Abstract
A 32-year old single man presented with azoospermia and low semen volume which was noted one and half a year ago. Transrectal ultrasonography and seminal vesiculography were performed to evaluate ejaculatory duct obstruction, and transurethral resection of the ejaculatory duct was performed using a hybrid technique of holmium:yttriumaluminium garnet laser with monopolar transurethral resection to overcome the narrow prostatic urethra. To our knowledge, this is the first report on the successful outcome of a hybrid technique applied for transurethral resection of the ejaculatory duct.
Infertility, defined as the inability to conceive after 1 year of unprotected intercourse, affects approximately 10% to 15% of reproductive age couples in the United States.1 Ejaculatory duct obstruction (EDO) is a relatively rare cause of infertility as male factor and is surgically correctable following an appropriate treatment. Complete EDO has been reported in 1% of all infertile men. Patients with complete EDO shows absent or low ejaculate, and azoospermia in the presence of a palpable vas deferens.2 EDO may show various symptoms including dysuria, hematospermia, pain during or after ejaculation, and perineal or testicular pain or discomfort.3 EDO may be congenital or acquired. The causes of EDO include congenital atresia, duct cysts, trauma, infection, inflammation and calculus formation.4 The standard method of establishing the diagnosis of EDO is seminal vesiculography. Dilated seminal vesicles can be fllled with a dye solution under transrectal ultrasonography (TRUS) guidance; if duct obstruction is complete, the efflux of the dye solution cannot be seen during cystoscopy.5 With advances in noninvasive diagnostic methods, such as high-resolution TRUS and magnetic resonance imaging (MRI), the seminal vesicles can be accurately evaluated, thereby facilitating the diagnosis of EDO.
The treatment of choice for distal seminal tract obstruction is transurethral resection of the ejaculatory duct (TUREJD). Approximately half of men undergoing this procedure for EDO show improvement of their semen parameters and half of the men who improve achieve a subsequent pregnancy.6 Here, we report a single case of EDO with a midline prostatic cyst which resulted in a narrow prostatic urethra. Thus, a hybrid technique using the holmium:yttriumaluminium garnet (Ho:YAG) laser and monopolar transurethral resection (TUR) was performed to overcome the narrow prostatic urethra. To our knowledge, our case is the first report of a hydrid technique used to treat TUREJD.
A 32-year old, single man presented with azoospermia and low semen volume which was noted one and half a year ago. He had no other known medical problems. Semen analysis revealed that the total volume was 0.5 mL and had no identifiable spermatozoa. Bilateral vas deferens were palpable on physical examination. TRUS revealed a midline prostatic cyst of approximately 1.5 cm in diameter with dilated seminal vesicles (Fig. 1). Pelvic MRI revealed a 2 cm sized prostatic utricular cyst and mild dilatation of the seminal vesicle (Fig. 2A, B, C and D). Seminal vesiculography was performed to evaluate ejaculatory duct obstruction because of the prostatic ultracular cyst (Fig. 2E). Under seminal vesiculography, the seminal vesicles and midline cyst were found to be filled with contrast media (Fig. 2D). Fluid which was aspirated from the midline cyst contained some spermatozoa on examination under light microscopy. Preoperative cystoscopy revealed a narrowing of the prostatic urethra near the verumontanum due to a midline prostatic cyst (Fig. 3A). Therefore, a diagnosis of a EDO was made and TUREJD was planned.
Under spinal anesthesia, the patient was placed in the lithotomy position. A 10 mL diluted indigo-carmine solution was injected through a midline cyst guided TRUS. Using a 24 Fr resectoscope (Karl Storz, Tuttlingen, Germany) with a laser bridge and a Ho:YAG laser with a 550 µm laser fiber (Lumenis, Yokneam, Israel), unroofing of the midline prostate cyst was performed. During the unroofing process, the power was set at 2 J and 10 Hz. After the process, the diluted indigo-carmine solution was extravasated to the surrounding area. When sufficient space at the prostatic urethra was secured following incision with the Ho:YAG laser, a monopolar TUR was performed (Fig. 3B and C). Using TUR, the cystic wall was completely resected and a guidewire was inserted through the ejaculatory duct. The ejaculatory ducts and their wall were visualized using a 6.5 Fr semi-rigid ureteroscope (Richard Wolf GmbH, Knittlingen, Germany) and appeared to be normal (Fig. 3D).
The patient was discharged the following day after the Foley catheter was removed. After a month, the patient did not have any lower urinary tract symptoms. A month later, postoperative semen analysis showed normal findings with a 3 mL volume. Concentration of spermatozoa was 15.2×106/mL.
