Abstract
Purpose
Thiazolidinediones are insulin-sensitizing agents that reduce neointimal proliferation and the adverse clinical outcomes associated with percutaneous coronary intervention (PCI) in patients with diabetes mellitus (DM). There is little data on whether or not low dose pioglitazone reduces adverse clinical outcomes.
Materials and Methods
The study population included 121 DM patients with coronary artery disease and they were randomly assigned to 60 patients taking 15 mg of pioglitazone daily in addition to their diabetic medications and 61 patients with placebo after the index procedure with drug-eluting stents (DESs). The primary end points were rate of in-stent restenosis (ISR) and change in atheroma volume and in-stent neointimal volume. The secondary end points were all-cause death, myocardial infarction (MI), stent thrombosis and re-PCI.
Results
There were no statistical differences in the clinical outcomes and the rate of ISR between the two groups [all-cause death; n=0 (0%) in the pioglitazone group vs. n=1 (1.6%) in the control group, p=0.504, MI; n=2 (3.3%) vs. n=1 (1.6%), p=0.465, re-PCI; n=6 (10.0%) vs. n=6 (9.8%), p=0.652, ISR; n=4 (9.3%) vs. n=4 (7.5%), p=1.000, respectively].
There were no differences in changes in neointimal volume, percent neointimal volume, total plaque volume and percent plaque volume between the two groups on intravascular ultrasonography (IVUS) study.
With the introduction of drug-eluting stents (DESs), the occurrence of in-stent restenosis (ISR) has dramatically decreased. However, ISR still remains a challenging obstacle in specific conditions, such as diabetic patients, long and multiple stent implantations and acute coronary syndrome. Especially in patients with diabetes mellitus, many studies have shown that increased restenosis after percutaneous coronary intervention (PCI) is partially due to amplified inflammatory response and increased neointimal hyperplasia. To overcome this problem, a variety of drugs with the potential to suppress neointimal proliferation have been evaluated, but most of them were not successful.
Thiazolidinediones (TZDs) are agonists of the peroxisome proliferation-activated receptor-γ (PPAR-γ) and they are anti-diabetic agents with activities for regulating the transcription of genes encoding proteins involved in insulin sensitivity and lipid metabolism.1 Recent intravascular ultrasonography (IVUS) studies have reported they have the potential to reduce neointimal proliferation, ISR and revascularization after bare-metal stent (BMS) implantation.2-7 However, many studies,8-10 including a recent meta-analysis evaluating rosiglitazone in about 27000 patients with diabetes, showed that rosiglitazone was related to an increased risk of cardiovascular death and myocardial infarction.8
Although whether pioglitazone presents the same risks as rosiglitazone remains unsolved, it seems that pioglitazone reduces cardiovascular events compared with a placebo group.11,12 One of the largest trials, the Prospective Pioglitazone Clinical Trial in Macrovascular Events (PROactive) trial, evaluated more than 5000 diabetic patients at high risk of macrovascular complications, and the study showed that pioglitazone non-significantly reduced the risk of coronary and peripheral vascular events.11 In terms of a secondary end point, a composite of death from myocardial infarction or stroke, a statistically significant risk reduction was reported in the pioglitazone medication group.11
Until now, most of the studies were performed with pioglitazone of 30-45 mg daily in patients who underwent PCI with BMSs.13-15 Few studies have systematically examined the effect of low dose pioglitazone, especially in patients who underwent PCI with DESs.16,17
The objective of our study was to assess whether low-dose pioglitazone (15 mg/day) reduces ISR, neointimal proliferation, atheroma volume and cardiovascular events in type 2 diabetes mellitus (DM) patients undergoing PCI with DESs.
This study was a single center, prospective and placebo-controlled randomized study. From October 2009 to July 2011, the study population included patients who had a known medical history or they were newly diagnosed with type 2 DM and symptomatic ischemic heart disease with an angiographically significant coronary lesion and who had undergone PCI with DESs. For the diagnosis of type 2 DM, patients had to meet the criteria of 1) fasting plasma glucose level >126 mg/dL, 2) known medical history of type 2 DM and 3) glycosylated hemoglobin level >7 mg/dL. For glycemic control, all kinds of diabetic medication were allowed, including insulin. Coronary artery disease included one-vessel or multi-vessel disease, a vessel length of less than 50 mm and a vessel diameter from 2.5 mm to 4 mm with de novo lesion, diffuse long lesion and ostial lesion. The exclusion criteria were patients who were already taking pioglitazone or patients with bifurcated (>2 mm) lesion, chronic total obstruction lesion, left main lesion, liver and renal dysfunction, left ventricular (LV) dysfunction (LV ejection fraction <40%) at the time of PCI or previous myocardial infarction (MI) in the previous 6 weeks before intervention. After the index PCI procedure with DESs, the patients were randomly assigned to two groups: either the study (pioglitazone 15 mg daily) group or the control group (placebo daily). The patients took the medication for 12 months.
