Abstract
Purpose
Mycobacterium tuberculosis is endemic in Korea. Because tuberculous peritonitis is characterized by ascites, abdominal pain, abdominal mass and elevation of serum CA-125, it can be confused with ovarian malignancies. The aim of this study was to evaluate the significance of serum CA-125 level in the differential diagnosis of tuberculous peritonitis and ovarian malignancy in a Mycobacterium tuberculosis-endemic area.
Materials and Methods
The medical records of patients diagnosed with tuberculous peritonitis (n=48) or epithelial ovarian malignancy (n=370) at Samsung Medical Center from January 2000 to October 2009 were retrospectively reviewed.
Results
Median serum CA-125 level in the epithelial ovarian cancer group was significantly higher than that in the tuberculous peritonitis group (p≤0.01). Only one patient (2.1%) in the tuberculous peritonitis group had a serum CA-125 level over 2000 U/mL. However, 109 patients (29.5%) in the epithelial ovarian cancer group had a serum CA-125 level over 2000 U/mL. At the CA-125 ranges of 400 to 599 and 600 to 799, the proportions of those with tuberculous peritonitis were 24% and 21.9%, respectively. At a serum CA-125 level over 1000 U/mL, however, the proportion of tuberculous peritonitis was much lower (2.1%).
CA-125 is a glycoprotein expressed by the coelomic epithelium (mesothelial cells of the pleura, pericardium and peritoneum) and Müllerian (tubal, endometrial and endocervical) epithelium.1 Serum CA-125 can be elevated in various conditions including ovarian cancer, endometriosis, pelvic inflammatory disease, tuberculous peritonitis, liver cirrhosis, chronic renal failure, pleural effusion and pancreas or colorectal cancer, as well as in postoperative status.2-7 As serum CA-125 is elevated in 80% of late-stage ovarian cancers,8 it is commonly used as a tumor marker for ovarian cancers.8-10
In clinical practice, newly developed ascites in female patients is a challenging condition, especially if these patients do not have any evidence of liver cirrhosis. In western countries, the most common cause of ascites is liver cirrhosis (85%), followed by malignancy (7%), heart failure (3%) and tuberculous peritonitis (2%).11 In Korea, liver cirrhosis (60%) was also shown to be the leading cause of ascites, followed by malignancy (26%), tuberculous peritonitis (7%) and chronic renal failure (1.6%).12 As Korea remains an endemic area of Mycobacterium tuberculosis, tuberculous peritonitis is a relatively common cause of ascites.12 As tuberculous peritonitis presents with ascites, abdominal pain, abdominal mass and high serum CA-125, it can be confused with ovarian cancers.13,14 In the literature, several cases of tuberculous peritonitis mimicking ovarian cancer have been reported.15-20 Two case control studies have shown that elevated serum CA-125 in patients with tuberculous peritonitis is normalized after anti-mycobacterium medication.21,22 However, there is no report concerning the cut-off value of serum CA-125 level between tuberculous peritonitis and ovarian malignancy in female patients with ascites. The aim of this retrospective study was to evaluate the significance of serum CA-125 level in the differential diagnosis of tuberculous peritonitis and ovarian malignancy.
The medical records of patients who were admitted to the Samsung Medical Center from January 2000 to October 2009 were retrospectively reviewed. The inclusion criteria were 1) patients who were female and 20 years or older, 2) final diagnosis of tuberculous peritonitis or epithelial ovarian cancer, 3) abdominal distension due to physically detectable ascites or more ascites than a physiological amount on abdominal computerized tomography (CT) (usually 50 mL or less23), and 4) available data of serum CA-125 level at initial diagnosis. Patients were excluded for one of the following: 1) ascites due to liver cirrhosis with or without hepatocellular carcinoma, chronic renal failure, heart failure, or any malignancy other than epithelial ovarian cancer, 2) pregnancy, 3) previous history of malignancy or current evidence of any malignancy other than epithelial ovarian cancer, 4) recurred epithelial ovarian cancer or benign ovarian tumor, or 5) previous history of abdominal surgery.
A total of 418 patients who fulfilled all of these criteria were enrolled. Among them, 48 (11.5%) patients were finally diagnosed with tuberculous peritonitis and 370 (88.5%) patients were finally diagnosed with epithelial ovarian cancer. The diagnosis of tuberculous peritonitis was made by surgery in 28 patients (58.3%), by trying anti-TB medications in 16 patients (33.3%), and by AFB stain & culture in 4 patients (8.3%) (Fig. 1). We reviewed the patients' medical records for underlying disease; past history of major surgery, tuberculous infection and malignancy; pregnancy status; symptoms such as fever, abdominal pain, palpable abdominal mass and weight loss; physical findings; serum CA-125 level; findings of chest radiography; the amount of ascites detected by physical examination or by imaging studies (ultrasonography, CT, MRI) and the cytopathologic results of ascites.
