Abstract
Purpose
To assess the therapeutic value of two different drainage catheters in treating chronic subdural hematoma (CSDH).
Materials and Methods
Two types of drainage catheters can be used to treat CSDH according to the position of holes in the catheter: open-type or closed-type catheter. In this retrospective study, 199 total patients with CSDH were reviewed according to catheter type. Among them, 84 patients were and 113 in the closed-type group (holes positioned within the distal-most 1 cm of the catheter). The surgeon selected the catheter type. Total drainage volume, initial drainage volume within 2 days, percentage of initial drainage volume per total drainage volume, duration of catheter insertion, and reoperation rate were compared.
Results
Total drainage volume was not different between the two groups (p=0.333). The initial drainage volume within 2 days was larger in the open-type group than closed-type group (p=0.024), but the percentage of initial drainage volume per total drainage volume was not different (p=0.354). The duration of catheter insertion was shorter in the open-type group than closed-type group (p=0.015). The reoperation rate of CSDH was also higher in the open-type group than closed-type group (p=0.004).
Chronic subdural hematomas (CSDHs) usually occur in the neurosurgical disease in the elderly, particularly after minor head injury.1,2 In patients older than 50 years, the brain parenchyme is reduced by almost 200 g, which results in an increased subdural space and arachnoid space up to 11%.3 Hematomas can occupy this extra volume without increasing intracranial pressure. Furthermore, a slowly progressing hematoma allows the brain to adjust by compressing the venous channels, thus providing further space for the expanding hematoma.3 In addition, the outer subdural membrane, which functions to absorb the subdural fluid, produces a layer of thin-walled sinusoidal vascular channels that are liable to bleed because of the presence of loose cell junctions. As long as there is a balance between the expanding and absorptive forces, however, the size of the hematoma remains constant and the patient remains asymptomatic.
The pressure gradient between the sinusoidal channels in the capsule and hematoma's cavity was disrupted by multiple head injury or position changes of the head in the vertical. And, disruption of the pressure gradiet induce additional bleeding. After Valsalva maneuver temporarily reduce intracranial pressure. And, that can lead to an expansion of the hematoma.4 In addition, the activation of the kallikrein-kinin cascade increases vascular permeability and may cause blood extravasation and plasma exudation from the capillaries into both the outer membrane and the hematoma cavity, thereby enlarging the hematoma.5,6
It is a clinical entity with a decreasing mortality and morbidity, especially since the advent of computed tomography (CT) and advances in surgical technique. There is still debate, however, on the pathophysiology, methodology of management, and surgical treatment of CSDH.7 Although many surgical techniques have been explored for the treatment of CSDH, most neurosurgeons favor a burr-hole craniostomy and closed-system drainage without irrigation because it has low morbidity and mortality rates and is simple. In neurosurgical field, there are different types of drainage catheter such as open or closed type. These catheters are categorized by the position of holes in the catheter, therefore, the function for drainage could be different by the types of catheters. However, there has been no study comparing the catheter type used in surgery.
In this study, 197 patients with CSDH underwent surgery and were analyzed prospectively for radiological, clinical, and surgical features. Results in the open-type catheter group were compared with those in the closed-type catheter group, and the surgical treatment options are discussed in the context of the current literature.
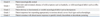
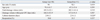
From March 2010 to May 2012, 199 consecutive patients (33 females and 166 males) with CSDH underwent burr-hole craniostomy with closed-system drainage at the Department of Neurosurgery, Inha University School of Medicine. The drainage catheter was categorized as either the open type or closed type according to the hole position on the catheter, with the open type having holes positioned within the distal-most 5 cm of the catheter and a large hole at the end (Fig. 1), and the closed type having holes positioned within the distal-most 1 cm of the catheter (Fig. 2). Total 199 patients with CSDH were retrospectively reviewed according to the catheter type; 84 patients were included in the open-type group (Group A) and 113 in the closed-type group (Group B), while 2 patients with both types of catheters were excluded from this study. CSDH was defined as the presence of a typical neomembrane, liquefied blood within the hematoma cavity, and at least a 3-week interval since the head trauma. Diagnosis was confirmed by CT and/or magnetic resonance imaging in all patients. They were also subdivided according to their CT and clinical findings. We analyzed the type of hematoma in CSDH which is a important factor that affects drainage. Nomura, et al.8 classified the CSDH into two groups: non-mixed density (hematoma observed as purely uniformed density such as low-density, isodensity or high-density) and mixed density. According to Markwalder, et al.,9 clinical condition was classified as followed (Table 1). As a result, the neurological deficit or any absence of symptom was graded "0"; minimal deficit accompanied by nausea and headache was graded as "1"; neurological deficit like hemiparesis related to drowsiness or disorientation was graded as 2; further neurological deficit with stupor and hemiplegia was graded as "3"; decerebrate or decorticate posture associated with coma was graded as "4". Additionally, Glasgow Coma Scale (GCS) score was used. Full recovery, minimal neurological deficit, severe neurological deficit, or death.10 That were classified for the postoperative clinical status.