A total of 121 patients completed with clinical follow-up: 60 patients in the pioglitazone group and 61 patients in the placebo group. At 12 months after PCI, complications and clinical outcomes were assessed, including all-cause death, re-PCI [target lesion revascularization (TLR), target vessel revascularization (TVR), non-TVR], MI and stent thrombosis. TLR was defined as clinically and angiographically driven PCI of the initially treated target lesion, including the stented segments and the segments within 5 mm from both the proximal and distal stent edges. TVR was defined as clinically and angiographically assessed PCI of the initially treated target vessel.
The primary end points were rate of ISR and late loss according to quantitative angiographic analysis as well as changes in atheroma and neointimal volume according to IVUS analysis. The secondary end points were all-cause death, MI [non-ST segment elevation myocardial infarction (NSTEMI), ST segment elevation myocardial infarction (STEMI)], re-PCI (TLR, TVR, non-TVR), a composite of them (all-cause death, MI, re-PCI) and stent thrombosis at 12 months.
Coronary angiography was performed with the standard radial and femoral approaches. Before the procedure, all patients received a loading dose of aspirin (300 mg) and clopidogrel (300-600 mg) and 100 U/kg of heparin intravenously; this maintained the activated clotting time within 250-300 seconds. For the IVUS study, intracoronary nitroglycerin (200 µg) was administered. An IVUS study was done before and after the stenting procedure. A commercially available system (CVIS/Boston Scientific Corporation, San Jose, CA, USA) was used for the IVUS examinations. The system consisted of a single-element 40-MHz transducer mounted on the tip of a flexible shaft rotating at 1800 rpm within a 2.6-F rapid exchange/common distal lumen imaging sheath. The IVUS study was performed with an automated pullback device at a rate of 0.5 mm/s. After the index PCI, the patients were maintained on a treatment of aspirin (100 mg/day) plus clopidogrel (75 mg/day) for at least 12 months.
All the angiographic and IVUS data were analyzed by two cardiologists who were blinded to the clinical information and the objective of this trial. Minimal luminal diameter (MLD) and reference diameter (RD) were measured and the percent of diameter stenosis was calculated. We estimated neointimal proliferation in the stent area and change in atheroma in the target lesion, which was more than 10 mm apart from stent (Fig. 1). All the ultrasound images were reviewed and evaluated for both qualitative and quantitative parameters. The images were digitized to perform morphometric analysis with commercially available planimetry software (echoPlaque, IndecMedical Systems, Santa Clara, CA, USA). The lumen and stent cross-sectional areas (CSAs) were measured throughout the stented segment at 1.0-mm increments. Neointimal CSA was then calculated as the difference between stent CSA and lumen CSA and neointimal volume was calculated with Simpson's method. The neointimal index was calculated as: neointimal volume/stent volume ×100. The lumen and vessel CSAs were measured at 1.0-mm increments for 10 mm from both the proximal and distal stent edges in a subset of the patients. Plaque CSA was calculated as the vessel CSA minus the lumen CSA. The vessel, lumen and plaque volumes were calculated with Simpson's method. The vessel, lumen and plaque volume indexes were calculated as volume divided by the length of the measured atheroma.
The quantitative data are presented as means±SDs or medians with inter-quartile ranges, and the qualitative data are presented as frequencies. Continuous variables were compared with t-tests. If normality was not met, then Wilcoxon test and Mann-Whitney test were used. Non-continuous variables were compared by the chi-square test. Statistical significance was met for p-values less than 0.05. All statistical analyses were performed with the SPSS version 18.0 software package (SPSS Inc., Chicago, IL, USA).
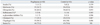
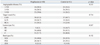
A total of 121 patients were followed for 12 months (60 patients in the pioglitazone group and 61 patients in the control group). One hundred and five patients (51 in the pioglitazone group and 54 in the control group) completed follow-up coronary angiography. Among them, follow-up IVUS was done in thirty-four patients (18 in the pioglitazone group and 16 in the control group). The baseline clinical demographic and angiographic findings were not significantly different between the two groups (Table 1). More than 70% of the patients were male. The mean age was 60.3±9.5 in the pioglitazone group and 61.9±8.8 in the control group. The average disease duration of DM was 6.0±7.0 years in the pioglitazone group and 5.5±6.4 years in the control group (p=0.407). There were no significant differences in medications. About seventy three percent of the patients were taking statins (atorvastatin, rosuvastatin) in both groups (Table 2).
There were no significant differences in the angiographic procedures between both groups (Table 3).
