Abstract
Purpose
To investigate the role of low dose rate (LDR) brachytherapy-based multimodal therapy in high-risk prostate cancer (PCa) and analyze its optimal indications.
Materials and Methods
We reviewed the records of 50 high-risk PCa patients [clinical stage ≥T2c, prostate-specific antigen (PSA) >20 ng/mL, or biopsy Gleason score ≥8] who had undergone 125I LDR brachytherapy since April 2007. We excluded those with a follow-up period <3 years. Biochemical recurrence (BCR) followed the Phoenix definition. BCR-free survival rates were compared between the patients with Gleason score ≥9 and Gleason score ≤8.
Results
The mean initial PSA was 22.1 ng/mL, and mean D90 was 244.3 Gy. During a median follow-up of 39.2 months, biochemical control was obtained in 72% (36/50) of the total patients; The estimated 3-year BCR-free survival was 92% for the patients with biopsy Gleason scores ≤8, and 40% for those with Gleason scores ≥9 (p<0.001). In Cox multivariate analysis, only Gleason score ≥9 was observed to be significantly associated with BCR (p=0.021). Acute and late grade ≥3 toxicities were observed in 20% (10/50) and 36% (18/50) patients, respectively.
Conclusion
Our results showed that 125I LDR brachytherapy-based multimodal therapy in high-risk PCa produced encouraging relatively long-term results among the Asian population, especially in patients with Gleason score ≤8. Despite small number of subjects, biopsy Gleason score ≥9 was a significant predictor of BCR among high risk PCa patients after brachytherapy.
The wide application of prostate-specific antigen (PSA)-based screening has led to a profound shift in the staging of prostate cancer (PCa).1 Although the vast majority of newly diagnosed PCa exhibit clinically localized disease, 15% of patients still present with high-risk tumors, and PCa remains a leading cause of cancer death.2,3 Men with high-risk disease are at the greatest risk for biochemical failure and prostate-cancer-related death; however, the effective management of high-risk PCa presents a significant clinical challenge to the physicians involved and remains controversial.4 The mainstay of treatment typically involves a combination of long-term androgen-deprivation therapy (ADT) with external beam radiation therapy (EBRT). Randomized trials have shown improved overall survival associated with this combination; however, even with this approach, more than half of patients experience disease recurrence.5,6
In 1998, D'Amico, et al.7 proposed a risk classification scheme for PCa, patients whose PSA level >20 ng/mL, Gleason score of 8-10, or clinical stage ≥T2c were included in high risk group. After validatation these risk classification via numerous studies, D'Amico risk classification is currently used in the litherature; however, the major shift among these risk groups over time suggests that the clinical relevance of this classification scheme may be diminishing. Moreover, this model is limited by the equal weight assigned to each factor and by the arbitrary selection of cutoffs for each risk factor.8 A relatively favorable prognosis was observed in high-risk PCa patients with low Gleason scores compared to those with high Gleason scores.9
Although prostate brachytherapy remains one of the first-line treatment options for men with clinically localized PCa, brachytherapy in high-risk PCa was reported only in higher volume centers.10,11 Therefore, we investigated the role of brachytherapy in high-risk PCa and analyzed its optimal indications.
With approval from the institutional review board, we reviewed the records of high-risk PCa patients who had undergone prostate 125I low-dose rate (LDR) brachytherapy at our clinic since April 2007. The D'Amico risk group classification was used: clinical stage ≥T2c, PSA >20 ng/mL or biopsy Gleason score ≥8. We excluded those patients with a follow-up period <3 years. A total of 50 patients were included in our study. All the patients were assessed based on their clinical history, physical examination, transrectal ultrasound (TRUS) scan, uroflowmetry and pre-treatment International Prostate Symptom Score. Pelvic magnetic resonance imaging, abdominal and pelvic computed tomography (CT) and bone scans were performed if clinically indicated. Biochemical recurrence (BCR) followed the Phoenix definition (i.e., a post-treatment nadir plus 2.0 ng/mL).12
