Abstract
Purpose
To investigate the relationship between prostate volume and the increased risk for being diagnosed with prostate cancer (PCa) in men with slowly increasing prostate specific antigen (PSA).
Materials and Methods
A cohort of 1035 men who visited our hospital's health promotion center and were checked for serum PSA levels more than two times between January 2001 and November 2011 were included. Among them, 116 patients had a change in PSA levels from less than 4 ng/mL to more than 4 ng/mL and underwent transrectal ultrasound guided prostate biopsy. Median age was 55.9 years and 26 (22.4%) had PCa. We compared the initial PSA level, the last PSA level, age, prostate volume, PSA density (PSAD), PSA velocity, and follow-up period between men with and without PCa. The mean follow-up period was 83.7 months.
Results
Significant predictive factors for the detection of prostate cancer identified by univariate analysis were prostate volume, follow-up period and PSAD. In the multivariate analysis, prostate volume (p<0.001, odds ratio: 0.890) was the most significant factor for the detection of prostate cancer. In the receiver operator characteristic curve of prostate volume, area under curve was 0.724. At the cut-off value of 28.8 mL for prostate volume, the sensitivity and specificity were 61.1% and 73.1% respectively.
At present, a prostate specific antigen (PSA) level of 4 ng/mL is widely used as the cutoff value for recommendation of a prostate biopsy. In this cutoff value, the sensitivity is 67.5-80%, but the specificity is only 20-30%.1-3 Other indexes such as PSA velocity (PSAV) and PSA density (PSAD) were introduced thereafter in order to compensate the low specificity of PSA level, and several previous studies proved the effectiveness of these new indexes for the early detection of prostate cancer (PCa).4,5 However, despite a possible relationship between these indexes and PCa, the roles of these indexes in early detection of PCa remains a matter of controversy.6-8
To compensate the low specificity of PSA level and to confirm other important factors for PCa detection at biopsy, we investigated the relationship between various factors including the initial and last PSA level, age, PSAV, PSAD, prostate volume, and follow-up period and outcomes of prostate biopsy through cumulative PSA follow-up data of a cohort in our hospital's health promotion center.
The current study was a single center, retrospective analysis. A cohort of 1035 men who visited our hospital's health promotion center and were tested for their serum PSA levels more than two times between January 2001 and November 2011 were the subjects of this study. Among them, 17 men with an elevated PSA level due to chronic prostatitis or with a history of 5-α-reductase use for benign prostate hyperplasia treatment were excluded from this study. Finally, 116 men who had a change in the PSA level from less than 4 ng/mL to more than 4 ng/mL underwent transrectal ultrasound (TRUS) guided prostate biopsy. Median age was 55.9 years (range 41-78). The mean follow-up period was 83.7 months (range 12-127).
PSA levels were measured by using ARCHITECT total PSA assay (Abbott Diagnostics inc., Abbott Park, IL, USA) in our hospital. Levels were measured before digital rectal examination or TRUS to minimize interference. Prostate volume was calculated by the ellipsoid formula, [(π/6)×(width of the maximal transverse dimension)×(length of the maximal anteroposterior dimension)×(height of the maximal superoinferior dimension)], using values obtained from TRUS (HDI 3500, Philips Medical Systems, Seattle, WA, USA). The height, width and length of a prostate were measured from two orthogonal views (e.g. transverse and sagittal plane) with two-dimensional ultrasound in this study. The 12-core biopsy scheme was used in our institution including a standard sextant, which was originally described by Hodge, et al.9 and three core biopsies was used in case of hypoechoic lesions on TRUS. Biopsies were performed under ultrasound guidance using an 20-gauge, 22 mm, BARD® Magnum® reusable core biopsy instrument (C.R Bard inc., Murray Hill, NJ, USA). PSAV was calculated by using two-point simple method, and defined as [PSAV=(PSA level of last visit-PSA level of initial visit)/follow-up period]. PSAD was defined as [PSAD=PSA/prostate volume]. We used prostate volume and PSAD measured by TRUS at the time of prostate biopsy.
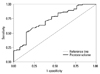
Between the PCa group and the non-PCa group, the initial PSA level, the last PSA level, the age, the prostate volume, the PSAD, the PSAV and the follow-up period were compared by Mann-Whitney U test (Table 1). To identify the predictive factors for PCa, univariate and multivariate logistic regression analysis with enter selection were conducted (Table 2). Odds ratios (ORs) and 95% confidential intervals for all covariatives were calculated. Predictive accuracy was quantified using the area under the curve (AUC) of the receiver operator characteristic (ROC) analysis (Fig. 1).10 SPSS 12.0 (SPSS Inc., Chicago, IL, USA) software was used for the statistical analyses. A p-value <0.05 was considered statistically significant. The Institutional Review Board of our medical institution approved this study (IRB No. 2013-023).
Of the 116 men, 26 (22.4%) were diagnosed with PCa by prostate biopsy. The PCa detection rates between PSA levels of 4.1-10.0 ng/mL was 18% (18 of 98 patients) and PCa detection rate in PSA levels over 10 ng/mL was 47% (8 of 18 patients).
The mean initial PSA and last PSA level during the follow-up was 1.91 and 8.07 ng/mL, respectively. The mean PSAV was 1.16 ng/mL/year (range 0.06-20.99). The mean prostate volume was 34.3 mL (range 9.7-106.0) and the mean PSAD was 0.28 ng/mL/mL (range 0.05-2.43).
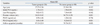
Of the evaluated variables, the prostate volume at biopsy (36.7 mL vs. 26.0 mL, p=0.002), the PSAD at biopsy (0.24 ng/mL/mL vs. 0.41 ng/mL/mL, p=0.001) and the follow-up interval (79 months vs. 97 months) were significantly different (Table 1). On the other hand, there was no significant difference in the initial PSA, last PSA, PSAV and age between the two groups.
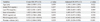
We conducted univariate and multivariate logistic regression analysis to identify the predictive factors for PCa in prostate needle biopsy. In the univariate logistic regression analysis, prostate volume (p<0.001, OR=0.916), PSAD (p=0.046, OR=3.322) and follow-up period (p=0.010, OR=1.025) were identified as significant predictive factors. Among these, prostate volume (p<0.001, OR=0.891) and age (p=0.022, OR=1.149) were identified as significant factors in multivariate logistic regression analysis (Table 2). Although PSAD was statistically significant in the univariate analysis, the result was challenged by the multivariate analysis. The AUC of prostate volume was 0.724 (Fig. 1). At 28.8 mL of prostate volume, the sensitivity and the specificity were 61.1% and 73.1%, respectively.