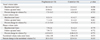
Coronary angiographic follow-up was done in 51 patients in the pioglitazone group and 54 patients in the control group. There were also no significant differences in the quantitative coronary angiographic analysis (QCA) analyses in both groups. The mean lesion length and reference diameter (RD) were similar between the two groups (RD: 2.64±0.46 mm in the pioglitazone group and 2.67±0.43 mm in the placebo group, p=0.809, lesion lengths: 26.6±10.79 mm in the pioglitazone group and 28.5±13.18 mm in the placebo group, p=0.412). There were no significant differences in pre-MLD, post-MLD and MLD at 12-month follow-up between both groups. This was the same for the pre- and post-follow-up diameter stenoses (Table 4). The amount of late loss was similar between the two groups (0.35±0.57 in the pioglitazone group and 0.31±0.60 in the control group, p=0.97). There were no significant differences in the ISR between both groups [4 patients (9.3%) in the pioglitazone group and 4 patients (7.5%) in the placebo group].
At 12 months, neointimal volume index, as analyzed by IVUS, in the stent area was not significantly different between both groups (1.86±1.04 mm3/mm in the pioglitazone group and 2.08±0.58 mm3/mm in the control group, p=0.474). The percent change in neointimal volume (%) was not statistically different (20.3±10.3% vs. 22.9±3.6%, respectively, p=0.315) (Table 5). IVUS analysis was performed on the atheroma in the target lesions more than 10 mm apart from the stent at baseline and at 12 months. There was no statistically significant reduction in plaque volume in the pioglitazone group compared to that in the control group (follow-up plaque volume index: 7.9±7.5 mm3/mm vs. 7.6±3.4 mm3/mm, p=0.772, percent change in plaque volume: -0.03±0.21% vs. -0.06±0.33%, p=0.772, respectively) (Table 5).
The baseline lipid profile was similar in both groups and mean glycosylated hemoglobin levels showed no significant difference (Table 6). In the pioglitazone group, triglyceride (TG) levels were decreased and high density lipoprotein cholesterol levels were increased at the 12 month follow-up compared to the control group, but there were no significant differences.
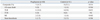
An in-hospital complication occurred in only 1 patient (1.2%) in the control group and there was none in the pioglitazone group. The incidence of major adverse cardiac event (MACE) at 12 month follow-up was not significantly different between both groups [7 patients (11.7%) in the pioglitazone group and 8 patients (13.1%) in the control group, p=0.514]. The incidences of each of the components of MACE (death, MI, TLR, TVR, stent thrombosis) were similar between both groups (Table 7). Stent thrombosis developed in 1 patient (1.7%) in the pioglitazone group and in 2 patients (3.3%) in the control group.
Among the results of our study, the administration of low dose pioglitazone (15 mg daily) was unable to reduce ISR, late loss, neointimal hyperplasia and atheroma. All cause death, MI, stent thrombosis and re-PCI in the pioglitazone group were not significantly different from those of the control group. Low dose pioglitazone did reduce coronary atheroma and ISR, different from that of high dose pioglitazone.
Thiazolidinediones act as PPAR-γ agonists and they have immunomodulatory and anti-inflammatory actions. They eventually reduce the early phase of atherosclerosis and attenuate the development of intimal hyperplasia after balloon-induced vascular injury.13,18 In regards to their mechanisms, TZDs suppress growth factor-mediated proliferation and migration of vascular smooth muscle cells; they enhance cytokine-mediated apoptosis of developed neointimal tissues and they may increase epithelial progenitor cells resulting in increased endothelialization and reduction of in-stent restenosis.19,20 PPAR-γ is highly expressed in activated macrophages,21 and so activation of PPAR-γ receptors with pioglitazone in the macrophages within the arterial wall after PCI may reduce local inflammatory and proliferative responses, thereby, finally, reducing restenosis.
Many previous studies have reported that high dose pioglitazone (30-45 mg/day) reduced neointimal hyperplasia by IVUS analysis and reduced the rate of ISR and TLR in both diabetic13-15,22 and non-diabetic patients23 who underwent PCI. As compared with rosiglitazone, which is known to increase cardiovascular adverse events,8 pioglitazone has been found to have beneficial effects on cardiovascular endpoints according to large trials like the PROactive trial (PROspective pioglitAzone Clinical Trial In macroVascular Events)11 and the PERISCOPE trial (Pioglitazone Effect on Regression on Intravascular Sonographic Coronary Obstruction Prospective Evaluation).17 The PROactive trial, which involved more than 5000 type 2 DM patients with known macrovascular disease, showed that pioglitazone treatment did not reduce the primary outcome, which was a composite of cerebral, cardiac and peripheral events, nor both disease-related and procedural endpoints, but a statistically significant reduction in the main secondary outcomes of all-cause mortality, MI or stroke was reported.11 However, almost every study has evaluated the effect of pioglitazone at