Abstract
Optical coherence tomography (OCT) has been recently applied to investigate coronary artery disease in interventional cardiology. Compared to intravascular ultrasound, OCT is able to visualize various vascular structures more clearly with higher resolution. Several validation studies have shown that OCT is more accurate in evaluating neointimal tissue after coronary stent implantation than intravascular ultrasound. Novel findings on OCT evaluation include the detection of strut coverage and the characterization of neointimal tissue in an in-vivo setting. In a previous study, neointimal healing of stent strut was pathologically the most important factor associated with stent thrombosis, a fatal complication, in patients treated with drug-eluting stent (DES). Recently, OCT-defined coverage of a stent strut was proposed to be related with clinical safety in DES-treated patients. Neoatherosclerosis is an atheromatous change of neointimal tissue within the stented segment. Clinical studies using OCT revealed neoatherosclerosis contributed to late-phase luminal narrowing after stent implantation. Like de novo native coronary lesions, the clinical presentation of OCT-derived neoatherosclerosis varied from stable angina to acute coronary syndrome including late stent thrombosis. Thus, early identification of neoatherosclerosis with OCT may predict clinical deterioration in patients treated with coronary stent. Additionally, intravascular OCT evaluation provides additive information about the performance of coronary stent. In the near future, new advances in OCT technology will help reduce complications with stent therapy and accelerating in the study of interventional cardiology.
Although bare-metal stents (BMS) show better outcomes than balloon angioplasty in reducing acute vessel closure,1,2 in-stent restenosis (ISR) of treated coronary arteries still remains a challenge. Pathologic studies have revealed that neointimal tissue within stented segments mainly consist of smooth muscle cells and extracellular matrix.3,4 Thus, the inhibition of smooth muscle cell has been a therapeutic target of percutaneous coronary intervention for reducing overwhelming growth of neointimal tissue. Compared to BMS, drug-eluting stents (DES) show remarkably reduced rates of angiographic restenosis and improved clinical outcomes.5,6 Therefore, DES, which comprises a metallic stent frame, anti-proliferative drugs and polymer, has been the main agent for treating coronary artery disease until now. While DES is considered an ideal treatment modality for coronary artery disease, this benefit has been challenged with the emergence of stent thrombosis, a serious complication. According to recent registries, the rate of late stent thrombosis was 0.53% per year and steadily increased to 3% over 4 years in first-generation DES-treated patients.7,8 Accordingly, balance between the efficacy and safety of DES should be considered in DES implantation in patients with coronary artery disease. As optical coherence tomography (OCT) has enabled the observation of delicate coronary vessels and stents with superior resolution, a number of OCT studies have investigated DES-treated lesions in various clinical situations. Therefore, we sought to review recent advances in OCT focusing on DES-treated lesions.
Intravascular ultrasound (IVUS) has been the standard imaging modality for evaluating the status of a coronary stent. However, it is limited in evaluating neointimal tissue within the stented segment due to its low resolution. Contrary to IVUS, OCT has a resolution of 10-20 µm, which is about 10 times higher than that of IVUS (80-120 µm). Previous studies have shown the superiority of OCT over IVUS in relation to resolution capacity. Compared to IVUS, OCT showed better diagnostic accuracy for detecting a small degree of in-stent neointima, which was defined as occupying <30% of the stent area measured with histology.9 The optical cutoff value of percent neointimal hyperplasia (NIH) cross-sectional area (CSA) for detecting NIH by IVUS was 14.7%; OCT-measured neointimal tissue of percent NIH CSA <14.7% cannot be detected with IVUS.10
Recently, time-domain OCT systems have evolved to next-generation frequency-domain OCT systems. In the former system, an occlusion balloon was inflated and lactated Ringer's solution was infused through a catheter for acquiring OCT images. However, the frequency-domain OCT system is able to generate frames at much higher rates and allows for faster pullback speeds. Instead of the occlusion balloon, contrast medium is continuously flushed at a rate of 4 to 5 mL/s for 3 to 4 seconds. In an OCT study to evaluate the feasibility of frequency-domain OCT, frequency-domain OCT showed shorter procedural time (3.2±0.8 min vs. 11.2±2.5 min, p<0.01) and a higher acquisition rate of clear images (99.4% vs. 80.8%, p<0.01) than time-domain OCT.11 Additionally, frequency-domain OCT was not related to any adverse cardiac events.11 Frequency-domain OCT showed better detection of incomplete stent apposition (malapposition) or uncovered strut, compared with IVUS.12,13