The discriminative accuracy of serum CA-125 was evaluated through receiver operating characteristic (ROC) curve analysis. These analyses were performed using PASW software (18.0 by SPSS Inc., Chicago, IL, USA). p-values less than 0.05 were considered significant.
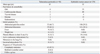
The median age of the tuberculous peritonitis group and epithelial ovarian cancer group was 45 and 53 years, respectively (p<0.01) (Table 1). From the aspect of initial symptoms, abdominal pain and abdominal distension were common symptoms in both groups. For combined tuberculosis of other sites, 2 patients (4.2%) had active pulmonary tuberculosis and 8 patients (16.7%) had intestinal tuberculosis.
On both univariate and multivariate analysis, age and level of CA-125 were significantly correlated with ovarian epithelial cancer (Table 2). Also, a comorbidity of cardiovascular disease seemed to affect ovarian epithelial cancer.
In the tuberculous peritonitis group, the most common radiologic impression on CT was peritoneal carcinomatosis (37.5%), followed by tuberculous peritonitis (35.4%). On initial chest radiography, the frequency of pleural effusion in the tuberculous peritonitis group and ovarian cancer group was not different (16.7% and 14.6%, respectively).
For the examination of ascites in the tuberculous peritonitis group, the sensitivity of AFB staining was 2.4% (1/41) and the sensitivity of AFB culture was 22.0% (9/41). The adenosine deaminase (ADA) level of the ascitic fluid was evaluated in 5 cases, and all 5 patients demonstrated elevated levels of ADA (50-128 IU/L). In 127 patients in the ovarian cancer group with available cytopathologic results of ascites, 82 patients (64.6%) exhibited the presence of malignant cells.
Serum CA-125 level in the epithelial ovarian cancer group was significantly higher than that in the tuberculous peritonitis group (p≤0.01, Mann-Whitney test). In the tuberculous peritonitis group, the median CA-125 level was 418 U/mL (range: 25-2702). Only 2 patients (4.7%) showed a serum CA-125 level under the normal upper limit of 31 U/mL. In the epithelial ovarian cancer group, the median CA-125 level was 1002 U/mL (range: 7-42600).
Fig. 2 shows the distribution of serum CA-125 levels for both groups. Four patients (8.3%) with tuberculous peritonitis had a serum CA-125 level over 1000 U/mL and only one patient (2.1%) had a serum CA-125 level over 2000 U/mL. With respect to the epithelial ovarian cancer patients, 189 patients (51.1%) had a serum CA-125 level over 1000 U/mL and 109 patients (29.5%) had a serum CA-125 level over 2000 U/mL.
Fig. 3 demonstrates the proportions of the two groups for various ranges of serum CA-125. At the CA-125 ranges of 400 to 599 and 600 to 799, the proportions of patients with tuberculous peritonitis were 24% and 21.9%, respectively. However, the proportion of those with tuberculous peritonitis was only 12.5% at the CA-125 range of 800 to 999. For a serum CA-125 level over 1000 U/mL, the proportion of those with tuberculous peritonitis was much lower (2.1%).
The sensitivity and specificity for diagnosing epithelial ovarian cancer from tuberculous peritonitis were calculated at every cut off level of serum CA-125 and expressed on a ROC curve (Fig. 4). The area under the curve was 0.716. At the serum CA-125 level of 943, the sensitivity for diagnosing ovarian cancer was 51.5% and the specificity for diagnosing ovarian cancer was 91.7% (Fig. 5).
As serum CA-125 is commonly elevated in epithelial ovarian malignancy, it is useful for the diagnosis and monitoring of treatment responses. CA-125, however, has several limitations. First, its sensitivity is less than optimal. It is increased in about 50% of early stage ovarian cancers. Secondly, it can be elevated in other benign conditions including peritonitis.24,25 Therefore, many have attempted to find new serum markers for better screening and monitoring of ovarian cancer. For example, a recent study showed that a multiplex, beaded-based immunoassay system, the combination of six markers (leptin, prolactin, osteopontin, insulin-like growth factor 2, macrophage inhibitory factor and CA-125), was better than CA-125 alone in the diagnosis of ovarian cancer.26 Other recent studies have demonstrated the usefulness of HE4 as a tumor marker of ovarian cancer with the capability to distinguish endometriosis from ovarian cancer.27,28