Most operations were performed by either general or local anesthesia. All patients were undergone by surgical procedures of 1 burr hole over the area of maximal hematoma width and closed-system drainage with a commercial silicone catheter and bag. The type of catheter was selected to the attending neurosurgeon. Right after subdural hematoma was spontaneously evacuated after burr-hole trephination, the drainage catheter was inserted. In all cases, warm saline irrigation through the silicone catheter was never applied to the procedure. The drainage bags maintained below the head level were removed in accordance with the change of the drainage volume and radiological findings; however, they were generally removed within 6 days to avoid the complications associated with a drainage catheter. Brain CT for pre-operation and post-operation was performed respectively and even follow-up CT was done for all cases. Clinical and/or radiological criteria were used for evaluation of CSDH recurrence and to determine the necessity for reoperation. The clinical criteria finally included a change in mental status, worsening of preexisting neurological deficit, and new onset or aggravation of headache for recurrence. For radiological criteria for recurrence, there was an increase in subdural collection and/or compressed brain parenchyma. They were all determined by comparing CT findings for the follow-up period with the postoperative CT findings. As defined above, all patients underwent reoperation if there are neurological symptoms recurred or if there are new neurological symptoms developed with the increase in hematoma thickness and volume on follow-up CT. Someone who showed no or minimal neurological deficit postoperatively, or who had a small amount of residual hematoma, were discharged and followed up as outpatients.
Follow-up CT was performed on the 2nd, 5th, and 30th postoperative days. The differently treated groups were compared with each other in total drainage volume, initial drainage volume within 2 days, percentage of initial drainage volume per total drainage volume, duration of catheter insertion, and reoperation rate. For statistical analysis, we used the chi-square test (Fisher's extract test) to determine significant differences between the groups. Differences were considered statistically significant at p<0.05.
In this study, the selection of the catheter was made, based only on personal preference without considering age, gender, type of hematoma, and consciousness of patients.
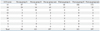
The series consists of 165 men and 32 women with a mean age of 70.9 years (range, 2 months to 98 years). In Group A, mean age was 72.5±10.2 years and 69.6±13.9 years in Group B. Group A (84 patients) was made up of 74 men and 10 women (88.1% men), whereas Group B (113 patients) was made up of 91 men and 22 women (80.5% men). There was no statistically significant difference in age between the 2 groups (age, p=0.111; sex, p=0.156) (Table 2).
The total drainage volumes were 192.1±140.6 mL for open-type and 173.2±131.5 mL for closed-type catheters (p=0.333). The catheters were maintained for 2.75±1.40 days with open-type and 3.35±1.90 days with closed-type catheters, which was statistically significant (p=0.015).
For the first 2 days, the drainage volumes were 163.8±101.6 mL for open-type and 133.1±87.4 mL for closed-type catheters, and the drainage volume was larger in open-type catheters (p=0.020). The recurrence rate was 22.35%±37.49 for open-type and 8.06%±17.45 for closed-type catheters, and this difference was especially statistically significant (p=0.24).
According to the clinical Markwalder grading scale, 22 patients were in grade 0, 98 patients in grade 1, 65 patients in grade 2, 10 patients in grade 3, and 2 patients in grade 4 (Table 3). The preoperative GCS grade for each catheter group is shown in Table 4, but it did not reach statistical significance (p=0.521). The change of postoperative grade was relatively milder on the Markwalder scale compared to the GCS scale; however, it was not statistically significant (p=0.373).
Hematoma progress was tracked through follow-up brain CT in order to assess when patients could be discharged (hematoma fully resolved) and whether reoperation would be necessary (postoperative hematoma recurrence). The reoperation was performed during the hospitalization if the hematoma was not resolving. About 20.9% of patients in Group A required reoperation (n=84), but only 14.2% of patients in Group B (n=113) underwent reoperation; this difference was statistically significant (p=0.034).
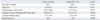
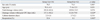
The type of hematoma was classified into mixed- and non-mixed type. The total drainage volumes were 201.79 (±165.5) mL for open-type and 149.0 (±118.47) mL for closed-type catheters. The catheters were maintained for 3.29 (±1.60) days with open-type, and 3.74 (±2.29) days with closed-type catheters, which was not statistically significant.
For the first 2 days, the drainage volumes were 157.06 (±102.24) mL for open-type and 112.80 (±78.98) mL for closed-type catheters, and the drainage volume was larger in open-type catheters (p=0.020). The recurrence rate was 22.35% (±37.49) for open-type and 8.06% (±17.45) for closed-type catheters, and this difference, was statistically significant (p=0.012) (Table 5).