Although PSA measurement has contributed to the early detection and treatment of PCa, PSA may be elevated in other non-malignant conditions such as benign prostatic hypertrophy and prostatitis, I addition, the specificity of PSA for PCa is less than ideal. Therefore, PSA cutoff values for PCa diagnosis is still controversial and decision-making on the performance of a prostate biopsy based on only PSA cutoff values has clinical limitations considering the relative low specificity of PSA. Many studies have been conducted to determine an appropriate PSA cutoff value for PCa detection. Catalona, et al.11 reported that a PSA level of 4 ng/mL or higher was appropriate as the PSA cutoff value for screening of PCa. It is suggested that lowering the PSA cutoff value from 4 to 2-3 ng/mL is appropriate because high PCa detection rate is demonstrated in those range of PSA. PSA cutoff value from 4 to 2.5 ng/mL results in an increase in the number of men who undergo biopsy and may result in an increased detection of potentially insignificant PCa.12 The adequate PSA cutoff value for prostate biopsy remains controversial. At the cutoff value of 4 ng/mL for PSA, the sensitivity is 67.5-80% and the specificity is only 20-30%. Another study reported the sensitivity and specificity of PSA were about 79% and 59% respectively.13 According to a study by Schmid, et al.,14 the PCa detection rate between PSA levels of 4.1-10.0 ng/mL is 25% and PSA levels of over 10 ng/mL has a detection rate of 50-60%. In our study, the PCa detection rate between PSA levels of 4.1-10.0 ng/mL was 18% and PSA levels of over 10 ng/mL has a detection rate of 47%, which is lower than the detection rates reported by Schmid, et al.14 The lower detection rate of PCa in Korea is likely attributable to the lower morbidity of PCa. However, our result was slightly higher than the PCa detection rate of 15.9% reported by Lee, et al.15 in patients with a PSA of 4.1-10.0 ng/mL in Korea. The low specificity of PSA and the relative low detection rate of PCa in this gray zone, have raised a question as to whether the strategy of prostate biopsy simply based on PSA cutoff values is sufficient for selecting suitable candidates for prostate biopsy. To compensate for the limitations of PSA, many potential predictive factors for PCa in biopsy such as PSAD, PSAV, age-adjusted PSA level and the ratio of free-PSA have been introduced.1 Recently, PSA-age volume, volume of transitional zone, and PSA-transitional volume density have been investigated.16,17
In the current study, there was a statistically significant difference in prostate volume, PSAD and the follow-up period between the two groups. Prostate volume was identified as a significant predictive factor of PCa detection in both the Student's t-test and multivariate logistic regression test. This is supported by the prostate volume AUC of 0.724 in the ROC curve (Fig. 1). Al-Azab, et al.18 also reported that a smaller prostate size was associated with PCa patients with PSA of 2.0-9.0 ng/mL. Other studies also demonstrated significant differences in the prostate volume between the patients with and without PCa.19-21 High PSA levels are positively related to PCa at biopsy, but a large prostate volume has a negative relationship. Prostate volume, itself is related to serum PSA and age.21 It is thought that high PCa detection in small prostate volume is caused by a relatively large PCa volume in normal prostate.
PSAD also has been introduced as a useful tool to increase the specificity in the early detection of PCa.22 In the current study, PSAD was statistically significant in the univariate analysis but the result was challenged by the multivariate analysis. It was reported that performing a prostate biopsy when the levels of PSAD is greater than 0.15 ng/mL/mL increases the cancer detection rate and can safely reduce the number of patients undergoing prostate biopsy without significantly compromising the cancer detection.23,24 The usefulness of PSAD for PCa detection is widely accepted in the PSA range of 4.0-10.0 ng/mL; however, this has been controversial and it's advantages have not been fully accepted.25,26 Prospective multi-center studies with a larger number of patients are needed to firmly establish the usefulness of PSAD.
Our study had some limitations. First, the sample size was relatively small and there was a lack of diversity in the subjects because the subjects were selected from a single hospital. Second, we only considered the first prostate biopsy. We were not able to reflect the results of repeated biopsies due to a considerable number being lost to follow-up and potential ethical issues. Among patients who were not diagnosed with PCa in the initial biopsy, 20% were diagnosed with PCa in repeated prostate biopsy.27 Third, we measured prostate volumes by means of TRUS and several experienced radiologists, not by prostatectomy specimens and only one experienced radiologist. This could be associated with inter- or intra- observer variability due to the subjective aspects of probe placement and choice of planar dimensions for measurement. If any error was made in measuring the height, width or length of the prostate by TRUS, the accuracy of prostate volume and PSAD would be reduced. However, TRUS is widely used to calculate prostate volume and is considered a reliable technique to estimate prostate size, with accuracy within 20% of the pathological weight.28 Moreover, a significant intra-observer variation in TRUS-guided prostate volume measurement could also exist even among highly experience radiologists. However, this variability is not enough to affect one's eligibility for PCa active surveillance strategy when PSAD criteria are used.29 Therefore, TRUS-guided prostate volume measurements is a reliable method of assessing prostate volume and PSAD in patients with PCa.
In men with PSA values more than 4 ng/mL during the periodic follow-up, a small prostate volume is the most important factor in the early detection of prostate cancer. It is suggested that clinicians should pay greater attention to patients with a prostate volume less than 28.8 mL as well as high PSA levels more than 4 ng/mL.
Figures and Tables
Fig. 1
Receiver operating characteristic curve for prostate volume. Area under curve was 0.724. At 28.8 mL of prostate volume, the sensitivity and the specificity were 61.1% and 73.1% respectively.
ACKNOWLEDGEMENTS
This work was supported by Priority Research Center Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2009-0094050).
References
1. Shariat SF, Scardino PT, Lilja H. Screening for prostate cancer: an update. Can J Urol. 2008; 15:4363–4374.
2. Bunting PS. Screening for prostate cancer with prostate-specific antigen: beware the biases. Clin Chim Acta. 2002; 315:71–97.