In clinical practice, the first impression for a female patient with ascites and high serum CA-125 is usually ovarian cancer in advanced stages. However, in the present study, the proportion of those with tuberculous peritonitis was higher than our expectation. The proportion of those with tuberculous peritonitis may depend on the prevalence of tuberculosis in a particular society. Recently, the prevalence of tuberculosis has increased in western countries partially due to the epidemic of acquired immunodeficiency syndrome. Therefore, differentiation between ovarian cancer and tuberculous peritonitis should be important not only in Korea but also in western countries. It is especially true considering that tuberculous peritonitis is universally curable.
In previous case series, 11.8% (9/76) of patients with tuberculous peritonitis showed a serum CA-125 level above 1000 U/mL.13,17,19,20,22,29-39 In the present study, in an unselected group of tuberculous peritonitis patients, 8.4% (4/48) showed a serum CA-125 level above 1000 U/mL. In female patients with ascites and a CA-125 level above 1000 U/mL, however, the proportion of tuberculous peritonitis was only 2.1% (4/193). Conversely, 51.1% (189/370) of ascitic patients with ovarian malignancy had a serum CA-125 level over 1000 U/mL. Therefore, in female patients with ascites and a serum CA-125 level over 1000 U/mL, tuberculous peritonitis would be a very exceptional diagnosis.
In this study, the median age of the tuberculous peritonitis group was 45 years, and was significantly younger than that of the ovarian malignancy group and relatively younger than that of a large contemporary study.40 Similar to several other case series studies, the most common symptoms of tuberculous peritonitis group were abdominal pain and abdominal distension.19,41,42 Based on clinical manifestations and imaging studies, 65% of tuberculous peritonitis patients were initially suspicious of peritoneal carcinomatosis caused by ovarian malignancy. This data again shows that clinical manifestations of tuberculous peritonitis and ovarian malignancy considerably overlap.
In the present study, we tried to select a single cut-off level to better differentiate between ovarian cancer and tuberculous peritonitis using an ROC curve. At the serum CA-125 level of 943, the sum of the sensitivity and specificity was highest (Fig. 4). Although the specificity was 0.917, the sensitivity for ovarian malignancy was only 0.515 at the CA-125 level of 943. In our opinion, one single cut-off level of serum CA-125 has little clinical usefulness.
Instead, we assessed the proportions of those with tuberculous peritonitis at certain ranges of serum CA-125 (Fig. 3). For example, at the CA-125 range of 400-599, the proportion of those with tuberculous peritonitis was 24%. As a whole, 19.1% (44/230) of ascitic female patients with a serum CA-125 level below 1000 were diagnosed with tuberculous peritonitis. Therefore, tuberculous peritonitis should always be considered in the differential diagnosis of such patients.
Our study has some limitations. First, only 48 patients with tuberculous peritonitis were included in this study, which was considerably smaller than the number of patients with epithelial ovarian cancer (370 patients). Second, compounding factors which can cause CA-125 elevation were not fully controlled; CA-125 can be increased in inflammatory conditions of the peritoneum and pleura, such as endometriosis, uterine myoma and pelvic inflammatory disease, as well as for frequent ascites tapping, operation or increased pleura fluid due to any cause.
One of the important findings of our study is that more than half of the patients with tuberculous peritonitis (58.3%) needed to have surgery to arrive at the final diagnosis. In the present study, the sensitivity of AFB culture from ascites was only 12.8%. Although the sensitivity of AFB stain and culture was low in present and previous studies,43 more extensive ascites analysis with suspicion of tuberculous peritonitis may be helpful for making diagnoses. In our opinion, a short course of empirical antibiotic treatment can be tried before surgery, as serum CA-125 level rapidly returned to normal when anti-Mycobacterium medication was given.21,22
In conclusion, the possibility of tuberculous peritonitis should be considered in the differential diagnosis of patients with ascites and high serum CA-125 level. Upon high suspicion of tuberculous peritonitis, some patients may be saved from unnecessary laparotomy and still achieve the final diagnosis.
Figures and Tables
Fig. 1
Methods of final diagnosis in patients with tuberculous peritonitis. Fifty-nine percent of the patients underwent a surgical procedure to arrive at the final diagnosis. Eight percent of the patients were diagnosed by clinical features as well as AFB stain and culture. TB, tuberculous.

