in the meandering mesenteric artery is retrograde i.e. IMA to SMA or it may cause necrosis of the sigmoid colon and upper rectum if the flow is antegrade i.e. SMA to IMA, especially if the left colic artery is not patent due to either atherosclerosis or exclusion for aneurysmal disease.4
Furthermore, Gourley and Gering7 recommend to routinely preserve the meandering mesenteric artery in all surgical procedures, including resection for cancer, thus providing its critical function in collateral mesenteric circulation.
Beside the arterial palpation and color assessment, laser Doppler flowmetry allows continuous and real-time measurement of anastomotic blood flow. It is also useful to predict a high-risk group for postoperative anastomotic ischemia, particularly in elderly male patients who undergo ultra low anterior resection.28 Along with advancement in robotic technology, the use of florescent camera and injection of indocyanine green is very helpful in identification of the vessels, especially in difficult cases where the plane around the vessels is not clear (Fig. 7). This careful assessment can help us determine the site of proximal resection margin.
Limitations: due to rare presentation of adverse vascular complications in colorectal surgery and our prospective caring about the collateral vessels at critical zone of IMV with this small sample size, we wereunable to determine the correlation between each type of collateral vessel and vascular complications rate. Nevertheless, this did not deter our aim to describetechnical and clinical recommendations and significance.
In conclusion, our preliminary observational study showed that a total of 56.6% of our patients have anatomical variations around the IMV. During IMV ligation, inadvertent ligation of arc of Riolan or meandering mesenteric artery around the IMV root "in type A&B" might result in compromised blood supply to the left colon, congestion, ischemia and different levels of colitis or anastomotic dehiscence.
Careful dissection and skeletonization at the IMV root "a critical zone of IMV" before ligation is mandatory to preserve the collateral vessel for the watershed area and to avoid further injury. Although a large number of observational cases are needed to verify the conclusion, this will not nonetheless affect the validity of our technical and clinical recommendations.
Figures and Tables
Fig. 1
Inferior mesenteric vein variations, 1) Drain at the confluence, 2) Drain at superior mesenteric vein, 3) Drain into splenic vein. PV, portal vein; SV, splenic vein; SMV, superior mesenteric vein; IMV, inferior mesenteric vein.

Fig. 2
Open view; type A class, 1) Collateral vessel crosses the inferior mesenteric vein at the lower of the pancreas, 2) IMV cut end, 3) Lower border of the pancreas, 4) Duodenum, 5) Aorta, 6) Cut end of the inferior mesenteric artery, 7) Left colic. IMV, inferior mesenteric vein.

Fig. 3
(A) Open view; type B; 1) Inferior mesenteric vein, 2) Arc of Riolan, 3) Dissection of starting point separates the artery from the vein, 4) Duodenum, 5) Pancreas. (B) laparoscopic view; type B; 1) Collateral artery (Arc of Riolan), 2) Inferior mesenteric vein, 3) Duodenum. (C) Laparoscopic view; type B; 1) Collateral artery (Arc of Riolan), 2) Inferior mesenteric vein, 3) Duodenum.

Fig. 4
Laparoscopic view; type C, 1) inferior mesenteric vein (IMV), 2) Duodenum, 3) Ligament of Treitz, 4) Pancreas. No arterial relation to IMV.

Fig. 6
Laparoscopic view demonstrates the critical zone of inferior mesenteric vein (IMV), showing that the arc of Riolan crosses the IMV at the lower border of the pancreas to the right side. Ligation of the IMV should be below the arc of Riolan.

ACKNOWLEDGEMENTS
Sami F. Al-Asari developed the idea for the study, designed the study, acquired the data, analyzed and interpreted the data, maintained the database, obtained follow-up data, wrote the manuscript, and critically reviewed/revised the manuscript. Daero Lim helped with data acquisition. Byung Soh Min collected the data. Nam Kyu Kim critically revised the manuscript for intellectual content.
References
1. Park MG, Hur H, Min BS, Lee KY, Kim NK. Colonic ischemia following surgery for sigmoid colon and rectal cancer: a study of 10 cases and a review of the literature. Int J Colorectal Dis. 2012; 27:671–675.

2. Netter Frank H.. Essentials Atlas of Human Anatomy. ISBN 0-914168-18-5 Copyright 1987.
3. Walker TG. Mesenteric vasculature and collateral pathways. Semin Intervent Radiol. 2009; 26:167–174.

4. Sakorafas GH, Zouros E, Peros G. Applied vascular anatomy of the colon and rectum: clinical implications for the surgical oncologist. Surg Oncol. 2006; 15:243–255.

