Abstract
Purpose
This study analyzed and evaluated the demographic, clinical, and cytogenetic data [G-banded karyotyping and array-based comparative genomic hybridization (array CGH)] of patients with unexplained developmental delay or intellectual disability at a single Korean institution.
Materials and Methods
We collected clinical and cytogenetic data based on retrospective charts at Ajou University Medical Center, Suwon, Korea from April 2008 to March 2012.
Results
A total of 190 patients were identified. Mean age was 5.1±1.87 years. Array CGH yielded abnormal results in 26 of 190 patients (13.7%). Copy number losses were about two-fold more frequent than gains. A total of 61.5% of all patients had copy number losses. The most common deletion disorders included 22q11.2 deletion syndrome, 15q11.2q12 deletion and 18q deletion syndrome. Copy number gains were identified in 34.6% of patients, and common diseases among these included Potocki-Lupski syndrome, 15q11-13 duplication syndrome and duplication 22q. Abnormal karyotype with normal array CGH results was exhibited in 2.6% of patients; theses included balanced translocation (n=2), inversion (n=2) and low-level mosaicism (n=1). Facial abnormalities (p<0.001) and failure to thrive were (p<0.001) also more frequent in the group of patients with abnormal CGH findings.
The prevalence of intellectual disability (ID) in Asian populations is estimated at 0.25-1.3%.1,2 ID and developmental delay (DD) affect not only the patients but also those around them including family and other community members. Consequently, ID/DD is an important issue in public health care. The causes of ID/DD are diverse and include various disorders that affect brain development and function. Although patients with ID/DD receive adequate care from primary care providers, the underlying cause of ID/DD remains poorly understood. Identification of underlying pathogenicity would permit better and more extensive support services, appropriate counseling, and anticipation of possible medical or behavioral complications. However, the proportion of ID/DD cases of unknown etiology is variously reported as 30-60%.3,4
Genetic testing by array-based comparative genomic hybridization (array CGH) has been widely implemented as a promising diagnostic method for patients with unexplained, non-syndromic ID/DD. Array CGH detects genome-wide chromosomal gains or/and losses by semi-quantitative ratio analysis, comparing a patient's DNA to reference DNA simultaneously hybridized to substrate-immobilized probes.5 Array CGH provides a much higher resolution than standard chromosomal karyotyping which cannot detect imbalances smaller than 5 Mb, and it enables identification of a greater number of genetic variations.6 Copy number variations (CNVs) are characterized as gains or losses in a genomic sequence greater than 1 kb and as alterations in the DNA of a genome. CNVs contribute significantly to genetic variability among different individuals and are increasingly recognized as a causal factor in human genomic disorders. Recent studies suggest that genomic CNVs are important in the etiology of neurodevelopmental disorders, including ID, DD, autism, schizophrenia, and other complex traits.7 The detection rate of pathogenic CNVs by array CGH has been reported as 15 to 20% in patients with unexplained ID/DD, which is substantially higher than that obtained with chromosomal karyotyping.8-11 In the present study, we analyzed demographic, clinical, and cytogenetic data (G-banded karyotyping and array CGH) from patients with unexplained DD/ID at a single institution in Korea.
We searched for all patients with unexplained DD or ID from Ajou University Medical Center, Suwon, Korea from April 2008 to March 2012. We included patients who underwent karyotyping and array CGH simultaneously. We excluded patients who exhibited abnormal results of previous metabolic, thyroid function or vision/hearing tests or who had been diagnosed with a brain tumor, brain infection, hypoxic-ischemic encephalopathy, neurocutaneous syndrome or clinically obvious chromosomal syndromes. Clinical data (birth history, family history of neurodevelopment diseases, growth charts, behavior problems, unprovoked seizure, morphologic abnormalities and major organ anomalies) and cytogenetic data (karyotype and array CGH) were collected based on retrospective chart reviews. Chromosome analysis was conducted with at least a 550-band resolution and described according to the International System for Human Cytogenetic Nomenclature 2009. Whole genome array CGH was performed using commercially available array CGH slides (MACArray Karyo 1440 BAC-chip, Macrogen, Seoul, Korea). The slides contained 1440 human bacterial artificial chromosome (BAC) clones including specific loci for more than 40 chromosomal disorders and 356 cell growth related genes from BAC libraries. Each BAC clone was spaced approximately 2.3 Mb on average across the entire genome and the range of each BAC clone