For the non-mixed type of hematomas (n=101), the total drainage volume was 185.52 (±122.12) for open-type and 202.55 (±141.44) for closed-type catheters. In the first 2 days, the drainage volume for each catheter type was not different; 168.32 (±101.93) mL for open-type and 157.82 (±91.39) mL for closed-type catheters. The recurrence rates were 30.00% (±36.29) for open-type and 21.57% (±31.54) for closed-type catheters, which was also not significant; however, the maintenance of catheter was 2.38 (±1.12) days for open-type and 2.88 (±1.11) days for closed-type catheters, which was statistically significant (p=0.026) (Table 6).
Treatment of CSDH has improved dramatically in recent years because of advances in diagnostic tools and surgical techniques. However, there is still some debate regarding the best strategy for treatment. Use of a burr-hole craniostomy and closed-system drainage without irrigation to manage symptomatic CSDH is the initial treatment because it is associated with lower recurrence rates than other treatment methods.11,12 After performing a burr-hole drainage, the rate of reoperation varies between 2.7% and 30%.5,9,13-16 In this study, reoperation rate was 17.3% (Group A=20.9%; Group B=14.2%), which is in keeping with that reported in many other studies. Debate has ensued over the mechanisms underlying the recurrence of CSDH. Many postulate that poor brain re-expansion and recurrent bleeding from the outer membrane are the major causes.6,17,18 Intracapsular air intrusion after surgery has also been suggested to contribute to the recurrence of CSDH.11,19 Interestingly, the literature indicates that the rate of recurrence is not significantly different for different surgical methods. It has been observed, however, that a prolonged period of maintenance in drainage reduces the recurrence of CSDH, but no study has investigated the drainage method in recovery from surgery.
After the burr-hole drainage, there are adverse effects on the cerebral swelling that include the thick and fibrous membrane of the hematoma, a decline of cerebral blood flow due to functional abnormality, degenerative cerebral shrinking, and lowered intracranial pressure due to the flowing out of cerebrospinal fluid.10,20,21 The faster drainage enables the intracranial pressure to lower before cerebral swelling fully recovers, and this has detrimental effects on cerebral swelling in the subdural space.
The drainage theory of CSDH was not confirmed, nevertheless, the expansion of CSDH due to the oncotic pressure leads to an increase in cranial pressure and results in neurological symptoms.22 Moreover, the drainage occurs via potential energy after drainage catheter insertion and the difference in drainage can be explained by fluid mechanics. The diameter of the catheter and the size of catheter entrance can affect the result of this study; however, the volume of drainage was controlled in this study by using catheters of the same diameter. Furthermore, the size of catheter entrance, depth of the same catheter, and the number of catheters could all influence CSDH drainage.23
The major difference between the 2 drainage methods used in the present study is the position and size of the catheter holes. Specifically, the open-type catheter has a large hole located in the end portion. The open-type catheter is expected to drain much faster initially than the closed-type catheter, because it has more theoretical advantage to drain. As expected, the observed drainage for the first 2 days in this study was much faster for the open-type catheter.
This study was designed to classify hematoma into mixed type and non-mixed type. According to previous study, hematoma of non-mixed type is relatively larger,8 and hematoma of mixed type showed higher recurrent rate.24 In this study, the difference of drainage is relevant to the result which was not classified hematoma with mixed and non-mixed type. In mixed type, there was significantly higher drainage and re-op rate for the first two days when the open catheter was used. On the other hand, closed type of catheter showed relatively long maintenance period which was statistically significant, indicating that the difference of catheter can affect the drainage of hematoma as well as the type of hematoma.
This faster drainage is related to the observed higher incidence of reoperation due to hematoma recurrence after CSDH in Group A and to the shorter maintenance period of the open-type catheter, which was 2.75 (±1.40) days for Group A and 3.35 (±1.90) days for Group B.
There have been several studies investigating the effect of anticoagulant therapies on the recurrence and treatment of CSDH. However, there was no study assessing the impact of drainage according to the type of catheter and the result of treatment for CSDH. The present study strongly indicates that the prognosis depends on the type of catheter. The use of the open-type catheter allowed for faster drainage of hematoma following surgery; however, the use of the closed-type catheter resulted in a lower rate of reoperation.
In conclusion, the use of open-type catheter allowed for faster drainage of hematoma following surgery; however, the use of closed-type catheter resulted in a lower rate of reoperation. When using closed-system drainage to treat CSDH, careful catheter selection is imperative. These data show that closed-type catheter is as reliable and effective as open-type catheter, and offers the advantage of a lower reoperation rate.
Figures and Tables
Fig. 1
The open-type catheter has 5 holes within the distal-most 5 cm, with a large hole at the end position of the catheter.
Table 3
The Preoperative and Postoperative Markwalder Chronic Subdural Hematoma Scale in Catheter Groups
References
1. Chen JC, Levy ML. Causes, epidemiology, and risk factors of chronic subdural hematoma. Neurosurg Clin N Am. 2000; 11:399–406.