Permanent 125I seeds were implanted into the prostate. All procedures were performed in the operating theater under spinal anesthesia. Preplanning included volumetric study of the prostate, which was performed by transrectal ultrasound (Rosses Medical System, Inc., Columbia, MD, USA) using a specific module for prostate brachytherapy. The images of the prostate were obtained in 5-mm transverse increments from the base to the apex and transferred to I-plant TPS® (CMS, Inc., St. Louis, MO, USA). The planned target volume is defined by a 5-mm margin around the anterior and lateral prostate capsule. No posterior prostate margin is drawn so as to protect the rectum. Seeds are introduced in strategic positions previously defined and optimized by the urologist and radiation oncologist using I-plant TPS®. A template with an alphanumeric grading allows for the implantation of each radioactive source at predetermined coordinates. The prescribed doses were 145 Gy which was suggested in American Association of Physicists in Medicine Task Group 6413 and the European Society for Therapeutic Radiology and Oncology/European Association of Urology/European Organisation for Research and Treatment Cancer (ESTRO/EAU/EORTC) recommendations on prostate brachytherapy.14 In most cases, more seeds were implanted for strict tumor control than planned in preplan. In 14 patients combined with EBRT, the prescribed doses were adjusted to 110 Gy.
The technical quality of the implant and quantified radiation doses to the bladder and adjacent rectum were evaluated by post-implant dosimetry. Post-implant CT scan dosimetry was performed at 1 month after operation. Tomographic images of the pelvis outlining the prostate, urethra, rectum, and bladder were transferred to iPlan radiation therapy (RT) image software (Brain LAB AG, Heimstetten, Germany), which calculated the final doses of radiation to these organs as well as the volume of prostate receiving 100% and 150% of the radiation dose (V100 and V150), respectively and the dose to 90% of the prostate (D90). The criteria for post-implant dosimetric adequacy included a V100 >80%, a D90 >90%, and a V150 <60% for 125I.15
Of the 50 patients, 14 individuals (28%), who had an initial prostatic volume over 50 mL, received neoadjuvant ADT with oral anti-androgen therapy in an effort to decrease prostate volume. Forty-eight patients (96%) received adjuvant ADT for 1.7 months on average. 28 patients with Gleason score ≥8 (56%) received adjuvant EBRT. The planned target volumes included the prostate and seminal vesicles, with a 5-mm margin in all directions. The radiation treatment was performed by 3-D conformal or intensity-modulated RT. The total dose administered to the planned target volume was 50-50.4 Gy, applied in daily fractions of 1.8-2 Gy over 5.5 weeks.
Patients were followed up at 3-month intervals with total PSA measurements; clinical, laboratory, and radiologic examinations were performed as needed. Toxicity was scored using the Radiation Therapy Oncology Group (RTOG) toxicity criteria.16
The SPSS software package version 15.0 (Statistical Package for Social SciencesTM, Chicago, IL, USA) was used for statistical analysis. Continuous variables were compared using the Mann-Whitney test, and categorical variables were compared via the chi-squared or Fisher's exact tests. A significance level of 5% probability (p<0.05) and a 95% confidence interval were adopted. BCR-free survival curves were generated using the Kaplan-Meier method, and the log-rank test was used for comparison. The potential predictors of BCR were analyzed via multivariate Cox proportional hazard regression analysis.
Of the 50 high-risk PCa patients who underwent 125I LDR brachytherapy, the mean age was 68.8±6.1 years, the mean TRUS volume was 34.45±12.56 mL, and the initial mean PSA was 22.21±27.51 ng/mL. Twenty patients (40%) had biopsy Gleason score ≥9, whereas the other 30 patients (60%) had biopsy Gleason scores ≤8. Forty-eight patients (96%) received ADT, and 28 patients (56%) received adjuvant EBRT. Among the patients with biopsy Gleason scores ≤8, 28 (93.3%) had received ADT (oral anti-androgen) with median duration of 4 months, and 8 patients (26.7%) had received EBRT with median of 45 Gy. All patients with Gleason score ≥9 had received adjuvant ADT and EBRT both.
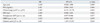
As can be seen in Table 1, patients with biopsy Gleason scores ≥9 had significantly higher PSA levels (p=0.001) and exhibited a higher rate of BCR (12; 60%) than those with a biopsy Gleason scores ≤8 (2; 6.7%) (p=0.007). Furthermore, a high proportion of these patients underwent adjuvant EBRT (p<0.001). Meanwhile, the two groups of patients showed no significant differences in age, prostate volume or clinical stage. The number of inserted seeds (94.3 vs. 89.6, p=0.556), mean D90 (Gy) (247.2 Gy vs. 240.0 Gy, p=0.716), mean D90 (%) (188.3% vs. 202.2%, p=0.407) and mean V100 (%) (99.9% vs. 99.8%, p=0.605) did not differ significantly between the groups.
