Abstract
Purpose
The treatment of a clinically node-positive (cN+) neck is important in the management of oral cavity squamous cell carcinoma (OSCC). However, the extent of neck dissection (ND) remains controversial. The purpose of our study was to evaluate whether level IV or V can be excluded in therapeutic ND for cN+ OSCC patients.
Materials and Methods
We performed a retrospective chart review of 92 patients who underwent a comprehensive or selective ND as a therapeutic treatment of cN+ OSCC from January 1993 to February 2009.
Results
The incidence rate of metastasis to level IV or V was 22% (16 of 72) on the ipsilateral neck. Of 67 cases without clinically suspicious nodes at level IV or V, 11 cases (16%, 11 of 67) had pathologically proven lymphatic metastasis to level IV or V. Only a nodal staging above N2b was significantly relevant with the higher rate of level IV or V lymph node metastasis (p=0.025). In this series, selective ND, combined with proper adjuvant therapy, achieved regional control and survival rates comparable to comprehensive ND in patients under the N stage of cN2a OSCC.
The primary goals of treatment of oral cavity squamous cell carcinoma (OSCC) are to control the local disease, eliminate the neck node metastasis, and prevent distant metastasis. Of these, the importance of regional control cannot be overemphasized because cervical lymph node metastasis is the single most potent prognostic factor of OSCC, and locoregional control is also known as a strong predictor of distant metastasis.1,2 About half of the patients with OSCC had pathologically positive lymph node metastases at the time of diagnosis, either clinically or subclinically.3,4 Therefore, the treatment of a clinically node-positive (cN+) neck is very important in the management of OSCC.
However, the extent of neck dissection (ND) remains controversial. Since the time when the surgical treatment of the neck had started as the classical radical ND (RND), there has been a lot of improvement in the aspect of reducing morbidity or extent of treatment. Comprehensive ND (CND) including all levels of the neck has been accepted as the standard treatment for cN+ OSCC in many countries, but selective ND (SND) followed by adjuvant therapy such as radiotherapy or chemo-radiotherapy also has been performed in other institutes.5-7 In order to decide the extent of ND, we investigated the incidence of level IV or V lymph node metastases, attempted to identify the predictive factors of metastasis in cN+ OSCC patients, and compared the survival rate of cN+ OSCC patients treated with SND or CND. The purpose of our study was to determine whether level IV or V could be excluded in therapeutic ND for cN+ OSCC patients.
We retrospectively reviewed the charts of previously untreated OSCC patients who were treated at the Yonsei Head and Neck Cancer Clinic between January 1993 and February 2009. Only patients who met the following criteria were included: 1) the initial treatment was a simultaneous curative surgery on the primary tumor and the neck and 2) therapeutic ND (radical/modified radical ND or SND) was performed for the treatment of a clinically node-positive neck. We excluded patients 1) whose initial treatment was radiotherapy or chemotherapy, 2) had presence of other simultaneous primary tumors, or 3) had distant metastasis at the time of initial presentation.
We proceeded with this study in two categories. First, we investigated the incidence of level IV or V lymph node metastases and identified the predictive factors of level IV or V metastasis in cN+ OSCC patients who were treated with CND. Second, we compared the survival rate or regional recurrence of cN+ OSCC patients who were treated with SND including level I, II and III (SND I-III) or CND. Prior to 2005, authors performed CND for the treatment of cN+ OSCC patients, but since 2005, the policy changed so that for the cases with cN1 or cN2a, we performed SND I-III. Therefore, we compared the oncologic outcome of cN1 or cN2a OSCC patients who were treated before 2005 with patients after 2005. Consequently, a total of 92 patients were included in this study-72 in the CND group and 20 in the SND group. Seventy-two patients of the CND group also included 34 patients with cN1 or cN2a necks.
Patients' charts were reviewed regarding age, gender, origin of primary tumor, T stage, N stage based on the criteria of the American Joint Committee on Cancer (2009), and the type of surgery performed. All patients were preoperatively determined as clinically N+, with the clinical N+ neck defined as cervical lymph nodes detected at the physical examination, imaging studies (either a computed tomography scan, magnetic resonance imaging or positron emission tomography scan), or fine needle aspiration cytology. The Institutional Review Board of Yonsei University College of Medicine approved this retrospective study.
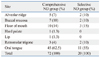
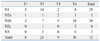
This study included 57 males and 15 females in the CND group and 17 males and 3 females in the SND group. The mean age was 53 years (range: 20-79) in the CND group and 56 years (range: 35-73) in the SND group. The distribution of primary sites is shown in Table 1. Table 2 and 3 summarize the clinical stages of all the cases. The age, sex and clinical stage were not different in both groups (data not shown).