size was 2,421-3,466,361 bp (average 121,708 bp). Each BAC clone was represented on an array as triplicate spots. All arrays were scanned using a GenePix4000B scanner (Axon Instruments, Foster City, CA, USA) and analyzed with array software (MAC VIEWER, Macrogen, Seoul, Korea). The position of the array targets were based on National Center for Biotechnology Information (NCBI) human genome build 37 (GRCh37/hg19; Feb. 2009). After detection of abnormalities by array CGH, we confirmed the microdeletions/duplications by fluorescence in situ hybridization (FISH). Ethical approval for this retrospective study was provided by the institutional review board of Ajou University Medical Center, Suwon, Korea (AJIRB-MED-MDB-12-136). Written informed consent was exempted by the board because this was a retrospective study.
A total of 190 (121 males and 69 females) patients, who fulfilled our criteria, were included in this study. The mean age was 5.1±1.87 (range, 0.34-32.0) years. Fifteen patients were small for gestational age. Postnatal failure to thrive (weight-for-age or height-for-age <3rd centile) was identified in 22 patients and overgrowth (weight-for-age or height-for-age >95th centile) in 6 patients. Eight patients had a family history of neurodevelopment disease. Thirty patients had a history of unprovoked seizures. Morphologic abnormalities12,13 were observed in 80 patients: microcephaly (head circumference <3rd centile) in 27, macrocephaly (head circumference >95th centile) in seven, brachycephaly in eight, dolichocephaly in three, plagiocephaly in two, cleft palate in six, facial abnormalities in 55, extremity abnormalities in 16, cryptorchidism in 11 and ambiguous genitalia in one patient. Behavioral problems were combined in 27 patients and included autistic features (n=15), aggressive behaviors (n=6), and hyperactive and attention deficit behaviors (n=6). Major organ anomalies were confirmed in 20 patients: congenital heart disease (n=19) and unilateral renal agenesis (n=1). Congenital heart diseases consisted of atrial septal defect (n=7), ventricular septal defect (n=6), patent ductus arteriosus (n=4), pulmonary stenosis (n=2), tetralogy of fallot, coarctation of the aorta, aortic stenosis, bicuspid aortic valve, and idiopathic hypertrophic subaortic stenosis (n=1, respectively). Demographic and clinical characteristics are summarized Table 1.
Array CGH yielded abnormal results in 26 of 190 patients (13.7%). Of the 26 patients with abnormal CGH, 10 patients (n=10/26, 38.5%) showed normal karyotype. The other 16 patients presented with array CGH results consistent with conventional karyotype analysis.
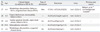
Sixteen patients (n=16/26, 61.5%) exhibited a heterozygous loss (deletion): 22q11.2 deletion syndrome (n=4), Angelman syndrome (n=3), 18q deletion syndrome (n=2), Williams-Beuren syndrome, Smith-Magenis syndrome, Wolf-Hirschhorn syndrome, 18p deletion syndrome, 3p deletion syndrome, 2q deletion and 13q deletion (n=1, respectively). Patients 5, 6, and 7 were diagnosed with Angelman syndrome, with a 2.06-Mb deletion of 15q1.2-q12. Heterozygous gains were identified in 8 patients (34.6%): Potocki-Lupski syndrome (n=2), 15q11-13 duplication syndrome (n=2), duplication 22q (n=2), Cat Eye syndrome, duplication 13q and Klinefelter syndrome (n=1, respectively). Patient 17 showed simultaneous deletion of Xp22.31 and duplication of Yq11.2. These abnormal karyotype findings are summarized in Table 2.
Abnormal karyotype with normal array CGH was exhibited in 5 patients: balanced translocation (n=2), inversion (n=2) and low-level mosaicism (n=1). These abnormalities are summarized in Table 3.
Morphologic abnormalities were significantly more frequent (p<0.001) in patients with abnormal array CGH than in patients with normal array CGH results. Facial abnormalities (p<0.001) were also more frequent in the group with abnormal CGH. The other morphologic abnormalities, including microcephaly (p=0.430), cleft palate (p=0.155), and extremity abnormalities (p=0.622), showed no significant difference between the two groups. Failure to thrive (p=0.005) was more frequent in patients with abnormal CGH. No statistically significant differences were found for being small for gestational age (p=0.458), family history of neurodevelopment disease (p=0.649), overgrowth (p=0.180), behavioral problems (p=0.854), unprovoked seizure (p=0.570) and congenital heart disease (p=0.091).
All parents of the patients who had abnormal array CGH results had normal phenotype. Cytogenetic analysis of the parents was not performed, except for the parents of patient 18 (de novo), because most of the parental samples were not available.