5. Michels NA, Siddharth P, Kornblith PL, Parke WW. The variant blood supply to the descending colon, rectosigmoid and rectum based on 400 dissections. Its importance in regional resections: a review of medical literature. Dis Colon Rectum. 1965; 8:251–278.

6. Kachlik D, Baca V. Macroscopic and microscopic intermesenteric communications. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2006; 150:121–124.

7. Gourley EJ, Gering SA. The meandering mesenteric artery: a historic review and surgical implications. Dis Colon Rectum. 2005; 48:996–1000.

8. Rosenblum JD, Boyle CM, Schwartz LB. The mesenteric circulation. Anatomy and physiology. Surg Clin North Am. 1997; 77:289–306.
9. Horton KM, Fishman EK. Volume-rendered 3D CT of the mesenteric vasculature: normal anatomy, anatomic variants, and pathologic conditions. Radiographics. 2002; 22:161–172.

10. Bernstein WC, Bernstein EF. Ischemic ulcerative colitis following inferior mesenteric arterial ligation. Dis Colon Rectum. 1963; 6:54–61.

11. Moskowitz M, Zimmerman H, Felson B. The meandering mesenteric artery of the colon. Am J Roentgenol Radium Ther Nucl Med. 1964; 92:1088–1099.
12. Douard R, Chevallier JM, Delmas V, Cugnenc PH. Clinical interest of digestive arterial trunk anastomoses. Surg Radiol Anat. 2006; 28:219–227.

13. Pikkieff H. Über die Blutversorgung des Dickendarms. Zschr Anat Entw. 1931; 96:658–679.
14. Lin PH, Chaikof EL. Embryology, anatomy, and surgical exposure of the great abdominal vessels. Surg Clin North Am. 2000; 80:417–433.

15. Baden JG, Racy DJ, Grist TM. Contrast-enhanced three-dimensional magnetic resonance angiography of the mesenteric vasculature. J Magn Reson Imaging. 1999; 10:369–375.

16. Meaney JF. Non-invasive evaluation of the visceral arteries with magnetic resonance angiography. Eur Radiol. 1999; 9:1267–1276.

17. Shirkhoda A, Konez O, Shetty AN, Bis KG, Ellwood RA, Kirsch MJ. Mesenteric circulation: three-dimensional MR angiography with a gadolinium-enhanced multiecho gradient-echo technique. Radiology. 1997; 202:257–261.

18. Therasse E, Soulez G, Roy P, Gauvin A, Oliva VL, Carrier R, et al. Lower extremity: nonstepping digital angiography with photostimulable imaging plates versus conventional angiography. Radiology. 1998; 207:695–703.

19. Grinnell RS, Hiatt RB. Ligation of the interior mesenteric artery at the aorta in resections for carcinoma of the sigmoid and rectum. Surg Gynecol Obstet. 1952; 94:526–534.
20. Goligher JC. The adequacy of the marginal blood-supply to the left colon after high ligation of the inferior mesenteric artery during excision of the rectum. Br J Surg. 1954; 41:351–353.

21. Morgan CN, Griffiths JD. High ligation of the inferior mesenteric artery during operations for carcinoma of the distal colon and rectum. Surg Gynecol Obstet. 1959; 108:641–650.
22. Feldman M, Scharschmidt BF, Sleisenger MH. Sleisenger and Fordtran's: Gastrointestinal and liver Disease: Pathophysiology/Diagnosis/Management. 9th ed. Philadelphia: Saunders/Elsevier;2010.
23. Sakanoue Y, Kusunoki M, Shoji Y, Kusuhara K, Yamamura T, Utsunomiya J. Passage of a colon 'cast' after anoabdominal rectal resection. Report of a case. Dis Colon Rectum. 1990; 33:1044–1046.
24. Erguney S, Yavuz N, Ersoy YE, Teksoz S, Selcuk D, Ogut G, et al. Passage of "colonic cast" after colorectal surgery: report of four cases and review of the literature. J Gastrointest Surg. 2007; 11:1045–1051.

25. Parc R, Cugnenc PH, Levy E, Huguet C, Loygue J. [Early post-operative complications in intestinal resections followed with colo-colitic or recto-colitic anastomoses. Clinical and biological manifestations of anastomotic complications. Therapeutic results about 523 cases (author's transl)]. Ann Chir. 1981; 35:69–82.
26. Einstein AJ, McLaughlin MA, Lipman HI, Sanz J, Rajagopalan S. Images in vascular medicine the Arc of Riolan: diagnosis by magnetic resonance angiography. Vasc Med. 2005; 10:239.
27. Cima RR, Bilings B. Strategies to avoid 3 common problems in colorectal surgery. Contemp Surg. 2008; 64:120–125.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download