In IVUS study, incomplete stent apposition is defined as a separation of at least one stent strut from the intimal surface of the arterial wall that is not overlapping a side branch and has evidence of blood flow behind the strut.14 OCT enables one to observe apposition of a stent strut more accurately compared to IVUS; malapposed stent struts on OCT are defined as a distance between the strut marker and lumen contour greater than the strut thickness plus the axial resolution of OCT.15 Accordingly, definitions of malapposed struts differ according to type of coronary stent because the thickness of struts and applied polymer vary. Fig. 1 shows typical examples of well-apposed and malapposed struts. The following are thresholds of malapposed struts for several DESs; ≥160 µm for sirolimus-eluting stent (Cypher Select™, Cordis, Miami Lake, FL, USA), ≥130 µm for paclitaxel-eluting stent (Taxus Liberte™, Boston Scientific, Natick, MA, USA), ≥110 µm for zotarolimus-eluting stent (Endeavor™ and Resolute™, Medtronic, Santa Rosa, CA, USA), ≥100 µm for everolimus-eluting stents (Xience™, Abbott Vascular, Santa Clara, CA, USA) and ≥130 µm for biolimus-eluting stent (Nobori™, Terumo Corporation, Tokyo, Japan or BioMatrix™, Biosensors Interventional, Singapore).16-19
As neointimal tissue proliferates after stent implantation, malapposed struts usually disappear when the distance between the stent strut and vessel wall is short.16,20-22 Previous OCT study showed that the percentage of malapposed struts with minimal malapposition decreased from 12.2±11.0% post-intervention to 1.0±2.2% after about 6 months of follow-up.16 However, some struts are persistently malapposed after an index procedure (persistent malapposition) and some are newly detected at follow-up (late-acquired malapposition). Although the healing process of malapposed struts has not yet been clearly addressed, recent OCT studies showed incomplete stent apposition was more likely to be sustained as its distance (or area) was far from the vessel wall;21,22 a strut-to-vessel distance of ≤260 µm on post-stenting OCT images was suggested as a cut-off value for resolved malapposition of first-generation DES.22 Additionally, in other study, coverage of malapposed struts was delayed with respect to well-apposed strut at 9 to 13 months of follow-up after DES implantation.23 Although overall malapposed struts were positively correlated with uncovered struts, a subgroup of lesions with minimal stent malapposition showed similar rates of uncovered struts to those without malapposition.24 The coverage of malapposed struts was also affected by DES type, first- vs. new-generation DESs.25
A number of OCT studies have evaluated the in-vivo status of DES at various time points after stent implantation. According to these reports, the healing of DES was quite slow and heterogeneous even several years after stent implantation.20,26,27 Neointimal growth after stent implantation is considered part of the wound healing process that generally occurs after injury.3 This process generally consists of three phases: 1) an inflammatory phase (platelet aggregation and inflammatory cell infiltration), 2) a granulation phase (migration and proliferation of endothelial cells, fibroblasts or smooth muscle cells from adjacent tissue) and 3) a matrix remodeling phase (production of proteoglycan from fibroblasts and smooth muscle cells).3 By these steps, BMSs are fully covered with neointima about 1 month after stent implantation.3 Because anti-proliferative drugs with DES inhibits the migration and proliferation of smooth muscle cells, delayed neointimal coverage of a DES is somewhat to be expected. However, even after the anti-proliferative drug is completely eluted into the adjacent wall, DES struts frequently remain uncovered upon ex- and in-vivo examination of implanted stents.28-30 Few sirolimus-eluting stents show complete coverage at 6 months post-intervention.29 For paclitaxel-eluting stents, another first-generation DES, one study also showed that the incidence of completely covered stents was 29.6% at 9 months post-intervention.30 Consequently, patients treated with first-generation DES should receive dual anti-platelet therapy (aspirin and clopidogrel) for a longer time than those that received a BMS. To overcome the above limitation with first-generation DES, new-generation DESs have been developed with an advanced strut platform, polymer and new anti-proliferative drugs.