2. Hamilton MG, Frizzell JB, Tranmer BI. Chronic subdural hematoma: the role for craniotomy reevaluated. Neurosurgery. 1993; 33:67–72.
3. Tabaddor K, Shulmon K. Definitive treatment of chronic subdural hematoma by twist-drill craniostomy and closed-system drainage. J Neurosurg. 1977; 46:220–226.

4. Markwalder TM, Reulen HJ. Influence of neomembranous organisation, cortical expansion and subdural pressure on the post-operative course of chronic subdural haematoma--an analysis of 201 cases. Acta Neurochir (Wien). 1986; 79:100–106.

5. Fujisawa H, Ito H, Kashiwagi S, Nomura S, Toyosawa M. Kallikrein-kinin system in chronic subdural haematomas: its roles in vascular permeability and regulation of fibrinolysis and coagulation. J Neurol Neurosurg Psychiatry. 1995; 59:388–394.

6. Aung TH, Wong WK, Mo HP, Tsang CS. Management of chronic subdural haematoma: burr hole drainage, replacement with Hartmann's solution, and closed-system drainage. Hong Kong Med J. 1999; 5:383–386.
7. Kwon TH, Park YK, Lim DJ, Cho TH, Chung YG, Chung HS, et al. Chronic subdural hematoma: evaluation of the clinical significance of postoperative drainage volume. J Neurosurg. 2000; 93:796–799.

8. Nomura S, Kashiwagi S, Fujisawa H, Ito H, Nakamura K. Characterization of local hyperfibrinolysis in chronic subdural hematomas by SDS-PAGE and immunoblot. J Neurosurg. 1994; 81:910–913.

9. Markwalder TM, Steinsiepe KF, Rohner M, Reichenbach W, Markwalder H. The course of chronic subdural hematomas after burr-hole craniostomy and closed-system drainage. J Neurosurg. 1981; 55:390–396.

10. Benzel EC, Bridges RM Jr, Hadden TA, Orrison WW. The single burr hole technique for the evacuation of non-acute subdural hematomas. J Trauma. 1994; 36:190–194.

11. Oku Y, Takimoto N, Yamamoto K, Onishi T. Trial of a new operative method for recurrent chronic subdural hematoma. J Neurosurg. 1984; 61:269–272.

12. Kuroki T, Katsume M, Harada N, Yamazaki T, Aoki K, Takasu N. Strict closed-system drainage for treating chronic subdural haematoma. Acta Neurochir (Wien). 2001; 143:1041–1044.

13. Okada Y, Akai T, Okamoto K, Iida T, Takata H, Iizuka H. A comparative study of the treatment of chronic subdural hematoma--burr hole drainage versus burr hole irrigation. Surg Neurol. 2002; 57:405–409.

14. Cameron MM. Chronic subdural haematoma: a review of 114 cases. J Neurol Neurosurg Psychiatry. 1978; 41:834–839.

15. Eggert HR, Harders A, Weigel K, Gilsbach J. [Recurrence following burr hole trephination of chronic subdural hematomas]. Neurochirurgia (Stuttg). 1984; 27:141–143.
16. Robinson RG. Chronic subdural hematoma: surgical management in 133 patients. J Neurosurg. 1984; 61:263–268.

17. Camel M, Grubb RL Jr. Treatment of chronic subdural hematoma by twist-drill craniotomy with continuous catheter drainage. J Neurosurg. 1986; 65:183–187.

18. Rosenørn J, Gjerris F. Long-term follow-up review of patients with acute and subacute subdural hematomas. J Neurosurg. 1978; 48:345–349.

19. Nakaguchi H, Tanishima T, Yoshimasu N. Relationship between drainage catheter location and postoperative recurrence of chronic subdural hematoma after burr-hole irrigation and closed-system drainage. J Neurosurg. 2000; 93:791–795.

20. Arbit E, Patterson RH Jr, Fraser RA. An implantable subdural drain for treatment of chronic subdural hematoma. Surg Neurol. 1981; 15:175–177.

21. Obana WG, Pitts LH. Management of head injury. Extracerebral lesions. Neurosurg Clin N Am. 1991; 2:351–372.
23. Fox RW, Pritchard PJ, McDonald AT. Introduction to Fluid Mechanics. 7th ed. New York: John Wiley & Sons Inc;2009.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download