Fig. 2
Distribution of serum CA-125 levels in patients with tuberculous peritonitis and ovarian epithelial malignancy in Korean women with ascites.
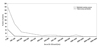
Fig. 3
Proportions of tuberculous peritonitis and ovarian epithelial malignancy by serum CA-125 level. The proportion of patients in the tuberculous peritonitis group begins to decline at the CA-125 level of 800 and suddenly drops to 2.1% at CA-125 levels over 1000 U/mL. TB, tuberculous.

Fig. 4
ROC curve for diagnosing ovarian cancer from tuberculous peritonitis. At the serum CA-125 level of 943, the sum of the sensitivity and specificity was highest. ROC, receiver operating characteristic.
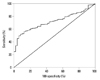
Fig. 5
A case of tuberculous peritonitis. (A) A 68-year old woman came to the hospital with abdominal distention which developed 2 months prior. CT scan was taken and the first impression was peritoneal carcinomatosis. (B) Laparoscopy was done and the histology showed chronic granulomatous inflammation with multinucleated giant cells. (C) No ascites were seen at the follow-up CT scan, 4 months after taking anti-Mycobacterium medication.

References
1. Nossov V, Amneus M, Su F, Lang J, Janco JM, Reddy ST, et al. The early detection of ovarian cancer: from traditional methods to proteomics. Can we really do better than serum CA-125? Am J Obstet Gynecol. 2008; 199:215–223.

2. Ozasa H, Noda Y, Mori T. Progesterone increases serum CA-125 in endometriosis. Fertil Steril. 1987; 47:699–701.

3. Halila H, Stenman UH, Seppälä M. Ovarian cancer antigen CA 125 levels in pelvic inflammatory disease and pregnancy. Cancer. 1986; 57:1327–1329.

4. Jäger W, Diedrich K, Wildt L. Elevated levels of CA-125 in serum of patients suffering from ovarian hyperstimulation syndrome. Fertil Steril. 1987; 48:675–678.

5. Niloff JM, Klug TL, Schaetzl E, Zurawski VR Jr, Knapp RC, Bast RC Jr. Elevation of serum CA125 in carcinomas of the fallopian tube, endometrium, and endocervix. Am J Obstet Gynecol. 1984; 148:1057–1058.

6. Molina R, Filella X, Bruix J, Mengual P, Bosch J, Calvet X, et al. Cancer antigen 125 in serum and ascitic fluid of patients with liver diseases. Clin Chem. 1991; 37:1379–1383.

7. Talbot RW, Jacobsen DJ, Nagorney DM, Malkasian GD, Ritts RE Jr. Temporary elevation of CA 125 after abdominal surgical treatment for benign disease and cancer. Surg Gynecol Obstet. 1989; 168:407–412.
8. Bast RC Jr, Klug TL, St John E, Jenison E, Niloff JM, Lazarus H, et al. A radioimmunoassay using a monoclonal antibody to monitor the course of epithelial ovarian cancer. N Engl J Med. 1983; 309:883–887.