Table 1 summarizes the strut apposition and coverage of various DESs. Compared to sirolimus-eluting stent, the coverage of Endeavor zotarolimus-eluting stent was almost complete at 3 months.31 The rate of stent thrombosis was 0.2% during 1-year follow-up in patients that received only 3-month dual anti-platelet therapy following Endeavor zotarolimus-eluting stent implantation in the REal Safety and Efficacy of 3-month dual antiplatelet Therapy (RESET) trial to evaluate the safety and efficacy thereof.32 Resolute zotarolimus-eluting stent also showed higher rates of strut coverage than sirolimus-eluting stent at 9 months,17 as did everolimus-eluting stent.18 The Swedish Coronary Angiography and Angioplasty Registry (SCAAR) data revealed that the rates of restenosis and definite stent thrombosis in these new-generation DESs were lower than that of first-generation DESs.33 Biolimus-eluting stent has the unique property of a biodegradable polymer with abluminal coating. In a sub-study of the Limus Eluted from A Durable vs. ERodable Stent coating (LEADERS) trial, OCT-defined coverage of biolimus-eluting stent was greater than that of sirolimus-eluting stent at 9 months.34 The superiority of biolimus-eluting stent translated into greater clinical safety during 4-year follow-up; late definite stent thrombosis occurred less frequently in patients treated with biolimus-eluting stent.35 Fig. 2 depicts various rates of DES coverage over time.
A recent autopsy study revealed delayed neointimal healing of implanted stent was associated with occurrence of late stent thrombosis; the odds ratio of a stent with a ratio of uncovered to total stent struts per section >30% was 9.0 (95% confidence interval, 3.5 to 22) for stent thrombosis.28 In a case-control study in which OCT was performed at onset of stent thrombosis, the length of an uncovered stent strut segment was significantly associated with stent thrombosis.36 Strut coverage assessed by OCT may be a surrogate marker for predicting catastrophic cardiovascular events in daily clinical practice. One OCT study suggested that a greater percentage of uncovered struts (a cut-off value of ≥5.9% uncovered struts), as assessed by OCT at 6-18 months follow-up, in asymptomatic DES-treated patients might predict increases in major adverse cardiac events related with stent safety in the future.37
In quantitative OCT analysis, stent and luminal CSA are measured, and NIH CSA is then calculated as the stent CSA minus the luminal CSA. Percentage of NIH CSA is calculated as NIH CSA×100/stent CSA. NIH thickness, the distance between the endoluminal surface of neointima and the strut, can be measured inside all struts as a line perpendicular to the neointima and strut.38 An uncovered strut is defined as having a NIH thickness of 0 µm.38 The percentage of malapposed or uncovered struts in each stented lesion can be calculated as the (number of malapposed or uncovered struts/total number of struts in all cross-sections of the lesion)×100, respectively.
Because the NIH within stent segments mainly consists of smooth muscle cells and extra-cellular matrix, the predominant pattern of NIH by IVUS evaluation has been presented as a homogenous appearance.10 However, one OCT study reported that various patterns of neointimal tissue develop in ISR lesions, suggesting that the mechanism for ISR might be complicated.39 Fig. 3 shows homogeneous, heterogeneous and layered patterns of neointimal tissue. Differences in optical property and backscattering pattern arise from the heterogeneity of neointimal tissue, which contains various components such as fibrin accumulation, excessive inflammation (hypersensitivity reaction), extra-cellular matrix or in-stent neoatherosclerosis, as well as smooth muscle cells.13 Therefore, it is difficult to conclude that specific types of neointimal tissue seen by OCT imply consistent histopathologic findings. Instead, observation of diverse neointima indicates that the healing process after stent deployment is not stable and may be associated with clinical events. An OCT study showed that heterogeneous or layered patterns of neointima were more frequently observed in ISR lesions than in non-ISR lesions.40 However, to clarify the clinical implications of different neointimal features, further investigations are needed.
Neoatherosclerosis refers to an atherosclerotic change in neointimal tissue, which is histologically defined as clusters of lipid-laden foamy macrophages within the neointima with or without necrotic core formation.41 On OCT images, lipidic neointima is shown as diffusely bordered, signal-poor regions with overlying signal-rich bands; calcific neointima shows well-delineated, signal-poor regions with sharp borders.15,42 OCT-defined neoatherosclerosis is mainly confined to lipidic or calcific neointima.43,44 Representative images of neoatherosclerosis are shown in Fig. 3. Neoatherosclerotic change in neointima occurs in both BMS and DES.41,43 Previous histologic study found that neoatherosclerosis was observed more frequently and earlier in DES