At a median follow-up of 39.2 months, 14 patients (28%) had BCR. One cancer-specific mortality was observed. The BCR-free survival was significantly higher in patients with biopsy Gleason scores ≤8 compared to those with Gleason scores ≥9 (log-rank, p<0.001) (Fig. 1). The estimated 3-year BCR-free survival was 92% for the patients with biopsy Gleason scores ≤8, and 40% for those with Gleason scores ≥9.
Table 2 presents a multivariate Cox proportional hazard regression analysis, showing that only the Gleason score was a significant predictor for BCR (HR=6.601, 95% CI: 1.419-15.253, p=0.024). Other factors, such as age, PSA, clinical stage, and amount of D90 and EBRT, were not significant.
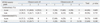
The comprehensive rates of toxicities are described in Table 3. Acute (<3 months) and late (>3 months) genitourinary (GU) toxicities were observed in 44 (88%) and 48 (96%) patients, respectively. Most of them were irritative voiding symptoms and were controlled by medication. RTOG grade 3 GU toxicities were observed in 10 patients during the acute period and in 16 patients during the late period. No significant difference was observed according to Gleason score. Acute and late gastrointestinal (GI) toxicities were observed in 38 (76%) and 32 (64%) patients, respectively. Most cases of acute GI toxicities were grade less than 3, which were rectal discomforts. One third of late GI toxicities were intermittent rectal bleeding, controlled by oral medications such as mesalamine. One recto-urethral fistula (grade 4) was developed in the group of Gleason score ≥9, and managed by surgical repair with gracilis muscle interposition in other institution. Another hemorrhagic ulceration (grade 4) requiring interventional procedure occurred in the group of Gleason score ≥9.
Prostate brachytherapy has been conducted at only a single institution in Korea since April 2007. In total, 250 patients with PCa received brachytherapy. This report is the first to present results from Korea, which can be used to interpret racial differences among patients treated with brachytherapy. In this study, a biopsy Gleason score ≥9 among patients with high-risk PCa was observed to be a significant predictor of BCR following 125I LDR brachytherapy. Although several patients with biopsy Gleason scores <8 and PSA >20 ng/mL or clinical stage ≥T2c were classified as a high-risk group according to the D'Amico criteria, their estimated 3-year BCR rate was 92%, which is significantly better than those reported for Gleason scores ≥9.
Among patients with high-risk disease, biochemical control varies by treatment modality. Biochemical control at 5 years ranged from 32% to 60% for radical prostatectomy,7,17,18 12-47% for EBRT alone7,18,19 and 16-54% for brachytherapy alone.17-20 However, the patients with high-risk PCa generally had more favorable treatment outcomes following multimodal treatment. Stone, et al.21 suggested that high-risk PCa treated with a combination of EBRT and permanent seed implantation improved biochemical disease-free survival, metastasis-free survival, and overall survival. Furthermore, da Silva Franca, et al.22 demonstrated the benefits of a combined approach for cases with poor prognoses. Their analyses of the clinical parameters of the group treated with a combination of EBRT plus brachytherapy and the group treated by brachytherapy alone showed that 71% of patients in the combination therapy group were high-risk, and that 36% of the patients in the brachytherapy-only group were high-risk (p=0.003). The Seattle study, which combined EBRT+brachytherapy in high-risk PCa patients, also reported a BCR-free survival rate of 62.2% at both 5 and 10 years.11 In our preliminary study, the estimated 3-year BCR-free rate was observed to be 70.8%, which is similar to other results from large-scale studies.
Interestingly, the patients with biopsy Gleason scores ≥9 had significantly lower biochemical control rates despite the combination of EBRT and brachytherapy. Therefore, we concluded that high-risk PCa, as defined by the D'Amico classification, did not lead to the creation of a homogenous group; in particular, patients with higher Gleason scores represented a "very-high-risk" group within the "high-risk" group. Actually, as seen in the radical prostatectomy cohort, high-risk PCa patients showed nearly 50% disease-free survival rate at 5 years after surgery alone.23 Loeb, et al.24 reported that a high biopsy Gleason score was the strongest independent predictor of BCR, metastasis, and PCa death among high-risk patients.
