Abstract
Purpose
Factor XIII (FXIII), a thrombin-activated plasma transglutaminase zymogen, is involved in cancer development and progression through a triggered coagulation pathway. The aim of this study was to examine whether FXIII activity levels differed in non-small cell lung cancer (NSCLC) patients according to histological types and TNM stage when compared with healthy subjects.
Materials and Methods
Twenty-eight NSCLC patients and 28 normal controls who had been individually age-, gender-, body mass index-, smoking status-, and smoking amount-matched were enrolled: 13 adenocarcinomas, 11 squamous cell carcinomas, and four undifferentiated NSCLCs; four stage I, two stage II, 12 stage III, and 10 stage IV NSCLCs. FXIII activity was measured using fluorescence-based protein arrays.
Results
The median FXIII activity level of the NSCLC group [24.2 Loewy U/mL, interquartile range (IQR) 14.9-40.4 Loewy U/mL] was significantly higher than that of the healthy group (17.5 Loewy U/mL, IQR 12.6-26.4 Loewy U/mL) (p=0.01). There were no differences in FXIII activity between adenocarcinoma (median 18.6 Loewy U/mL) and squamous cell carcinoma (median 28.7 Loewy U/mL). NSCLC stage significantly influenced FXIII activity (p=0.02). The FXIII activity of patients with stage III NSCLC (median 27.3 Loewy U/mL, IQR 19.3-40.5 Loewy U/mL) was significantly higher than those of patients with stage I or II (median 14.0 Loewy U/mL, IQR 13.1-23.1 Loewy U/mL, p=0.04). FXIII activity was negatively correlated with aPTT in NSCLC patients (r=-0.38, p=0.04).
Lung cancer is the primary cause of cancer-related mortality worldwide.1 Non-small cell lung cancer (NSCLC) accounts for about 75% of all lung cancer cases.2 Despite recent therapeutic advances in NSCLC, the overall 5-year survival is only around 15% for all stages.1 The main reason for treatment failure is delayed diagnosis, as the disease has often already achieved local advanced or metastatic phases by the time it is detected.3 Currently, there are no validated biomarkers for early lung cancer detection and tumor progression. Thus, the investigation of detective biomarkers has garnered great attention in lung cancer research.4,5
Coagulation factors participate in inflammatory responses and tumorigenic conditions. About 50% of all cancer patients and 90% of patients with metastases show coagulation abnormalities of different levels,6 and antithrombotic therapy has been reported to prolong survival time among patients with small cell lung cancer.7 Additionally, coagulation factors have been shown to promote tumor cell growth, invasion, metastasis, and angiogenesis;8 moreover, coagulation abnormalities have been suggested as affecting tumor dissemination via multiple mechanisms.9,10
Factor XIII (FXIII), including fibrinogen and fibrin, contribute to the final step in the coagulation cascade. FXIII, also known as fibrin stabilizing factor, is a member of the transglutaminase family,11 and is purported to exert anti-apoptotic effects on endothelial cells and promote angiogenic activity.11 Active FXIII catalyzes the formation of covalent cross links between γ-glutamyl and ε-lysyl residues of adjacent fibrin monomers, mechanically strengthening fibrin and protecting the newly formed fibrin network from destruction by the powerful fibrinolytic process.12 Since several FXIII substrates such as fibronectin and fibrinogen are known to be important in tumor stroma formation and metastasis,13-15 it has been suggested that FXIII activity may also be important in tumor development and metastasis. Accordingly, many clinical studies have reported the association of FXIII with human malignancies, including oral cancer,16 hepatocellular carcinoma,17 ovarian cancer,6 and leukemia.18 However, the role of FXIII in NSCLC has not yet been studied.
The purpose of this study was to compare FXIII activity in NSCLC patients with that in matched healthy subjects, and to determine whether there are differences in FXIII activity level according to histological type and TNM stage.
The NSCLC patients were prospectively enrolled at Korea University Ansan Hospital from September 2009 to March 2010. NSCLC was diagnosed through biopsies of primary lesions in patients with abnormalities on plain chest radiography and chest computed tomography scans. The stages of lung cancer were determined according to the National Comprehensive Cancer Network guidelines.19 As a healthy control group, age-, gender-, body mass index (BMI)-, smoking status-, and smoking amount-matched subjects were selected among participants in the Korean Health and Genome Study (KHGS), an ongoing population-based prospective cohort study that has been conducted since 2001.20 Participants with histories of cancer in other organs, coagulopathy, diabetes mellitus, dyslipidemia, cardiovascular disease, or any medications were excluded. The study protocol was approved by the institutional review board of the Korea University Ansan Hospital and informed consent was obtained from all study participants.