full doses of 30 mg to 45 mg per day. In the real world, for the several reasons, including the risk of peripheral edema, aggravation of congestive heart failure and liver dysfunction, as well as cost and limited health insurance coverage, prescribing a full dose of pioglitazone is limited. Therefore, the evaluation of a threshold concentration of pioglitazone that can reduce ISR and neointimal proliferation is necessary for its application in the clinical field. There is, however, little data on the effect of low dose pioglitazone. One trial evaluated the benefit of pioglitazone at 15 mg per day in humans.16 In that trial, low dose pioglitazone reduced ISR at 6 months after primary PCI with BMSs in patients with acute myocardial infarction and type 2 DM or impaired glucose tolerance. Fifty six patients treated with pioglitazone were compared with 37 patients treated without pioglitazone. At the 6 month follow-up, the ISR rate was also significantly lower in the pioglitazone group than that in the controls (21.3% vs. 44.8%, respectively, p=0.03).16 One other retrospective cohort study showed that compared with rosiglitazone, both a high dose of pioglitazone (30 mg/day) and a low dose of pioglitazone (15 mg) were associated with a significantly lower risk of the composite outcomes of death, readmission, MI and heart failure in DM patients.17 In our study, the administration of low dose pioglitazone failed to reduce the rates of ISR and neointimal proliferation. This result was different from that of high dose pioglitazone. This could be explained by several factors. First, our results may be related to the dose of pioglitazone. High dose pioglitazone suppress local inflammatory conditions after PCI and reduces ISR, but low dose pioglitazone may be not sufficient to suppress the local inflammatory process after PCI. Joner, et al. reported that a low dose of pioglitazone (3 mg/kg per day, which was equivalent of 15 mg/day in humans) did not reduce neointimal proliferation and restenosis after PCI with BMSs in a rabbit model. But high doses of pioglitazone did reduce neointimal proliferation and restenosis.24 Second, although a beneficial effect for pioglitazone in reducing ISR, neointimal proliferation and clinical outcomes has been reported by a large randomized trial and meta-analysis, almost all of the subjects were DM patients who underwent PCI with the BMS. There is currently little data on whether or not pioglitazone reduces ISR and neointimal proliferation in DM patients who have undergone PCI with DESs. Therefore, the effect of pioglitazone on neointimal proliferation after PCI with DESs should be thoroughly investigated by a large-scaled randomized trial. A large scale randomized multicenter center study comparing the efficacy of patients receiving both high dose pioglitazone and sirolimus-eluting stents is in progress in Italy.
In our study, there were no differences in clinical outcomes at 12 months between a low dose pioglitazone group and control group. There was no data on long term clinical outcomes for low dose pioglitazone. Large scale long term follow-up study will be needed with low dose pioglitazone.
Langenfeld, et al.25 reported that high dose pioglitazone (45 mg/day) reduced carotid intimal media thickness (IMT) after 12 and 24 weeks. Rosiglitazone also reduced the carotid IMT.26 But there is currently no data on whether or not pioglitazone could induce regression of coronary atheroma. We analyzed atheroma on target lesions by IVUS after the administration of low dose pioglitazone for 12 months. There was no change in plaque volume index and percent change in plaque volume compared to the control group. This result may indicate that a low dose of pioglitazone is not sufficient to reduce coronary atheroma. The reason therefore may be as follows: change in carotid IMT is more sensitive than that in coronary atheroma after taking statins and PPAR-γ agonists. High dose rosuvastatin regressed coronary atheroma in the ASTEROID study.27 Statin has a strong influence on LDL cholesterol. Regression of coronary atheroma is mostly related to a reduction of LDL-C. Pioglitazone mainly reduces TG. Therefore, we were unable to observe a change in coronary atheroma in our study.
The limitations of our study are the small sample size, single center study, and heterogeneity in the type of DES used. Considering the low incidence of restenosis after DES, a large scale randomized study will be needed with low dose pioglitazone.
In conclusion, our study demonstrated that low dose pioglitazone does not reduce ISR, neointimal volume nor atheroma volume after 12 months in DM patients who have undergone PCI with DESs.
Figures and Tables
 | Fig. 1IVUS image for measure of neointimal volume at in-stent lesion (A) and atheroma volume at another target lesion (B). IVUS, intravascular ultrasonography. |
ACKNOWLEDGEMENTS
This study was supported by a grant from the Korean Heath Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (A070001).
References
2. Takagi T, Yamamuro A, Tamita K, Yamabe K, Katayama M, Mizoguchi S, et al. Pioglitazone reduces neointimal tissue proliferation after coronary stent implantation in patients with type 2 diabetes mellitus: an intravascular ultrasound scanning study. Am Heart J. 2003; 146:E5.