The American Brachytherapy Society strongly recommends CT-based post-implant prostate dosimetry with quality cut-off points of V100 >80% and D90 >90%. Dosimetric implant quality is essential for the optimization of biochemical outcomes15: previous reports showed a statistically significant relationship between dosimetric parameters and biochemical controls because patients without BCR were those with better dosimetric values.21,22 Among several studies about prostate brachytherapy, the optimal dose had been widely investigated, D90 dose of 144 Gy was considered optimal prescription dose for 125I implants.25 However, D90 doses of over 180 Gy with modified peripheral loading among prostate brachytherapy did not increase normal tissue toxicity. This suggests that a dose of 160 Gy may have a benefit to ensure a minimal D90 dose of 144 Gy.26 The concept that higher prostate doses can be achieved through the use of EBRT and brachytherapy has been studied using the biologically effective dose concept. In a recent study, biologically effective doses of over 150 Gy were found to be associated with a significantly higher rate of biochemical control.27 In our studies, the mean D90 value was 244.3 Gy (167.5-357.5 Gy) and the percent of D90 was 193.8% (136.2-252.2%) which is much higher than those in other studies. Although there is a concern regarding complications, high-energy transfer may result in effective tumor control: with high D90, BCR did not differ significantly between the groups treated with brachytherapy alone and brachytherapy with combined EBRT (p=0.094). For the same reason, EBRT was not a significant predictor of BCR in the current multivariate Cox proportional analysis (HR=1.032, p=0.059).
The toxicities in our series were higher than those in other series. Schafer, et al.28 showed that only 10.4% and 1% of men reported moderate and severe urinary symptoms, respectively, whereas Koontz, et al.29 reported that acute GU toxicity and GI toxicity occurred in approximately 80% and 24% of patients, respectively, and that late GU toxicity and GI toxicity occurred in 21% and 38% of patients, respectively. In our series, late GU toxicity was observed in nearly 96% of all patients, but 65% of them were classified as RTOG toxicity grade <3, which was controlled by medication. Late GI toxicity was observed in 64% of the patients in our series, which is higher than values reported by other studies. One patient experienced grade 4 GI toxicity, with recto-urethral fistula requiring surgical repair. Although there was higher incidence of complication rates because of the high D90 level, most patients managed to lead normal social lives. In more recent cases, we tried to avoid insertion of seed near the urethra and rectum. Thus, we inserted accurate seed amount to suspicious cancerous lesion near the urethra or rectum using calculation using real time planning system. Further advanced radiologic equipments to find accurate cancer lesion in prostate may be helpful for reducing these problems.
The main limitation of our study may be small number of patients included. However, this study represents the only report of high-risk PCa after brachytherapy in Korea. Another limitation of our study was that the D90 range was wide and the D90 level was high compared with other brachytherapy series. If the safety profile is stabilized over a longer follow-up period, the prospective data gathered here will further increase in value. Additional investigation is required.
In conclusion, our results showed that 125I LDR prostate brachytherapy-based multimodal therapy in high-risk PCa produced encouraging long-term results among the Asian population, especially in patients with Gleason scores ≤8. The biopsy Gleason scores ≥9 was the only significant predictor of BCR among high risk PCa patients treated with brachytherapy after controlling other variables. Despite small number of subjects, the present results represent the only such report from Korea. Therefore, further efforts should be made to identify appropriate predictors for brachytherapy among high-risk PCa groups through studies with larger, prospective cohorts.
Figures and Tables
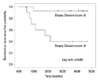 | Fig. 1Kaplan Meier survival curve according to biopsy Gleason score among high-risk prostate cancer patients who underwent 125I low dose rate brachytherapy. |
References
1. Stamey TA, Caldwell M, McNeal JE, Nolley R, Hemenez M, Downs J. The prostate specific antigen era in the United States is over for prostate cancer: what happened in the last 20 years? J Urol. 2004; 172(4 Pt 1):1297–1301.