Plasma samples were collected from NSCLC patients and healthy subjects, and stored at -80℃. The FXIII activity assay was performed using fluorescence-based protein arrays. To fabricate the fibrinogen arrays, well-type amine arrays were incubated with fibrinogen. Reaction mixtures were prepared in a solution containing CaCl2, thrombin and plasma. An aliquot of the reaction mixture was then applied to each of the array wells. After washing, FXIII-catalyzed cross-linking of biotinamido pentylamine and fibrin were probed with Cy3-conjugated streptavidin. The arrays were dried and scanned with a fluorescence scanner using a 543 nm laser (ScanArray Express, PerkinElmer Life and Analytical Sciences, Boston, MA, USA). The fluorescence intensity of array spots measured with the ScanArray Express program was representative of the FXIII activity in each sample. The FXIII activity was expressed as Loewy unit per milliliter (Loewy U/mL).21
Differences in baseline characteristics between NSCLC patients and healthy subjects were analyzed using the Mann-Whitney test and presented as median and interquartile ranges (IQR). In subgroup analysis, the associations between FXIII activities and cell types or stages of NSCLC were analyzed by Kruskal-Wallis ANOVA. FXIII activities between two groups were compared using Mann-Whitney tests. We calculated Pearson correlation coefficients for estimating relationships between variables. All tests were two-sided, and differences of p<0.05 were considered statistically significant. SPSS software version 12.0 (Statistical Package for Social Sciences, Chicago, IL, USA) was used for all statistical analyses.
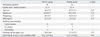
Table 1 presents the baseline characteristics of the participants. The mean age of the 28 NSCLC patients was 64.4 years; 22 (78.6%) were male. There were no significant differences in age, gender, height, weight, BMI, smoking status and smoking amount between the NSCLC and healthy group. The histological types and stages of the NSCLC group are as follows: 13 adenocarcinomas, 11 squamous cell carcinomas, and four undifferentiated carcinomas; four stage I, two stage II, 12 stage III, and 10 stage IV NSCLCs (Table 2). The median activated prothromboplastin time (aPTT) was 29.0 second (normal range: 30-47 seconds).
The median FXIII activity level of the NSCLC group (24.2 Loewy U/mL, IQR 14.9-40.4 Loewy U/mL) was significantly higher than that of the healthy group (17.5 Loewy U/mL, IQR 12.6-26.4 Loewy U/mL) (p=0.01) (Table 1).
FXIII activity in patients with squamous cell carcinoma (median 28.7 Loewy U/mL, IQR 20.3-42.2 Loewy U/mL) was significantly higher than in the healthy group (median 17.5 Loewy U/mL, IQR 12.6-26.4 Loewy U/mL, p=0.01) (Fig. 1). However, there were no differences in FXIII activity between the healthy group and patients with adenocarcinoma (median 18.6 Loewy U/mL, IQR 13.4-26.9 Loewy U/mL) (p=0.38) and between the patients with adenocarcinoma and squamous cell carcinoma (p=0.12). In addition, there were no differences in FXIII activity between patients with adenocarcinoma and those with squamous cell carcinoma of stages I-IIIa (median 14.00 vs. median 26.10, p=0.17) and of stages IIIb-IV (median 24.78 vs. median 28.69, p=0.35).
In the analysis based on TNM stages of NSCLC, FXIII activities were significantly different among the healthy group and patients of different NSCLC stage (p=0.02, by Kruskal-Wallis test). FXIII activity in patients with stage III NSCLC (median 27.3 Loewy U/mL, IQR 19.3-40.5 Loewy U/mL) was significantly higher than that in both the healthy group (median 17.5 Loewy U/mL, IQR 12.6-26.4 Loewy U/mL, p=0.01) and the patients with stage I or II NSCLC (median 14.0 Loewy U/mL, IQR 13.1-23.1 Loewy U/mL, p=0.04) (Fig. 2). FXIII activity in patients with stage IV NSCLC (median 26.4 Loewy U/mL, IQR 16.8-55.2 Loewy U/mL) was significantly higher than that of the healthy group (p=0.03). However, there were no differences in FXIII activity between the patients with stage IV NSCLC and the patients with stage III NSCLC, or between the patients with stage IV NSCLC and patients with stages I or II NSCLC. Also, there was no significant difference in FXIII activity in separate analysis according to T stage, N stage, or M stage, respectively.
FXIII activity was negatively correlated with aPTT in NSCLC patients (Fig. 3), but not with prothrombin time (PT). There was moderate negative correlation between FXIII activity and aPTT, in which the correlation coefficient was -0.38 (p=0.04) in itself, and -0.48 (p=0.03) when adjusted with PT.
The results of this study showed that FXIII activity was higher in patients with NSCLC than in the healthy group. Patients with squamous cell carcinoma and stage III and IV disease showed significantly higher FXIII activities than those of the healthy group. Additionally, FXIII activity was higher in patients with stage III disease than in patients with stages I or II. Moreover, FXIII activity was negatively correlated with aPTT in NSCLC patients.