compared to BMS.41 This finding was also shown in an OCT study,43 suggesting incomplete endothelization might be involved in acceleration of atherogenesis inside neointima. Neoatherosclerosis contributes to late-phase luminal narrowing after stent implantation.45,46 Previous angiographic study revealed that the luminal diameter of BMS followed a biphasic pattern of early narrowing and late improvement between 6 months and 3 years.47 On the other hand, the neointima of DES continuously progressed up to 5 years.48 An OCT study showed thin-cap fibroatheroma-like neointima was more commonly detected in very late ISR lesions (>3 years) than in early ISR lesions (<1 year).46 Another serial OCT study also demonstrated that the frequency of neoatherosclerosis in DES-treated lesions increased between 9 months and 2 years.26 Clinical presentation of neoatherosclerosis varies from stable angina to stent thrombosis. Compared to patients with stable angina, patients with unstable angina show higher incidences of OCT-defined thin-cap fibroatheroma, intimal rupture and thrombi.49 In addition, OCT-defined rupture of lipidic neointima was observed in patients with very late stent thrombosis.50 Although one OCT study suggested that risk factors of neoatherosclerosis were similar to those of native coronary artery disease,44 the mechanism of neoatherosclerotic change remains unknown and needs to be investigated in the future.
Although OCT is a recent advancement in intravascular imaging, a number of limitations remain. OCT has a shallow penetration depth of about 2 mm and is not able to visualize structures behind severely attenuated components such as lipid-laden neointima or thrombus. In contrary to IVUS, blood in coronary arteries should be eliminated to acquire adequate OCT images because blood scatters light. For this purpose, continuous flush of saline or contrast media has been applied. Since frequency-domain OCT utilizes a faster authorized pullback system than time-domain OCT, it takes less time to inject contrast media. Nevertheless, it is inevitably necessary to create a blood-free field due to the natural limitation of optics. The current OCT system is not able to discriminate fibrin accumulation, excessive inflammation, abundant extracellular matrix, or neoatherosclerosis, because these are similarly shown as a dark appearance on OCT.13,51
Three-dimensional OCT technology is now under investigation for evaluating coronary artery disease. Three-dimensional OCT reconstruction allows researchers to analyze planes which are not visible on two-dimensional images.52 Although three-dimensional OCT technology is still time-consuming, this application has been applied to the assessment of bifurcated lesion and coronary stent.52,53 An OCT study showed that three-dimensional OCT reconstruction was feasible for evaluating the orifices of side-branch vessels after stent implantation.52 Fig. 4 represents a contour map analysis for evaluating the status of a coronary stent strut.53 By this approach, the performance of a coronary stent could be easily visualized at a glance. Tissue characterization with OCT remains a challenge because tissue components vary and some appear similarly on OCT. Several OCT techniques are being developed to enhance the differentiation of tissue components. Polarization-sensitive OCT is a novel technique that can be used to measure the polarization properties of backscattered light.54 Cellular targeting agents such as fluorophores may be useful to characterize neointimal tissues, combined with hybrid OCT systems.55
Utilizing the high resolution of OCT, several OCT studies have evaluated the in-vivo status of DES. The OCT-derived detection of an uncovered strut or neoatherosclerosis may be of use in preventing and predicting adverse cardiac events such as the stent thrombosis. Moreover, advances in OCT technology are expected to reveal detailed changes in coronary stents and to widen the practical usefulness thereof.
Figures and Tables
Fig. 1
Representative images of well-apposed vs. malapposed struts. Optical coherence tomography shows well-apposed struts with complete coverage 9 months after drug-eluting stent implantation (A), whereas some struts (arrowheads) show incomplete stent apposition and uncovered portions to the lumen (B).
Fig. 2
Strut coverage of drug-eluting stent (DES) over time. A dot represents each of the studies in Table 1, except for Bayesian hierarchical models. A curved line represents estimated change of uncovered strut after DES implantation. Usage of sirolimus-eluting stent and incomplete stent apposition increases the risk of delayed coverage after DES implantation.
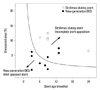
Fig. 3
Various patterns of neointimal tissue. (A) Homogeneous pattern, (B) heterogeneous pattern, (C) layered pattern, (D) lipid-laden neointima, (E) neointima with calcification.