9. Bast RC Jr, Klug TL, Schaetzl E, Lavin P, Niloff JM, Greber TF, et al. Monitoring human ovarian carcinoma with a combination of CA 125, CA 19-9, and carcinoembryonic antigen. Am J Obstet Gynecol. 1984; 149:553–559.

10. Canney PA, Moore M, Wilkinson PM, James RD. Ovarian cancer antigen CA125: a prospective clinical assessment of its role as a tumour marker. Br J Cancer. 1984; 50:765–769.

11. Runyon BA, Montano AA, Akriviadis EA, Antillon MR, Irving MA, McHutchison JG. The serum-ascites albumin gradient is superior to the exudate-transudate concept in the differential diagnosis of ascites. Ann Intern Med. 1992; 117:215–220.

12. Hwangbo Y, Jung JH, Shim J, Kim BH, Jung SH, Lee CK, et al. [Etiologic and laboratory analyses of ascites in patients who underwent diagnostic paracentesis]. Korean J Hepatol. 2007; 13:185–195.
13. Bilgin T, Karabay A, Dolar E, Develioğu OH. Peritoneal tuberculosis with pelvic abdominal mass, ascites and elevated CA 125 mimicking advanced ovarian carcinoma: a series of 10 cases. Int J Gynecol Cancer. 2001; 11:290–294.

14. Vardareli E, Kebapci M, Saricam T, Pasaoglu O, Açikalin M. Tuberculous peritonitis of the wet ascitic type: clinical features and diagnostic value of image-guided peritoneal biopsy. Dig Liver Dis. 2004; 36:199–204.

15. Nistal de Paz F, Herrero Fernández B, Pérez Simón R, Fernández Pérez E, Nistal de Paz C, Ortoll Battle P, et al. Pelvic-peritoneal tuberculosis simulating ovarian carcinoma: report of three cases with elevation of the CA 125. Am J Gastroenterol. 1996; 91:1660–1661.
16. Panoskaltsis TA, Moore DA, Haidopoulos DA, McIndoe AG. Tuberculous peritonitis: part of the differential diagnosis in ovarian cancer. Am J Obstet Gynecol. 2000; 182:740–742.

17. Candocia SA, Locker GY. Elevated serum CA 125 secondary to tuberculous peritonitis. Cancer. 1993; 72:2016–2018.

18. O'Riordan DK, Deery A, Dorman A, Epstein OE. Increased CA 125 in a patient with tuberculous peritonitis: case report and review of published works. Gut. 1995; 36:303–305.
19. Koc S, Beydilli G, Tulunay G, Ocalan R, Boran N, Ozgul N, et al. Peritoneal tuberculosis mimicking advanced ovarian cancer: a retrospective review of 22 cases. Gynecol Oncol. 2006; 103:565–569.

20. Nebhani M, Boumzgou K, Brams S, Laghzaoui M, El Attar H, Bouhya S, et al. [Pelvic tuberculosis mimicking bilateral ovarian tumor. A case report]. J Gynecol Obstet Biol Reprod (Paris). 2004; 33:145–147.
21. Simsek H, Savas MC, Kadayifci A, Tatar G. Elevated serum CA 125 concentration in patients with tuberculous peritonitis: a case-control study. Am J Gastroenterol. 1997; 92:1174–1176.
22. Mas MR, Cömert B, Sağlamkaya U, Yamanel L, Kuzhan O, Ateşkan U, et al. CA-125; a new marker for diagnosis and follow-up of patients with tuberculous peritonitis. Dig Liver Dis. 2000; 32:595–597.

23. Chang DK, Kim JW, Kim BK, Lee KL, Song CS, Han JK, et al. Clinical significance of CT-defined minimal ascites in patients with gastric cancer. World J Gastroenterol. 2005; 11:6587–6592.