During ND, the contents of the level IV and V specimen were dissected, labeled and processed separately from the main neck dissection specimen. Surgical specimens were then sent to the Pathology Department for permanent section analysis. Histopathologic examination of the metastases included identifying the number and location of the nodes containing metastatic disease. The relationship between level IV or V lymph node metastasis and clinicopathologic predictive factors was assessed.
We compared the survival rates of cN1 or cN2a patients treated by CND or SND. Thirty-four patients were treated with CND and 20 patients with SND. The follow-up period ranged from 5 to 182 months (mean follow-up: 47 months). Patients were followed up for the minimum of two years, or until death. The actuarial 2-year disease-free survival rates were generated.
Statistical analysis was done with the Fisher's exact test, Mann-Whitney U test, Kaplan-Meier method and log-rank test. Statistical significance was defined as p<0.05.
In the CND group, ipsilateral CNDs were performed in 72 patients; radical, modified radical, or extended radical NDs in 15, 49, or 8 necks, respectively. The contra-lateral neck was managed with RND in 5, SND I-III in 42, and observation in 25 patients. An average of 39.3 (range 18-75) lymph nodes were collected from each neck. The mean number of lymph nodes harvested from each level was as follows: 4.1 (range 0-15) from level I, 12.5 (range 2-24) from level II, 7.7 (range 1-20) from level III, 7.2 (range 1-22) from level IV and 8.3 (range 1-19) from level V.
In the SND group, SND I-III was performed in 20 patients for the treatment of cN1 or cN2a neck. The contra-lateral neck was managed with SND I-III in 12 and observation in 8 patients.
Patients received postoperative radiotherapy if they had at least one of the following criteria: 1) multiple lymph node metastases, 2) extracapsular spread of the metastases on histopathological evaluation of the material from the neck dissection, 3) the resected primary tumor demonstrated a positive or very close margin, or 4) the primary tumor was stage 3 or 4. In the CND group, 28 out of 34 cN1, cN2a patients received postoperative radiotherapy. Postoperative radiotherapy was performed after initial surgical treatment in 17 out of 20 SND patients. The mean dose in the CND and SND group were 58.4 Gy (range, 50.4-66.8 Gy) and 58.9 Gy (range, 50.4-74.4 Gy), respectively.
From the 72 patients that were evaluated, 62 (86%) were revealed to have lymph node metastases by pathologic examination. Of these 62 patients, 60 had ipsilateral positive lymph nodes, while the remaining two had contra-lateral lymph nodes only. Fourty-five percent (27 of 60) of patients had ipsilateral metastatic lymph nodes at a single level and 55% (33 of 60) at multiple levels. Level I and II were most frequently affected on the ipsilateral side, with a similar prevalence of 45.8% (33 of 72). The distribution of pathologically positive lymph nodes by level is described in Table 3.
The incidence rate of metastasis to level IV or V was 22% (16 of 72) on the ipsilateral neck. 11 patients were revealed to have nodal metastasis in level IV, 1 in level V, and 4 in level IV and V. Of those 16 patients, 5 had clinically suspicious metastatic nodes on level IV and the remaining 11 did not. Therefore, all five cases that were preoperatively suspected to have metastatic nodes at level IV eventually were revealed to have pathologic positive nodes in level IV. There was no patient who was suspected to have level V metastasis pre-operatively. Of the 67 cases that were believed to have a clinically node-negative level IV neck, 11 cases were histologically proven to have level IV metastases. Therefore, the occult metastasis rate of level IV was 16% (11 of 67). In level V, there were five cases with pathologically positive lymph nodes, but none were detected pre-operatively. The occult metastasis rate of level V was 7% (5 of 72), and the clinical N stage of these patients were cN2b in four cases and cN2c in one.
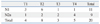
Six patients were clinically suspected to have bilateral metastasis (Table 2). One patient who had a suspicious node only in contra-lateral level I was treated with SND (I-III), while the remaining five cases underwent comprehensive ND. Contra-lateral level IV or V involvement was confirmed in three cases (Table 3). No patients had been detected to have contra-lateral level IV or V metastasis pre-operatively, and all patients who had contra-lateral level IV or V metastasis were diagnosed with advanced T stage (all T4a) and had multiple neck nodes in the contra-lateral neck. However, we found no statistically significant predictive factor for contra-lateral level IV or V metastasis because of the small number of patients (Table 4).
We analyzed the relationship between level IV or V lymph node metastasis and several clinicopathologic factors in 67 patients with clinically positive nodes within neck level I, II or III. There were no statistically significant differences in age, sex, clinical T stage, or histologic grade. Only a nodal staging above N2b was significantly relevant with level IV (p=0.025) (Table 5) and level V lymph node metastasis (p=0.036).
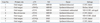
In the CND group, nine patients (26.4%) died of tumors, five (14.2%) died of causes unrelated to OSCC, and 20 patients (59%) were alive and free of cancer at the time of final follow-up. Of the nine patients who died of tumors, local failure developed in three patients, regional or locoregional failure in three, and distant failure in the remaining three. In the SND group, six patients (30%) died of tumors, two (10%) died of causes unrelated OSCC and 12 patients (60%) were alive and free of cancer. Local failure occurred in two patients, regional failure in three, and distant failure in one.