Coagulation abnormalities have been suggested to influence tumor dissemination via multiple mechanisms.9,10 The inhibition of coagulation factors, including FXIII, have been reported to decrease metastatic progression.22,23 In a previous study, elevated plasma fibrinogen was positively correlated with tumor size, advanced stage and squamous cell type of NSCLC.15 Additionally, abnormal prothrombin time, higher platelet count, fibrinogen and D-dimer were all shown to be associated with poor prognosis in NSCLC.24 Approximately 90% of cancer patients with metastasis and half of all cancer patients have abnormal coagulation parameters, including shortened aPTT and increased levels of other related coagulation factors.25 Our results validated the relationship between coagulation factor levels and measured coagulation testing. FXIII is a heterotetramer that consists of two globular A subunits and two strand like B subunits.26 FXIII is responsible for the formation of fibrin in the final stage of coagulation cascade,27 and participates in hemostasis, angiogenesis, wound healing and maintenance of pregnancy.28 The levels of FXIII-A subunit, which are converted from FXIII, are usually higher in females, elderly patients, and smokers.28 Therefore, in our study, 28 NSCLC patients were compared with individually age-, gender-, BMI-, smoking status-, and smoking amount-matched healthy subjects.
Studies of FXIII activity in tumor biology are scarce. FXIII has been shown to support metastasis primarily by limiting NK cell-mediated clearance of micrometastatic tumor cells through cross-linking fibrin,22 which is also supposed to function as a promoter for stable adhesion for early metastasis.14 FXIII also plays an important role in tumor angiogenesis by direct stimulation of endothelial cell proliferation, migration and survival.11 In this study of NSCLC, FXIII activity in patients with advanced stage disease was significantly higher than that in patients with earlier stage disease, which was consistent with a previous study regarding the potential role of FXIII in tumor biology.11,14 The reasons for the increased FXIII activities are supposed to be due to increased FXIII-A secretion from damaged tumor-associated macrophages and increased vascular permeability factor/vascular endothelial growth factor (VEGF), which is a key element for angiogenesis and coagulation/fibrinolysis activation.29 This phenomenon was predominant in squamous cell carcinoma rather than in adenocarcinoma, according to a previous report.30 Considering our results, FXIII activity may be a potential novel biomarker for NSCLC, and further investigations are necessary to reveal the effect of FXIII activity on cell type, progression, and prognosis in NSCLC patients. However, there are some contradictions with the reports in patients with breast cancer31 and advanced gastrointestinal tumors,32 as these patients had reduced FXIII levels.
There are some limitations to the present study. First, the sample size was small. In order to match age, gender, BMI, smoking status, and smoking amount and exclude factors which could potentially influence FXIII activity, a limited number of NSCLC patients and participants from KHGS were enrolled. Therefore, it was impossible to perform subgroup analysis of undifferentiated cell types or make comparisons with other cell types. Second, because this was a cross-sectional study, the effect of FXIII activity on prognosis could not be evaluated. Finally, the relationship of other coagulation factors such as fibrinogen and D-dimer were not analyzed.
In conclusion, FXIII activity in NSCLC patients and patients with advanced stages was significantly increased compared to those of strictly matched healthy subjects and patients with earlier stages of disease, respectively. These findings suggest potential roles for FXIII in NSCLC progression. Therefore, further studies with larger sample sizes are necessary to investigate the role of FXIII in lung cancer biology.
Figures and Tables
 | Fig. 1FXIII activities were significantly different among the healthy, adenocarcinoma, and squamous cell carcinoma groups (p=0.03). FXIII activity in squamous cell carcinoma (median 28.7 Loewy U/mL, IQR 20.3-42.2 Loewy U/mL) was significantly higher than that in the healthy group (median 17.5 Loewy U/mL, IQR 12.6-26.4 Loewy U/mL, p=0.01), but there were no differences between adenocarcinoma (median 18.6 Loewy U/mL, IQR 13.4-26.9 Loewy U/mL) and squamous cell carcinoma. Comparisons were performed using Kruskal-Wallis and Mann-Whitney tests. FXIII, factor XIII; Adeno, adenocarcinoma; Squamous, squamous cell carcinoma; IQR, interquartile range. |
 | Fig. 2TNM stage of NSCLC significantly influenced FXIII activity (p=0.02). FXIII activity in patients with stage III NSCLC (median 27.3 Loewy U/mL, IQR 19.3-40.5 Loewy U/mL) was significantly higher than that in both the healthy controls (median 17.5 Loewy U/mL, IQR 12.6-26.4 Loewy U/mL, p=0.01) and the patients with stage I or II disease (median 14.0 Loewy U/mL, IQR 13.1-23.1 Loewy U/mL, p=0.04). FXIII activity in patients with stage IV NSCLC (median 26.4 Loewy U/mL, IQR 16.8-55.2 Loewy U/mL) was significantly higher than that in the healthy group. Comparisons were performed using Kruskal-Wallis tests and Mann-Whitney tests. NSCLC, non-small cell lung cancer; FXIII, factor XIII; IQR, interquartile range. |
 | Fig. 3aPTT and FXIII activity showed a significant correlation in NSCLC patients (r=-0.38, p=0.04). aPTT, activated prothromboplastin time; FXIII, factor XIII; NSCLC, non-small cell lung cancer. |
References
1. Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol. 2006; 24:2137–2150.