Fig. 4
Contour plot of strut coverage after drug-eluting stent implantation, using optical coherence tomography. The contour plot shows detailed information about the position and coverage of stent strut, in which the circumferential arc is plotted along the X axis and the stent length is plotted along the Y axis. Blue circles represent uncovered struts, red circles represent malapposed struts, and orange circles represent struts crossing over a side-branch vessel.53

Table 1
Strut Apposition and Coverage of Drug-Eluting Stent Assessed by Optical Coherence Tomography

*Values were presented as the percentage of strut which was divided by total number of analyzable struts.15
†Values were derived from Bayesian hierarchical models.
References
1. Serruys PW, de Jaegere P, Kiemeneij F, Macaya C, Rutsch W, Heyndrickx G, et al. Benestent Study Group. A comparison of balloon-expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. N Engl J Med. 1994; 331:489–495.

2. Fischman DL, Leon MB, Baim DS, Schatz RA, Savage MP, Penn I, et al. Stent Restenosis Study Investigators. A randomized comparison of coronary-stent placement and balloon angioplasty in the treatment of coronary artery disease. N Engl J Med. 1994; 331:496–501.

3. Forrester JS, Fishbein M, Helfant R, Fagin J. A paradigm for restenosis based on cell biology: clues for the development of new preventive therapies. J Am Coll Cardiol. 1991; 17:758–769.

5. Moses JW, Leon MB, Popma JJ, Fitzgerald PJ, Holmes DR, O'Shaughnessy C, et al. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med. 2003; 349:1315–1323.

6. Stone GW, Ellis SG, Cox DA, Hermiller J, O'Shaughnessy C, Mann JT, et al. A polymer-based, paclitaxel-eluting stent in patients with coronary artery disease. N Engl J Med. 2004; 350:221–231.

7. Daemen J, Wenaweser P, Tsuchida K, Abrecht L, Vaina S, Morger C, et al. Early and late coronary stent thrombosis of sirolimus-eluting and paclitaxel-eluting stents in routine clinical practice: data from a large two-institutional cohort study. Lancet. 2007; 369:667–678.

8. Wenaweser P, Daemen J, Zwahlen M, van Domburg R, Jüni P, Vaina S, et al. Incidence and correlates of drug-eluting stent thrombosis in routine clinical practice. 4-year results from a large 2-institutional cohort study. J Am Coll Cardiol. 2008; 52:1134–1140.

9. Suzuki Y, Ikeno F, Koizumi T, Tio F, Yeung AC, Yock PG, et al. In vivo comparison between optical coherence tomography and intravascular ultrasound for detecting small degrees of in-stent neointima after stent implantation. JACC Cardiovasc Interv. 2008; 1:168–173.

10. Kwon SW, Kim BK, Kim TH, Kim JS, Ko YG, Choi D, et al. Qualitative assessment of neointimal tissue after drug-eluting stent implantation: comparison between follow-up optical coherence tomography and intravascular ultrasound. Am Heart J. 2011; 161:367–372.

11. Takarada S, Imanishi T, Liu Y, Ikejima H, Tsujioka H, Kuroi A, et al. Advantage of next-generation frequency-domain optical coherence tomography compared with conventional time-domain system in the assessment of coronary lesion. Catheter Cardiovasc Interv. 2010; 75:202–206.

12. Bezerra HG, Attizzani GF, Sirbu V, Musumeci G, Lortkipanidze N, Fujino Y, et al. Optical coherence tomography versus intravascular ultrasound to evaluate coronary artery disease and percutaneous coronary intervention. JACC Cardiovasc Interv. 2013; 6:228–236.

13. Nakano M, Vorpahl M, Otsuka F, Taniwaki M, Yazdani SK, Finn AV, et al. Ex vivo assessment of vascular response to coronary stents by optical frequency domain imaging. JACC Cardiovasc Imaging. 2012; 5:71–82.

14. Hong MK, Mintz GS, Lee CW, Park DW, Park KM, Lee BK, et al. Late stent malapposition after drug-eluting stent implantation: an intravascular ultrasound analysis with long-term follow-up. Circulation. 2006; 113:414–419.