Regional recurrence (RR) occurred in four and three patients in the CND and SND group, respectively. In the CND group, RR developed in the ipsilateral dissected neck in three patients and one in contralateral undissected neck, while all recurrences occurred within the ipsilateral field of dissection in the SND group. There was no RR in level IV or V in either group. The CND patient who had recurred in the contralateral undissected neck was reoperated successfully with salvage ND followed by postoperative chemoradiotherapy, but the remaining six patients died of recurred neck disease. The clinical information of these patients are described in Table 6.
Calculated by the Kaplan-Meier method, the 2-year actuarial disease-free survival rate was 71.8% in the CND group and 69.2% in the SND group, and difference was not statistically significant (p=0.823). Similar to the disease-free survival, the 2-year neck control rate of both groups were not statistically different (CND 88.0% vs. SND 84.0%, p=0.719) (Fig. 1).
It is well known that the surgical removal of cancer is one of the most important treatment in OSCC and locoregional control is closely connected with survival.8,9 In addition, the most common cause of treatment failure of OSCC is known to be nodal failure. As it is extremely difficult to salvage from recurrence after initial surgery,8 the first surgical management of the neck should include proper extent if indicated.
Classical RND was accepted as the treatment of choice in neck management of head and neck cancers since 1906 when it was first described by Crile. However, performing RNDs risks causing surgical morbidities. Regarding level IV or V, there could be spinal accessory nerve injury,10 phrenic nerve paralysis11 or chylous leakage.12,13 Therefore, there has been a general effort to reduce morbidity and overtreatment when performing neck dissections. In OSCC, it has been reported that lymph node metastases usually occur in level I, II or III in several post-surgical pathologic studies.14,15 SND I-III is widely accepted as an elective treatment for clinically node-negative OSCC patients, while comprehensive ND removing every neck node from level I to level V is still regarded as the standard treatment for clinically node-positive OSCC patients in many institutes.9,14
Several authors have reported equivalent regional control and survival rates with protocols of SND followed by adjuvant therapy, such as radiotherapy or chemo-radiotherapy, compared to RND.5,6,16 However, most patients who had pathologically proven metastatic lymph nodes received high dose post-operative adjuvant therapy; therefore, it is difficult to assess whether the control of neck disease was accomplished by proper surgery or by adjuvant therapy. However, there are many widely known long-term morbidities caused by chemo-radiotherapy, such as xerostomia, dysphagia or neck fibrosis.17,18 If we could accurately predict the possibility of nodal metastasis with the patients' clinical characteristics and remove the suspicious area appropriately, we could decrease the severity of adjuvant therapy. However, this study is only a retrospective study, so there is still a long way to go until we are able to precisely predict nodal metastasis and subsequently reduce the dosage or extent of adjuvant therapy. Future multi-center studies might be helpful in overcoming these obstacles.
Many authors have suggested that patients with a greater than 20% risk of occult metastases, based on the anatomic location and the T stage of the primary tumor, should undergo elective ND.19,20 In this study, the occult metastasis rate of level IV in patients who have suspicious nodes in level I, II or III was 16% (11 of 67). However, the occult metastasis rate for level IV in patients under the N stage of cN2a was 6% (2 of 33) and 26% (9 of 34) in patients over cN2b. The difference between two groups was statistically significant in this series (p=0.025). Hence, we should consider a removal of level IV lymph nodes in patients with an N stage higher than N2b. However, the occult metastasis rate to level V was 7% (5 of 72) and 13% (5 of 38) even in patients over cN2b. This result was similar with our previous report21 and other studies.22,23
Based on these studies and our own clinical data, the policy of neck treatment for OSCC changed in 2005 and since then, patients under the N stage of cN2a have been treated with SND I-III rather than modified radical ND or RND. Therefore, we were able to compare the oncologic outcome of cN1 or cN2a OSCC patients according to neck treatment, CND or SND I-III. In this series, SND combined with proper adjuvant therapy, achieved a survival rate comparable to CND in patients under the N stage of cN2a OSCC. In addition, regional recurrence did not occur in level IV or V in either group.
In conclusion, due to the low occult metastasis rate, equivalent survival rate and regional control, level IV and V did not have regional recurrance in patients under cN2a OSCC, but the exclusion of level IV or V in the therapeutic ND in patients with an N stage higher than cN2b needs further investigation. Thus, we suggest level IV and V patients can avoid recurrence under cN2a OSCC patients.
Figures and Tables
Fig. 1
Disease-free survival and neck control rates according to neck dissection. (A) Disease-free survival. (B) Neck control rate. CND, comprehensive neck dissection; SND, selective neck dissection.