3. Takagi T, Akasaka T, Yamamuro A, Honda Y, Hozumi T, Morioka S, et al. Troglitazone reduces neointimal tissue proliferation after coronary stent implantation in patients with non-insulin dependent diabetes mellitus: a serial intravascular ultrasound study. J Am Coll Cardiol. 2000; 36:1529–1535.

4. Takagi T, Yamamuro A, Tamita K, Yamabe K, Katayama M, Morioka S, et al. Impact of troglitazone on coronary stent implantation using small stents in patients with type 2 diabetes mellitus. Am J Cardiol. 2002; 89:318–322.

5. Takagi T, Yamamuro A, Tamita K, Katayama M, Morioka S. Thiazolidinedione treatment attenuates diffuse neointimal hyperplasia in restenotic lesions after coronary stent implantation in type 2 diabetic patients: an intravascular ultrasound study. J Cardiol. 2005; 45:139–147.
6. Choi D, Kim SK, Choi SH, Ko YG, Ahn CW, Jang Y, et al. Preventative effects of rosiglitazone on restenosis after coronary stent implantation in patients with type 2 diabetes. Diabetes Care. 2004; 27:2654–2660.

7. Osman A, Otero J, Brizolara A, Waxman S, Stouffer G, Fitzgerald P, et al. Effect of rosiglitazone on restenosis after coronary stenting in patients with type 2 diabetes. Am Heart J. 2004; 147:e23.

8. Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med. 2007; 356:2457–2471.

9. Lincoff AM, Wolski K, Nicholls SJ, Nissen SE. Pioglitazone and risk of cardiovascular events in patients with type 2 diabetes mellitus: a meta-analysis of randomized trials. JAMA. 2007; 298:1180–1188.