Genetic tests are recommended for unexplained ID/DD as they can provide diagnostic and prognostic information and allow precise genetic counseling for families with an affected child. For decades, G-banded karyotyping has been the standard first-tier test for detection of genetic imbalance. In recent years, clinical evidence supporting the use of array CGH for unexplained ID/DD has increased and array CGH is now commercially available in the clinical setting.8 Array CGH provides a remarkably higher resolution compared to conventional karyotyping, revealing submicroscopic deletions and duplications.14-16 Several studies anticipate that array CGH will become a routine method in patients with ID/DD, replacing routine karyotyping.8,11,17 The present study, for first time at a single institute in Korea, evaluated the diagnostic yield of array CGH in patients with unexplained ID/DD.
A meta-analysis of 33 studies on patients with ID, autism spectrum disorders, or multiple congenital anomalies indicated an average diagnostic yield for array CGH of 12%.18 In our study, the rate of abnormal findings was 13.7% and this appeared to be consistent with previous studies.4,8,19,20 Morphologic abnormalities, especially facial abnormalities, and failure to thrive were significantly more frequent in patients with abnormal array CGH than in patients with normal array CGH. Therefore, we discerned that patients with ID/DD accompanied by facial abnormalities or failure to thrive would generate a higher diagnostic value for array CGH.
In this study, we also perceived that copy number losses were about twice as frequent as gains; losses were identified in 61.5% and gains in 34.6% of patients. Because most copy number changes arise by non-allelic homologous recombination (NAHR), both loss and gain events arising from NAHR should occur at similar rates theoretically. However, microdeletion syndromes have been reported more often than microduplication syndromes in patient groups with ID/DD clinically. Several possibilities might explain why copy number losses are detected more often than gains in patients with ID/DD. Horev, et al.21 advocated that deletions exerted a more severe effect than duplications on phenotype, including viability, brain structure, and behavior, in mice. Moreover, Shchelochkov, et al.22 reported that microduplications show milder phenotypes such as subtle dysmorphic facial features, internal organ anomalies, and neuropsychological abnormalities than microdeletions in humans. In this context, we also identified more copy number losses than gains. We agree with previous reports that gains are clinically under-diagnosed due to relatively milder or absent ID/DD. Although ID/DD patients with mild phenotypes may be under-diagnosed, array CGH can help doctors to identify and elucidate cytogenetic abnormalities, increasing the diagnostic yield thereof.
In our study, patients 5, 6 and 7 had gene dosage changes of 2.06 Mb size on chromosome 15. Only one patient, patient 5, showed abnormal results in karyotyping, even at the same resolution. Standard karyotyping can only detect large chromosomal aberrations over 5-10 Mb in size, and fails to detect small regions of amplification or deletion. In addition, interpretation of a karyotype is labor intensive and highly dependent upon the experience and skill of the cytogeneticist. Array CGH provides a relatively high throughput and highly automated data interpretation, and requires no hands-on work per sample after initiation of the assay run. Therefore, we consider that chromosomal genetic testing with array CGH has additional merits as a diagnostic method, when compared with G-banded karyotyping, only in patients with unexplained ID.
On the other hand, an abnormal karyotype with normal array CGH was found in 2.6% (n=5/190) of patients in this study: balanced translocation (n=2), inversion (n=2) and low-level mosaicism of trisomy 14 (n=1). The inability of array CGH to detect balanced structural abnormalities is well known. One patient (patient 27) showed low-level mosaicism (estimated percentage of mosaicism was 23.3%) of trisomy 14 confirmed by karyotyping, but this was not detected by array CGH alone. The ability of array CGH to detect low-level mosaicism is not completely known. Based on a literature review, array CGH is unable to detect abnormal cell mosaicism at a frequency below 20-30%.23 Although the association of these chromosome structural changes and low-level gene dosage changes with abnormal phenotypes is controversial, this is important information for genetic counseling. Karyotyping is still a useful tool for supplementing the limitations of array CGH technology.
As we mentioned previously, CNVs have been shown to be associated with a wide variety of developmental and neurocognitive syndromes. Although array CGH has several limitations, it is sufficiently precise that clinical implementation of array CGH provides additional information on causative genetic diseases in patients with unexplained DD or ID. We also expect that array CGH, complemented by karyotype analysis, would be a useful diagnostic tool in selected patient groups, especially those with ID/DD combined with craniofacial anomaly or failure to thrive.
Figures and Tables
Table 2
Results of Abnormal Array CGH