15. Tearney GJ, Regar E, Akasaka T, Adriaenssens T, Barlis P, Bezerra HG, et al. Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies: a report from the International Working Group for Intravascular Optical Coherence Tomography Standardization and Validation. J Am Coll Cardiol. 2012; 59:1058–1072.
16. Kim WH, Lee BK, Lee S, Shim JM, Kim JS, Kim BK, et al. Serial changes of minimal stent malapposition not detected by intravascular ultrasound: follow-up optical coherence tomography study. Clin Res Cardiol. 2010; 99:639–644.

17. Kim JS, Kim JS, Shin DH, Kim BK, Ko YG, Choi D, et al. Optical coherence tomographic comparison of neointimal coverage between sirolimus- and resolute zotarolimus-eluting stents at 9 months after stent implantation. Int J Cardiovasc Imaging. 2012; 28:1281–1287.

18. Choi HH, Kim JS, Yoon DH, Hong KS, Kim TH, Kim BK, et al. Favorable neointimal coverage in everolimus-eluting stent at 9 months after stent implantation: comparison with sirolimus-eluting stent using optical coherence tomography. Int J Cardiovasc Imaging. 2012; 28:491–497.

19. Gutiérrez-Chico JL, Jüni P, García-García HM, Regar E, Nüesch E, Borgia F, et al. Long-term tissue coverage of a biodegradable polylactide polymer-coated biolimus-eluting stent: comparative sequential assessment with optical coherence tomography until complete resorption of the polymer. Am Heart J. 2011; 162:922–931.

20. Katoh H, Shite J, Shinke T, Matsumoto D, Tanino Y, Ogasawara D, et al. Delayed neointimalization on sirolimus-eluting stents: 6-month and 12-month follow up by optical coherence tomography. Circ J. 2009; 73:1033–1037.

21. Gutiérrez-Chico JL, Wykrzykowska J, Nüesch E, van Geuns RJ, Koch KT, Koolen JJ, et al. Vascular tissue reaction to acute malapposition in human coronary arteries: sequential assessment with optical coherence tomography. Circ Cardiovasc Interv. 2012; 5:20–29. S1–S8.

22. Kawamori H, Shite J, Shinke T, Otake H, Matsumoto D, Nakagawa M, et al. Natural consequence of post-intervention stent malapposition, thrombus, tissue prolapse, and dissection assessed by optical coherence tomography at mid-term follow-up. Eur Heart J Cardiovasc Imaging. 2013; [Epub ahead of print].

23. Gutiérrez-Chico JL, Regar E, Nüesch E, Okamura T, Wykrzykowska J, di Mario C, et al. Delayed coverage in malapposed and side-branch struts with respect to well-apposed struts in drug-eluting stents: in vivo assessment with optical coherence tomography. Circulation. 2011; 124:612–623.

24. Kim BK, Hong MK, Shin DH, Kim JS, Ko YG, Choi D, et al. Relationship between stent malapposition and incomplete neointimal coverage after drug-eluting stent implantation. J Interv Cardiol. 2012; 25:270–277.

25. Kim BK, Shin DH, Kim JS, Ko YG, Choi D, Jang Y, et al. Optical coherence tomography-based evaluation of malapposed strut coverage after drug-eluting stent implantation. Int J Cardiovasc Imaging. 2012; 28:1887–1894.

26. Kim JS, Hong MK, Shin DH, Kim BK, Ko YG, Choi D, et al. Quantitative and qualitative changes in DES-related neointimal tissue based on serial OCT. JACC Cardiovasc Imaging. 2012; 5:1147–1155.

27. Takano M, Yamamoto M, Mizuno M, Murakami D, Inami T, Kimata N, et al. Late vascular responses from 2 to 4 years after implantation of sirolimus-eluting stents: serial observations by intracoronary optical coherence tomography. Circ Cardiovasc Interv. 2010; 3:476–483.

28. Finn AV, Joner M, Nakazawa G, Kolodgie F, Newell J, John MC, et al. Pathological correlates of late drug-eluting stent thrombosis: strut coverage as a marker of endothelialization. Circulation. 2007; 115:2435–2441.

29. Matsumoto D, Shite J, Shinke T, Otake H, Tanino Y, Ogasawara D, et al. Neointimal coverage of sirolimus-eluting stents at 6-month follow-up: evaluated by optical coherence tomography. Eur Heart J. 2007; 28:961–967.