3. Schilsky RL, Taube SE. Tumor markers as clinical cancer tests--are we there yet? Semin Oncol. 2002; 29:211–212.
4. Carter HB, Pearson JD, Metter EJ, Brant LJ, Chan DW, Andres R, et al. Longitudinal evaluation of prostate-specific antigen levels in men with and without prostate disease. JAMA. 1992; 267:2215–2220.

5. Loeb S, Roehl KA, Catalona WJ, Nadler RB. Prostate specific antigen velocity threshold for predicting prostate cancer in young men. J Urol. 2007; 177:899–902.

6. Schröder FH, Roobol MJ, van der Kwast TH, Kranse R, Bangma CH. Does PSA velocity predict prostate cancer in pre-screened populations? Eur Urol. 2006; 49:460–465.

7. Vickers AJ, Wolters T, Savage CJ, Cronin AM, O'Brien MF, Pettersson K, et al. Prostate-specific antigen velocity for early detection of prostate cancer: result from a large, representative, population-based cohort. Eur Urol. 2009; 56:753–760.

8. Vickers AJ, Savage C, O'Brien MF, Lilja H. Systematic review of pretreatment prostate-specific antigen velocity and doubling time as predictors for prostate cancer. J Clin Oncol. 2009; 27:398–403.

9. Hodge KK, McNeal JE, Terris MK, Stamey TA. Random systematic versus directed ultrasound guided transrectal core biopsies of the prostate. J Urol. 1989; 142:71–74.