10. Singh S, Loke YK, Furberg CD. Long-term risk of cardiovascular events with rosiglitazone: a meta-analysis. JAMA. 2007; 298:1189–1195.

11. Dormandy JA, Charbonnel B, Eckland DJ, Erdmann E, Massi-Benedetti M, Moules IK, et al. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet. 2005; 366:1279–1289.

12. Takagi T, Okura H, Kobayashi Y, Kataoka T, Taguchi H, Toda I, et al. A prospective, multicenter, randomized trial to assess efficacy of pioglitazone on in-stent neointimal suppression in type 2 diabetes: POPPS (Prevention of In-Stent Neointimal Proliferation by Pioglitazone Study). JACC Cardiovasc Interv. 2009; 2:524–531.

13. Goetze S, Xi XP, Kawano H, Gotlibowski T, Fleck E, Hsueh WA, et al. PPAR gamma-ligands inhibit migration mediated by multiple chemoattractants in vascular smooth muscle cells. J Cardiovasc Pharmacol. 1999; 33:798–806.

14. Igarashi M, Hirata A, Yamaguchi H, Tsuchiya H, Ohnuma H, Tominaga M, et al. Characterization of an inhibitory effect of pioglitazone on balloon-injured vascular smooth muscle cell growth. Metabolism. 2001; 50:955–962.

15. Law RE, Goetze S, Xi XP, Jackson S, Kawano Y, Demer L, et al. Expression and function of PPARgamma in rat and human vascular smooth muscle cells. Circulation. 2000; 101:1311–1318.

16. Marx N, Wöhrle J, Nusser T, Walcher D, Rinker A, Hombach V, et al. Pioglitazone reduces neointima volume after coronary stent implantation: a randomized, placebo-controlled, double-blind trial in nondiabetic patients. Circulation. 2005; 112:2792–2798.

17. Nissen SE, Nicholls SJ, Wolski K, Nesto R, Kupfer S, Perez A, et al. Comparison of pioglitazone vs glimepiride on progression of coronary atherosclerosis in patients with type 2 diabetes: the PERISCOPE randomized controlled trial. JAMA. 2008; 299:1561–1573.

18. Aizawa Y, Kawabe J, Hasebe N, Takehara N, Kikuchi K. Pioglitazone enhances cytokine-induced apoptosis in vascular smooth muscle cells and reduces intimal hyperplasia. Circulation. 2001; 104:455–460.

19. Jiang C, Ting AT, Seed B. PPAR-gamma agonists inhibit production of monocyte inflammatory cytokines. Nature. 1998; 391:82–86.

20. Hahn JY, Kim HS, Koo BK, Na SH, Chung JW, Youn TJ, et al. One month follow-up C-reactive protein may be a useful predictor of angiographic restenosis and long-term clinical outcomes after bare metal stent implantation. Int J Cardiol. 2006; 109:267–269.

21. Delhaye C, Maluenda G, Wakabayashi K, Ben-Dor I, Lemesle G, Collins SD, et al. Long-term prognostic value of preprocedural C-reactive protein after drug-eluting stent implantation. Am J Cardiol. 2010; 105:826–832.

22. Patel D, Walitt B, Lindsay J, Wilensky RL. Role of pioglitazone in the prevention of restenosis and need for revascularization after bare-metal stent implantation: a meta-analysis. JACC Cardiovasc Interv. 2011; 4:353–360.

23. Rosmarakis ES, Falagas ME. Effect of thiazolidinedione therapy on restenosis after coronary stent implantation: a meta-analysis of randomized controlled trials. Am Heart J. 2007; 154:144–150.

24. Joner M, Farb A, Cheng Q, Finn AV, Acampado E, Burke AP, et al. Pioglitazone inhibits in-stent restenosis in atherosclerotic rabbits by targeting transforming growth factor-beta and MCP-1. Arterioscler Thromb Vasc Biol. 2007; 27:182–189.

25. Langenfeld MR, Forst T, Hohberg C, Kann P, Lubben G, Konrad T, et al. Pioglitazone decreases carotid intima-media thickness independently of glycemic control in patients with type 2 diabetes mellitus: results from a controlled randomized study. Circulation. 2005; 111:2525–2531.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download