2. Cooperberg MR, Lubeck DP, Mehta SS, Carroll PR. CaPSURE. Time trends in clinical risk stratification for prostate cancer: implications for outcomes (data from CaPSURE). J Urol. 2003; 170(6 Pt 2):S21–S25.

3. Fang LC, Merrick GS, Butler WM, Galbreath RW, Murray BC, Reed JL, et al. High-risk prostate cancer with Gleason score 8-10 and PSA level ≤15 ng/mL treated with permanent interstitial brachytherapy. Int J Radiat Oncol Biol Phys. 2011; 81:992–996.

4. Dibiase SJ, Hussain A, Kataria R, Amin P, Bassi S, Dawson N, et al. Long-term results of a prospective, Phase II study of long-term androgen ablation, pelvic radiotherapy, brachytherapy boost, and adjuvant docetaxel in patients with high-risk prostate cancer. Int J Radiat Oncol Biol Phys. 2011; 81:732–736.

5. Bolla M, Collette L, Blank L, Warde P, Dubois JB, Mirimanoff RO, et al. Long-term results with immediate androgen suppression and external irradiation in patients with locally advanced prostate cancer (an EORTC study): a phase III randomised trial. Lancet. 2002; 360:103–106.

6. Horwitz EM, Bae K, Hanks GE, Porter A, Grignon DJ, Brereton HD, et al. Ten-year follow-up of radiation therapy oncology group protocol 92-02: a phase III trial of the duration of elective androgen deprivation in locally advanced prostate cancer. J Clin Oncol. 2008; 26:2497–2504.

7. D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998; 280:969–974.
8. Yossepowitch O, Eastham JA. Radical prostatectomy for high-risk prostate cancer. World J Urol. 2008; 26:219–224.

9. Yossepowitch O, Eggener SE, Serio AM, Carver BS, Bianco FJ Jr, Scardino PT, et al. Secondary therapy, metastatic progression, and cancer-specific mortality in men with clinically high-risk prostate cancer treated with radical prostatectomy. Eur Urol. 2008; 53:950–959.

10. Merrick GS, Butler WM, Wallner KE, Galbreath RW, Allen ZA, Adamovich E. Androgen-deprivation therapy does not impact cause-specific or overall survival after permanent prostate brachytherapy. Int J Radiat Oncol Biol Phys. 2006; 65:669–677.

11. Sylvester JE, Grimm PD, Blasko JC, Millar J, Orio PF 3rd, Skoglund S, et al. 15-Year biochemical relapse free survival in clinical Stage T1-T3 prostate cancer following combined external beam radiotherapy and brachytherapy; Seattle experience. Int J Radiat Oncol Biol Phys. 2007; 67:57–64.