4. Coate LE, John T, Tsao MS, Shepherd FA. Molecular predictive and prognostic markers in non-small-cell lung cancer. Lancet Oncol. 2009; 10:1001–1010.

5. Montuenga LM, Pio R. Current challenges in lung cancer early detection biomarkers. Eur J Cancer. 2009; 45:Suppl 1. 377–378.

6. Wang X, Wang E, Kavanagh JJ, Freedman RS. Ovarian cancer, the coagulation pathway, and inflammation. J Transl Med. 2005; 3:25.

7. Kakkar AK, Levine MN, Kadziola Z, Lemoine NR, Low V, Patel HK, et al. Low molecular weight heparin, therapy with dalteparin, and survival in advanced cancer: the fragmin advanced malignancy outcome study (FAMOUS). J Clin Oncol. 2004; 22:1944–1948.

8. Sampson MT, Kakkar AK. Coagulation proteases and human cancer. Biochem Soc Trans. 2002; 30:201–207.

9. Camerer E, Qazi AA, Duong DN, Cornelissen I, Advincula R, Coughlin SR. Platelets, protease-activated receptors, and fibrinogen in hematogenous metastasis. Blood. 2004; 104:397–401.

10. Palumbo JS, Kombrinck KW, Drew AF, Grimes TS, Kiser JH, Degen JL, et al. Fibrinogen is an important determinant of the metastatic potential of circulating tumor cells. Blood. 2000; 96:3302–3309.