30. Kim JS, Kim JS, Kim TH, Fan C, Lee JM, Kim W, et al. Comparison of neointimal coverage of sirolimus-eluting stents and paclitaxel-eluting stents using optical coherence tomography at 9 months after implantation. Circ J. 2010; 74:320–326.

31. Kim JS, Jang IK, Kim JS, Kim TH, Takano M, Kume T, et al. Optical coherence tomography evaluation of zotarolimus-eluting stents at 9-month follow-up: comparison with sirolimus-eluting stents. Heart. 2009; 95:1907–1912.

32. Kim BK, Hong MK, Shin DH, Nam CM, Kim JS, Ko YG, et al. A new strategy for discontinuation of dual antiplatelet therapy: the RESET Trial (REal Safety and Efficacy of 3-month dual antiplatelet Therapy following Endeavor zotarolimus-eluting stent implantation). J Am Coll Cardiol. 2012; 60:1340–1348.
33. Sarno G, Lagerqvist B, Fröbert O, Nilsson J, Olivecrona G, Omerovic E, et al. Lower risk of stent thrombosis and restenosis with unrestricted use of 'new-generation' drug-eluting stents: a report from the nationwide Swedish Coronary Angiography and Angioplasty Registry (SCAAR). Eur Heart J. 2012; 33:606–613.

34. Barlis P, Regar E, Serruys PW, Dimopoulos K, van der Giessen WJ, van Geuns RJ, et al. An optical coherence tomography study of a biodegradable vs. durable polymer-coated limus-eluting stent: a LEADERS trial sub-study. Eur Heart J. 2010; 31:165–176.

35. Stefanini GG, Kalesan B, Serruys PW, Heg D, Buszman P, Linke A, et al. Long-term clinical outcomes of biodegradable polymer biolimus-eluting stents versus durable polymer sirolimus-eluting stents in patients with coronary artery disease (LEADERS): 4 year follow-up of a randomised non-inferiority trial. Lancet. 2011; 378:1940–1948.

36. Guagliumi G, Sirbu V, Musumeci G, Gerber R, Biondi-Zoccai G, Ikejima H, et al. Examination of the in vivo mechanisms of late drug-eluting stent thrombosis: findings from optical coherence tomography and intravascular ultrasound imaging. JACC Cardiovasc Interv. 2012; 5:12–20.

37. Won H, Shin DH, Kim BK, Mintz GS, Kim JS, Ko YG, et al. Optical coherence tomography derived cut-off value of uncovered stent struts to predict adverse clinical outcomes after drug-eluting stent implantation. Int J Cardiovasc Imaging. 2013; [Epub ahead of print].

38. Kim BK, Kim JS, Park J, Ko YG, Choi D, Jang Y, et al. Comparison of optical coherence tomographic assessment between first- and second-generation drug-eluting stents. Yonsei Med J. 2012; 53:524–529.

39. Gonzalo N, Serruys PW, Okamura T, van Beusekom HM, Garcia-Garcia HM, van Soest G, et al. Optical coherence tomography patterns of stent restenosis. Am Heart J. 2009; 158:284–293.

40. Lee SJ, Kim BK, Kim JS, Ko YG, Choi D, Jang Y, et al. Evaluation of neointimal morphology of lesions with or without in-stent restenosis: an optical coherence tomography study. Clin Cardiol. 2011; 34:633–639.

41. Nakazawa G, Otsuka F, Nakano M, Vorpahl M, Yazdani SK, Ladich E, et al. The pathology of neoatherosclerosis in human coronary implants bare-metal and drug-eluting stents. J Am Coll Cardiol. 2011; 57:1314–1322.
42. Prati F, Regar E, Mintz GS, Arbustini E, Di Mario C, Jang IK, et al. Expert review document on methodology, terminology, and clinical applications of optical coherence tomography: physical principles, methodology of image acquisition, and clinical application for assessment of coronary arteries and atherosclerosis. Eur Heart J. 2010; 31:401–415.

43. Yonetsu T, Kim JS, Kato K, Kim SJ, Xing L, Yeh RW, et al. Comparison of incidence and time course of neoatherosclerosis between bare metal stents and drug-eluting stents using optical coherence tomography. Am J Cardiol. 2012; 110:933–939.