DD, developmental delay; ID, intellectual disability; TOF, tetralogy of fallot; SGA, small for gestational age; FTT, failure to thrive; PS, pulmonary stenosis; PDA, patent ductus arteriosus; ADHD, attention deficit hyperactivity disorder; ASD, atrial septal defect; BAV, bicuspid aortic valve; CGH, comparative genomic hybridization.
*Siblings.
References
1. Jeevanandam L. Perspectives of intellectual disability in Asia: epidemiology, policy, and services for children and adults. Curr Opin Psychiatry. 2009; 22:462–468.

2. Kwok HW, Chui EM. A survey on mental health care for adults with intellectual disabilities in Asia. J Intellect Disabil Res. 2008; 52:996–1002.

3. Croen LA, Grether JK, Selvin S. The epidemiology of mental retardation of unknown cause. Pediatrics. 2001; 107:E86.

4. Rauch A, Hoyer J, Guth S, Zweier C, Kraus C, Becker C, et al. Diagnostic yield of various genetic approaches in patients with unexplained developmental delay or mental retardation. Am J Med Genet A. 2006; 140:2063–2074.

5. Shaffer LG, Bejjani BA. Medical applications of array CGH and the transformation of clinical cytogenetics. Cytogenet Genome Res. 2006; 115:303–309.

6. Oostlander AE, Meijer GA, Ylstra B. Microarray-based comparative genomic hybridization and its applications in human genetics. Clin Genet. 2004; 66:488–495.

7. Lee C, Iafrate AJ, Brothman AR. Copy number variations and clinical cytogenetic diagnosis of constitutional disorders. Nat Genet. 2007; 39:7 Suppl. S48–S54.

8. Miller DT, Adam MP, Aradhya S, Biesecker LG, Brothman AR, Carter NP, et al. Consensus statement: chromosomal microarray is a first-tier clinical diagnostic test for individuals with developmental disabilities or congenital anomalies. Am J Hum Genet. 2010; 86:749–764.

9. Stankiewicz P, Beaudet AL. Use of array CGH in the evaluation of dysmorphology, malformations, developmental delay, and idiopathic mental retardation. Curr Opin Genet Dev. 2007; 17:182–192.