11. Dardik R, Loscalzo J, Inbal A. Factor XIII (FXIII) and angiogenesis. J Thromb Haemost. 2006; 4:19–25.

12. Katona E, Nagy B, Kappelmayer J, Baktai G, Kovács L, Márialigeti T, et al. Factor XIII in bronchoalveolar lavage fluid from children with chronic bronchoalveolar inflammation. J Thromb Haemost. 2005; 3:1407–1413.

14. Palumbo JS, Potter JM, Kaplan LS, Talmage K, Jackson DG, Degen JL. Spontaneous hematogenous and lymphatic metastasis, but not primary tumor growth or angiogenesis, is diminished in fibrinogen-deficient mice. Cancer Res. 2002; 62:6966–6972.
15. Jones JM, McGonigle NC, McAnespie M, Cran GW, Graham AN. Plasma fibrinogen and serum C-reactive protein are associated with non-small cell lung cancer. Lung Cancer. 2006; 53:97–101.

16. Vairaktaris E, Vassiliou S, Yapijakis C, Spyridonidou S, Vylliotis A, Derka S, et al. Increased risk for oral cancer is associated with coagulation factor XIII but not with factor XII. Oncol Rep. 2007; 18:1537–1543.

17. An Y, Bekesova S, Edwards N, Goldman R. Peptides in low molecular weight fraction of serum associated with hepatocellular carcinoma. Dis Markers. 2010; 29:11–20.

18. Kiss F, Hevessy Z, Veszprémi A, Katona E, Kiss C, Vereb G, et al. Leukemic lymphoblasts, a novel expression site of coagulation factor XIII subunit A. Thromb Haemost. 2006; 96:176–182.

19. Rami-Porta R, Crowley JJ, Goldstraw P. The revised TNM staging system for lung cancer. Ann Thorac Cardiovasc Surg. 2009; 15:4–9.
20. Kim SJ, Suk MH, Choi HM, Kimm KC, Jung KH, Lee SY, et al. The local prevalence of COPD by post-bronchodilator GOLD criteria in Korea. Int J Tuberc Lung Dis. 2006; 10:1393–1398.
21. Kwon MH, Kong DH, Jung SH, Suh IB, Kim YM, Ha KS. Rapid determination of blood coagulation factor XIII activity using protein arrays for serodiagnosis of human plasma. Anal Chem. 2011; 83:2317–2323.

22. Palumbo JS, Barney KA, Blevins EA, Shaw MA, Mishra A, Flick MJ, et al. Factor XIII transglutaminase supports hematogenous tumor cell metastasis through a mechanism dependent on natural killer cell function. J Thromb Haemost. 2008; 6:812–819.

23. Bobek V, Kovarík J. Antitumor and antimetastatic effect of warfarin and heparins. Biomed Pharmacother. 2004; 58:213–219.

24. Ferrigno D, Buccheri G, Ricca I. Prognostic significance of blood coagulation tests in lung cancer. Eur Respir J. 2001; 17:667–673.

25. Gouin-Thibault I, Samama MM. Laboratory diagnosis of the thrombophilic state in cancer patients. Semin Thromb Hemost. 1999; 25:167–172.

26. Adány R, Bárdos H. Factor XIII subunit A as an intracellular transglutaminase. Cell Mol Life Sci. 2003; 60:1049–1060.

27. Lorand L. Factor XIII and the clotting of fibrinogen: from basic research to medicine. J Thromb Haemost. 2005; 3:1337–1348.

29. Bárdos H, Juhász A, Répássy G, Adány R. Fibrin deposition in squamous cell carcinomas of the larynx and hypopharynx. Thromb Haemost. 1998; 80:767–772.

30. Roselli M, Mineo TC, Basili S, Mariotti S, Martini F, Bellotti A, et al. Vascular endothelial growth factor (VEGF-A) plasma levels in non-small cell lung cancer: relationship with coagulation and platelet activation markers. Thromb Haemost. 2003; 89:177–184.

31. Jiang WG, Ablin R, Douglas-Jones A, Mansel RE. Expression of transglutaminases in human breast cancer and their possible clinical significance. Oncol Rep. 2003; 10:2039–2044.

32. Born P, Lippl F, Ulm K, Gerein P, Lersch C, Eckel F, et al. Reduced levels of coagulation factor XIII in patients with advanced tumor disease. Hepatogastroenterology. 2000; 47:194–198.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download