References
1. Liao CT, Wang HM, Chang JT, Ng SH, Hsueh C, Lee LY, et al. Analysis of risk factors for distant metastases in squamous cell carcinoma of the oral cavity. Cancer. 2007. 110:1501–1508.

2. Jerjes W, Upile T, Petrie A, Riskalla A, Hamdoon Z, Vourvachis M, et al. Clinicopathological parameters, recurrence, locoregional and distant metastasis in 115 T1-T2 oral squamous cell carcinoma patients. Head Neck Oncol. 2010. 2:9.

3. Lindberg R. Distribution of cervical lymph node metastases from squamous cell carcinoma of the upper respiratory and digestive tracts. Cancer. 1972. 29:1446–1449.

4. Sano D, Myers JN. Metastasis of squamous cell carcinoma of the oral tongue. Cancer Metastasis Rev. 2007. 26:645–662.

5. Simental AA Jr, Duvvuri U, Johnson JT, Myers EN. Selective neck dissection in patients with upper aerodigestive tract cancer with clinically positive nodal disease. Ann Otol Rhinol Laryngol. 2006. 115:846–849.

6. Ferlito A, Rinaldo A, Silver CE, Gourin CG, Shah JP, Clayman GL, et al. Elective and therapeutic selective neck dissection. Oral Oncol. 2006. 42:14–25.

7. Ambrosch P, Kron M, Pradier O, Steiner W. Efficacy of selective neck dissection: a review of 503 cases of elective and therapeutic treatment of the neck in squamous cell carcinoma of the upper aerodigestive tract. Otolaryngol Head Neck Surg. 2001. 124:180–187.

8. Leemans CR, Tiwari R, Nauta JJ, van der Waal I, Snow GB. Regional lymph node involvement and its significance in the development of distant metastases in head and neck carcinoma. Cancer. 1993. 71:452–456.

9. Nikolarakos D, Bell RB. Management of the node-positive neck in oral cancer. Oral Maxillofac Surg Clin North Am. 2008. 20:499–511.

10. Dijkstra PU, van Wilgen PC, Buijs RP, Brendeke W, de Goede CJ, Kerst A, et al. Incidence of shoulder pain after neck dissection: a clinical explorative study for risk factors. Head Neck. 2001. 23:947–953.

11. de Jong AA, Manni JJ. Phrenic nerve paralysis following neck dissection. Eur Arch Otorhinolaryngol. 1991. 248:132–134.

12. Crumley RL, Smith JD. Postoperative chylous fistula prevention and management. Laryngoscope. 1976. 86:804–813.

13. de Gier HH, Balm AJ, Bruning PF, Gregor RT, Hilgers FJ. Systematic approach to the treatment of chylous leakage after neck dissection. Head Neck. 1996. 18:347–351.

14. Ho CM, Lam KH, Wei WI, Lau WF. Treatment of neck nodes in oral cancer. Surg Oncol. 1992. 1:73–78.

15. Shah JP, Candela FC, Poddar AK. The patterns of cervical lymph node metastases from squamous carcinoma of the oral cavity. Cancer. 1990. 66:109–113.

16. Pathak KA, Das AK, Agarwal R, Talole S, Deshpande MS, Chaturvedi P, et al. Selective neck dissection (I-III) for node negative and node positive necks. Oral Oncol. 2006. 42:837–841.

17. Nguyen NP, Moltz CC, Frank C, Vos P, Smith HJ, Karlsson U, et al. Dysphagia following chemoradiation for locally advanced head and neck cancer. Ann Oncol. 2004. 15:383–388.

18. Larson DL. Management of complications of radiotherapy of the head and neck. Surg Clin North Am. 1986. 66:169–182.

19. Weiss MH, Harrison LB, Isaacs RS. Use of decision analysis in planning a management strategy for the stage N0 neck. Arch Otolaryngol Head Neck Surg. 1994. 120:699–702.

20. Persky MS, Lagmay VM. Treatment of the clinically negative neck in oral squamous cell carcinoma. Laryngoscope. 1999. 109(7 Pt 1):1160–1164.

21. Lim YC, Koo BS, Lee JS, Choi EC. Level V lymph node dissection in oral and oropharyngeal carcinoma patients with clinically node-positive neck: is it absolutely necessary? Laryngoscope. 2006. 116:1232–1235.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download