10. D'Amours G, Kibar Z, Mathonnet G, Fetni R, Tihy F, Désilets V, et al. Whole-genome array CGH identifies pathogenic copy number variations in fetuses with major malformations and a normal karyotype. Clin Genet. 2012; 81:128–141.
11. Shoukier M, Klein N, Auber B, Wickert J, Schröder J, Zoll B, et al. Array CGH in patients with developmental delay or intellectual disability: are there phenotypic clues to pathogenic copy number variants? Clin Genet. 2013; 83:53–65.

12. Klinger G, Merlob P. Elements of morphology: standard terminology for the ear--additional features. Am J Med Genet A. 2009; 149A:1606.

13. Merks JH, van Karnebeek CD, Caron HN, Hennekam RC. Phenotypic abnormalities: terminology and classification. Am J Med Genet A. 2003; 123A:211–230.

14. Shaffer LG, Bejjani BA, Torchia B, Kirkpatrick S, Coppinger J, Ballif BC. The identification of microdeletion syndromes and otherchromosome abnormalities: cytogenetic methods of the past, new technologies for the future. Am J Med Genet C Semin Med Genet. 2007; 145C:335–345.
15. Dale RC, Grattan-Smith P, Nicholson M, Peters GB. Microdeletions detected using chromosome microarray in children with suspected genetic movement disorders: a single-centre study. Dev Med Child Neurol. 2012; 54:618–623.

16. Kurian MA. The clinical utility of chromosomal microarray in childhood neurological disorders. Dev Med Child Neurol. 2012; 54:582–583.

17. Wincent J, Anderlid BM, Lagerberg M, Nordenskjöld M, Schoumans J. High-resolution molecular karyotyping in patients with developmental delay and/or multiple congenital anomalies in a clinical setting. Clin Genet. 2011; 79:147–157.

18. Park SJ, Jung EH, Ryu RS, Kang HW, Ko JM, Kim HJ, et al. Clinical implementation of whole-genome array CGH as a first-tier test in 5080 pre and postnatal cases. Mol Cytogenet. 2011; 4:12.

19. Shen Y, Irons M, Miller DT, Cheung SW, Lip V, Sheng X, et al. Development of a focused oligonucleotide-array comparative genomic hybridization chip for clinical diagnosis of genomic imbalance. Clin Chem. 2007; 53:2051–2059.

20. Zahir F, Friedman JM. The impact of array genomic hybridization on mental retardation research: a review of current technologies and their clinical utility. Clin Genet. 2007; 72:271–287.

21. Horev G, Ellegood J, Lerch JP, Son YE, Muthuswamy L, Vogel H, et al. Dosage-dependent phenotypes in models of 16p11.2 lesions found in autism. Proc Natl Acad Sci U S A. 2011; 108:17076–17081.

22. Shchelochkov OA, Cheung SW, Lupski JR. Genomic and clinical characteristics of microduplications in chromosome 17. Am J Med Genet A. 2010; 152A:1101–1110.

23. Ballif BC, Hornor SA, Sulpizio SG, Lloyd RM, Minier SL, Rorem EA, et al. Development of a high-density pericentromeric region BAC clone set for the detection and characterization of small supernumerary marker chromosomes by array CGH. Genet Med. 2007; 9:150–162.

24. Huang C, Yang YF, Yin N, Chen JL, Wang J, Zhang H, et al. Congenital heart defect and mental retardation in a patient with a 13q33.1-34 deletion. Gene. 2012; 498:308–310.

26. Peeters H, Vermeesch J, Fryns JP. A cryptic duplication 22q13.31 to qter leads to a distinct phenotype with mental retardation, microcephaly and mild facial dysmorphism. Genet Couns. 2008; 19:365–371.
27. Machado IN, Heinrich JK, Campanhol C, Rodrigues-Peres RM, Oliveira FM, Barini R. Prenatal diagnosis of a partial trisomy 13q (q14-->qter): phenotype, cytogenetics and molecular characterization by spectral karyotyping and array comparative genomic hybridization. Genet Mol Res. 2010; 9:441–448.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download