24. Jacobs I, Bast RC Jr. The CA 125 tumour-associated antigen: a review of the literature. Hum Reprod. 1989; 4:1–12.

25. Woolas RP, Xu FJ, Jacobs IJ, Yu YH, Daly L, Berchuck A, et al. Elevation of multiple serum markers in patients with stage I ovarian cancer. J Natl Cancer Inst. 1993; 85:1748–1751.

26. Visintin I, Feng Z, Longton G, Ward DC, Alvero AB, Lai Y, et al. Diagnostic markers for early detection of ovarian cancer. Clin Cancer Res. 2008; 14:1065–1072.

27. Wu L, Dai ZY, Qian YH, Shi Y, Liu FJ, Yang C. Diagnostic value of serum human epididymis protein 4 (HE4) in ovarian carcinoma: a systematic review and meta-analysis. Int J Gynecol Cancer. 2012; 22:1106–1112.

28. Kadija S, Stefanovic A, Jeremic K, Radojevic MM, Nikolic L, Markovic I, et al. The utility of human epididymal protein 4, cancer antigen 125, and risk for malignancy algorithm in ovarian cancer and endometriosis. Int J Gynecol Cancer. 2012; 22:238–244.

29. Plestina S, Vrbanec D, Vidmar S, Pulanić D, Herceg D. [Active pelvic-peritoneal tuberculosis with ascites and very high CA-125 level--a case report]. Lijec Vjesn. 2002; 124:71–73.
30. Piura B, Rabinovich A, Leron E, Yanai-Inbar I, Mazor M. Peritoneal tuberculosis mimicking ovarian carcinoma with ascites and elevated serum CA-125: case report and review of literature. Eur J Gynaecol Oncol. 2002; 23:120–122.
31. Thakur V, Mukherjee U, Kumar K. Elevated serum cancer antigen 125 levels in advanced abdominal tuberculosis. Med Oncol. 2001; 18:289–291.

32. Wu JF, Li HJ, Lee PI, Ni YH, Yu SC, Chang MH. Tuberculous peritonitis mimicking peritonitis carcinomatosis: a case report. Eur J Pediatr. 2003; 162:853–855.

33. Younossian AB, Rochat T, Favre L, Janssens JP. Ascites and highly elevated CA-125 levels in a case of peritoneal tuberculosis. Scand J Infect Dis. 2006; 38:216–218.

34. Straughn JM, Robertson MW, Partridge EE. A patient presenting with a pelvic mass, elevated CA-125, and fever. Gynecol Oncol. 2000; 77:471–472.

35. Sheth SS. Elevated CA 125 in advanced abdominal or pelvic tuberculosis. Int J Gynaecol Obstet. 1996; 52:167–171.

36. Jana N, Mukhopadhyay S, Dhali GK. Pelvic tuberculosis with elevated serum CA125: a diagnostic dilemma. J Obstet Gynaecol. 2007; 27:217–218.

37. Tan O, Luchansky E, Rosenman S, Pua T, Azodi M. Peritoneal tuberculosis with elevated serum Ca-125 level mimicking advanced stage ovarian cancer: a case report. Arch Gynecol Obstet. 2009; 280:333–335.

38. Shin HP, Lee JI, Seo HM, Lim SJ, Jung SW, Cha JM, et al. Laparoscopic appearance in a case of peritoneal tuberculosis with elevated cancer antigen 125 levels. Gastrointest Endosc. 2009; 69:180–182.

39. Protopapas A, Milingos S, Diakomanolis E, Elsheikh A, Protogerou A, Mavrommatis K, et al. Miliary tuberculous peritonitis mimicking advanced ovarian cancer. Gynecol Obstet Invest. 2003; 56:89–92.

40. Chow KM, Chow VC, Hung LC, Wong SM, Szeto CC. Tuberculous peritonitis-associated mortality is high among patients waiting for the results of mycobacterial cultures of ascitic fluid samples. Clin Infect Dis. 2002; 35:409–413.

41. Jakubowski A, Elwood RK, Enarson DA. Clinical features of abdominal tuberculosis. J Infect Dis. 1988; 158:687–692.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download