10. Steyerberg EW, Vickers AJ, Cook NR, Gerds T, Gonen M, Obuchowski N, et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology. 2010; 21:128–138.
11. Catalona WJ, Smith DS, Ratliff TL, Basler JW. Detection of organ-confined prostate cancer is increased through prostate-specific antigen-based screening. JAMA. 1993; 270:948–954.

12. Müntener M, Kunz U, Eichler K, Puhan M, Schmid DM, Sulser T, et al. Lowering the PSA threshold for prostate biopsy from 4 to 2.5 ng/ml: influence on cancer characteristics and number of men needed to biopt. Urol Int. 2010; 84:141–146.

13. Antenor JA, Han M, Roehl KA, Nadler RB, Catalona WJ. Relationship between initial prostate specific antigen level and subsequent prostate cancer detection in a longitudinal screening study. J Urol. 2004; 172:90–93.

14. Schmid HP, Riesen W, Prikler L. Update on screening for prostate cancer with prostate-specific antigen. Crit Rev Oncol Hematol. 2004; 50:71–78.

15. Lee DH, Yang WJ, Chung BH, Kim SI, Kim SJ, Kim YS, et al. A multicenter study of the detection rate for prostate cancer according to the serum prostate-specific antigen level in Korean men. Korean J Urol. 2005; 46:433–437.
16. Patel S, Issa MM, El-Galley R. Evaluation of novel formula of PSA, age, prostate volume, and race in predicting positive prostate biopsy findings. Urology. 2013; 81:602–606.

17. Qi TY, Chen YQ, Jiang J, Zhu YK, Yao XH, Wang XJ. Utility of the transition zone index for identification of prostate cancer in Chinese men with intermediate PSA levels. Int Urol Nephrol. 2012; 44:807–815.

18. Al-Azab R, Toi A, Lockwood G, Kulkarni GS, Fleshner N. Prostate volume is strongest predictor of cancer diagnosis at transrectal ultrasound-guided prostate biopsy with prostate-specific antigen values between 2.0 and 9.0 ng/mL. Urology. 2007; 69:103–107.

19. Stephan C, Stroebel G, Heinau M, Lenz A, Roemer A, Lein M, et al. The ratio of prostate-specific antigen (PSA) to prostate volume (PSA density) as a parameter to improve the detection of prostate carcinoma in PSA values in the range of < 4 ng/mL. Cancer. 2005; 104:993–1003.

20. Ghafoori M, Varedi P, Hosseini SJ, Asgari M, Shakiba M. Value of prostate-specific antigen and prostate-specific antigen density in detection of prostate cancer in an Iranian population of men. Urol J. 2009; 6:182–188.
21. Roobol MJ, Schröder FH, Hugosson J, Jones JS, Kattan MW, Klein EA, et al. Importance of prostate volume in the European Randomised Study of Screening for Prostate Cancer (ERSPC) risk calculators: results from the prostate biopsy collaborative group. World J Urol. 2012; 30:149–155.

22. Benson MC, Whang IS, Pantuck A, Ring K, Kaplan SA, Olsson CA, et al. Prostate specific antigen density: a means of distinguishing benign prostatic hypertrophy and prostate cancer. J Urol. 1992; 147(3 Pt 2):815–816.

23. Bazinet M, Meshref AW, Trudel C, Aronson S, Péloquin F, Nachabe M, et al. Prospective evaluation of prostate-specific antigen density and systematic biopsies for early detection of prostatic carcinoma. Urology. 1994; 43:44–51.

24. Elliott CS, Shinghal R, Presti JC Jr. The performance of prostate specific antigen, prostate specific antigen density and transition zone density in the era of extended biopsy schemes. J Urol. 2008; 179:1756–1761.

25. Gregorio EP, Grando JP, Saqueti EE, Almeida SH, Moreira HA, Rodrigues MA. Comparison between PSA density, free PSA percentage and PSA density in the transition zone in the detection of prostate cancer in patients with serum PSA between 4 and 10 ng/mL. Int Braz J Urol. 2007; 33:151–160.

26. Park HK, Lee KY, Kim KH, Jung H, Yoon SJ, Kim TB. Intermediate versus low or high prostate-specific antigen density level: comparison of cancer detection rate between 12- and 18-core prostate biopsy. Scand J Urol Nephrol. 2010; 44:391–398.

28. Nunez-Nateras R, Andrews JR, Martin GL, Andrews PE, Humphreys MR, Ferrigni RG, et al. Accuracy of ultrasound in estimation of prostate weight: comparison of urologists and radiologists. Can J Urol. 2010; 17:4985–4988.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download