44. Yonetsu T, Kato K, Kim SJ, Xing L, Jia H, McNulty I, et al. Predictors for neoatherosclerosis: a retrospective observational study from the optical coherence tomography registry. Circ Cardiovasc Imaging. 2012; 5:660–666.
45. Habara M, Terashima M, Nasu K, Kaneda H, Inoue K, Ito T, et al. Difference of tissue characteristics between early and very late restenosis lesions after bare-metal stent implantation: an optical coherence tomography study. Circ Cardiovasc Interv. 2011; 4:232–238.

46. Habara M, Terashima M, Nasu K, Kaneda H, Yokota D, Ito T, et al. Morphological differences of tissue characteristics between early, late, and very late restenosis lesions after first generation drug-eluting stent implantation: an optical coherence tomography study. Eur Heart J Cardiovasc Imaging. 2013; 14:276–284.

47. Kimura T, Yokoi H, Nakagawa Y, Tamura T, Kaburagi S, Sawada Y, et al. Three-year follow-up after implantation of metallic coronary-artery stents. N Engl J Med. 1996; 334:561–566.

48. Collet CA, Costa JR, Abizaid A, Chamié D, Staico R, Costa R, et al. Assessing the temporal course of neointimal hyperplasia formation after different generations of drug-eluting stents. JACC Cardiovasc Interv. 2011; 4:1067–1074.

49. Kang SJ, Mintz GS, Akasaka T, Park DW, Lee JY, Kim WJ, et al. Optical coherence tomographic analysis of in-stent neoatherosclerosis after drug-eluting stent implantation. Circulation. 2011; 123:2954–2963.

50. Ko YG, Kim DM, Cho JM, Choi SY, Yoon JH, Kim JS, et al. Optical coherence tomography findings of very late stent thrombosis after drug-eluting stent implantation. Int J Cardiovasc Imaging. 2012; 28:715–723.

51. Nagai H, Ishibashi-Ueda H, Fujii K. Histology of highly echolucent regions in optical coherence tomography images from two patients with sirolimus-eluting stent restenosis. Catheter Cardiovasc Interv. 2010; 75:961–963.

52. Okamura T, Onuma Y, García-García HM, Regar E, Wykrzykowska JJ, Koolen J, et al. 3-Dimensional optical coherence tomography assessment of jailed side branches by bioresorbable vascular scaffolds: a proposal for classification. JACC Cardiovasc Interv. 2010; 3:836–844.

53. Ha J, Kim BK, Kim JS, Shin DH, Ko YG, Choi D, et al. Assessing neointimal coverage after DES implantation by 3D OCT. JACC Cardiovasc Imaging. 2012; 5:852–853.

54. Giattina SD, Courtney BK, Herz PR, Harman M, Shortkroff S, Stamper DL, et al. Assessment of coronary plaque collagen with polarization sensitive optical coherence tomography (PS-OCT). Int J Cardiol. 2006; 107:400–409.

55. Tahara N, Imaizumi T, Virmani R, Narula J. Clinical feasibility of molecular imaging of plaque inflammation in atherosclerosis. J Nucl Med. 2009; 50:331–334.

56. Kim JS, Jang IK, Fan C, Kim TH, Kim JS, Park SM, et al. Evaluation in 3 months duration of neointimal coverage after zotarolimus-eluting stent implantation by optical coherence tomography: the ENDEAVOR OCT trial. JACC Cardiovasc Interv. 2009; 2:1240–1247.

57. Kim S, Kim JS, Shin DH, Kim BK, Ko YG, Choi D, et al. Comparison of early strut coverage between zotarolimus- and everolimus-eluting stents using optical coherence tomography. Am J Cardiol. 2013; 111:1–5.

58. Gutiérrez-Chico JL, van Geuns RJ, Regar E, van der Giessen WJ, Kelbæk H, Saunamäki K, et al. Tissue coverage of a hydrophilic polymer-coated zotarolimus-eluting stent vs. a fluoropolymer-coated everolimus-eluting stent at 13-month follow-up: an optical coherence tomography substudy from the RESOLUTE All Comers trial. Eur Heart J. 2011; 32:2454–2463.

59. Inoue T, Shite J, Yoon J, Shinke T, Otake H, Sawada T, et al. Optical coherence evaluation of everolimus-eluting stents 8 months after implantation. Heart. 2011; 97:1379–1384.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download