12. Roach M 3rd, Hanks G, Thames H Jr, Schellhammer P, Shipley WU, Sokol GH, et al. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int J Radiat Oncol Biol Phys. 2006; 65:965–974.

13. Yu Y, Anderson LL, Li Z, Mellenberg DE, Nath R, Schell MC, et al. Permanent prostate seed implant brachytherapy: report of the American Association of Physicists in Medicine Task Group No. 64. Med Phys. 1999; 26:2054–2076.

14. Salembier C, Lavagnini P, Nickers P, Mangili P, Rijnders A, Polo A, et al. Tumour and target volumes in permanent prostate brachytherapy: a supplement to the ESTRO/EAU/EORTC recommendations on prostate brachytherapy. Radiother Oncol. 2007; 83:3–10.

15. Merrick GS, Grimm PD, Sylvester J, Blasko JC, Butler WM, Allen ZA, et al. Initial analysis of Pro-Qura: a multi-institutional database of prostate brachytherapy dosimetry. Brachytherapy. 2007; 6:9–15.

16. Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995; 31:1341–1346.

17. Fletcher SG, Mills SE, Smolkin ME, Theodorescu D. Case-matched comparison of contemporary radiation therapy to surgery in patients with locally advanced prostate cancer. Int J Radiat Oncol Biol Phys. 2006; 66:1092–1099.

18. Stokes SH. Comparison of biochemical disease-free survival of patients with localized carcinoma of the prostate undergoing radical prostatectomy, transperineal ultrasound-guided radioactive seed implantation, or definitive external beam irradiation. Int J Radiat Oncol Biol Phys. 2000; 47:129–136.

19. Zelefsky MJ, Hollister T, Raben A, Matthews S, Wallner KE. Five-year biochemical outcome and toxicity with transperineal CT-planned permanent I-125 prostate implantation for patients with localized prostate cancer. Int J Radiat Oncol Biol Phys. 2000; 47:1261–1266.

20. Dattoli M, Wallner K, True L, Cash J, Sorace R. Long-term outcomes after treatment with brachytherapy and supplemental conformal radiation for prostate cancer patients having intermediate and high-risk features. Cancer. 2007; 110:551–555.

21. Stone NN, Potters L, Davis BJ, Ciezki JP, Zelefsky MJ, Roach M, et al. Multicenter analysis of effect of high biologic effective dose on biochemical failure and survival outcomes in patients with Gleason score 7-10 prostate cancer treated with permanent prostate brachytherapy. Int J Radiat Oncol Biol Phys. 2009; 73:341–346.

22. da Silva Franca CA, Vieira SL, Carvalho AC, Bernabé AJ, Penna AB. Localized prostate cancer with intermediate- or high-risk features treated with combined external beam radiotherapy and iodine-125 seed brachytherapy. Brachytherapy. 2010; 9:307–312.

23. Tareen B, Kimmel J, Huang WC. Contemporary treatment of high-risk localized prostate cancer. Expert Rev Anticancer Ther. 2010; 10:1069–1076.

24. Loeb S, Schaeffer EM, Trock BJ, Epstein JI, Humphreys EB, Walsh PC. What are the outcomes of radical prostatectomy for high-risk prostate cancer? Urology. 2010; 76:710–714.

25. Stock RG, Stone NN, Tabert A, Iannuzzi C, DeWyngaert JK. A dose-response study for I-125 prostate implants. Int J Radiat Oncol Biol Phys. 1998; 41:101–108.

26. Kao J, Stone NN, Lavaf A, Dumane V, Cesaretti JA, Stock RG. (125)I monotherapy using D90 implant doses of 180 Gy or greater. Int J Radiat Oncol Biol Phys. 2008; 70:96–101.

27. Ho AY, Burri RJ, Cesaretti JA, Stone NN, Stock RG. Radiation dose predicts for biochemical control in intermediate-risk prostate cancer patients treated with low-dose-rate brachytherapy. Int J Radiat Oncol Biol Phys. 2009; 75:16–22.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download