In patients with suspected EDO, the standard procedure has become TUREJD, which was described by Farley and Barnes in 1973.7 TUREJD can be performed with the general equipments for transurethral resection of the prostate.8 After a resectoscope is introduced into the urthera, the proximal verumontanum, which may be enlarged, can be resected by a cutting loop. Classical TUREJD is carried out using a pure cutting current without electrocoagulation.9 One to two chips are usually resected, removing the proximal verumontanum only. If bleeding is encountered, gentle coagulation is recommended to avoid the ejaculatory ducts. A catheter is inserted into the bladder and is left in place for a few hours in the recovery room. Postoperative urinary retention can occur after catheter removal, particularly in patients with a prior voiding dysfunction.
Schroeder-Printzen, et al.10 reported their surgical experience in sixteen infertile patients with EDO. They performed a combination of transurethral incision and resection using the Tuner-Warwick hook and TUR roof. With their technique, unroofing of all the central cysts following to positive results of intracystic dye test were carried out. With 15 patients with symptomatic EDO undergoing TUREJD, Johnson, et al.11 evaluated the diameter of seminal vesicles and considered dilated when their diameters were 12 mm or longer on TRUS. Each man was treated with TUREJD using a conventional resecting loop in the midline of the proximal verumontanum. They concluded that patients with symptomatic EDO who underwent TUREJD demonstrated improvements in their ejaculation, sensation of orgasm, semen analysis values and fertility. Recently, Wang, et al.12 reported interesting results on transurethral seminal vesiculoscopy for EDO. Twenty-one patients underwent their procedures, and a stone in the ejaculatory duct was removed in 5 cases, using a Ho:YAG laser. They concluded that their results had fewer complications and more optimal sperm recovery than the conventional method. Previous studies showed relatively good surgical outcomes.
In our case, we performed unroofing of a prostatic cyst using the Ho:YAG laser because of narrow prostatic urethra. The advantages of the Ho:YAG laser are as follows: precise unroofing using a small diameter laser fiber and avoidance of unnecessary coagulation, thereby minimizing damage to adjacent structures. In patients with EDO, this hybrid method may be a safe and satisfactory alternative treatment option to conventional TUREJD.
Figures and Tables
 | Fig. 1Transrectal ultrasonography revealed (A) a midline prostatic cyst with an approximate diameter of 1.5 cm (white arrow) with (B) dilated seminal vesicles. |
 | Fig. 2T2-weighted magnetic resonance image and seminal vesiculography. (A and C) Approximately 2 cm sized cystic lesion (white arrows) was located in the prostate. (B, C and D) Mild dilatation of the seminal vesicles was observed. (E) The seminal vesicles and midline cyst (white arrow head) were filled with contrast media under seminal vesiculography. |
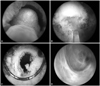 | Fig. 3Hybrid technique for complete ejaculatory duct obstruction. (A) Small space of the prostatic urethra. (B) Using Ho:YAG laser with a 550 µm laser fiber (Lumenis, Yokneam, Israel), unroofing of midline prostate cyst was performed. (C) Using TUR, the cystic wall was completely resected and a guidewire was inserted through the ejaculatory duct. (D) The ejaculatory ducts and its wall were visualized using a 6.5 Fr semi-rigid ureteroscope (Richard Wolf GmbH, Knittlingen, Germany). Ho:YAG, holmium:yttriumaluminium garnet; TUR, transurethral resection. |
References
1. Bang JK, Lim JJ, Choi J, Won HJ, Yoon TK, Hong JY, et al. Reversible infertility associated with testosterone therapy for symptomatic hypogonadism in infertile couple. Yonsei Med J. 2013; 54:702–706.

2. Jarow JP. Seminal vesicle aspiration in the management of patients with ejaculatory duct obstruction. J Urol. 1994; 152:899–901.

3. Ozgök Y, Tan MO, Kilciler M, Tahmaz L, Kibar Y. Diagnosis and treatment of ejaculatory duct obstruction in male infertility. Eur Urol. 2001; 39:24–29.

4. Pryor JP, Hendry WF. Ejaculatory duct obstruction in subfertile males: analysis of 87 patients. Fertil Steril. 1991; 56:725–730.

5. Yurdakul T, Gokce G, Kilic O, Piskin MM. Transurethral resection of ejaculatory ducts in the treatment of complete ejaculatory duct obstruction. Int Urol Nephrol. 2008; 40:369–372.

7. Farley S, Barnes R. Stenosis of ejaculatory ducts treated by endoscopic resection. J Urol. 1973; 109:664–666.

8. Park MS, Kim YS, Yoon YR. A case of infertility because of ejaculatory duct obstruction. Korean J Urol. 1992; 33:917–921.
9. Fisch H, Lambert SM, Goluboff ET. Management of ejaculatory duct obstruction: etiology, diagnosis, and treatment. World J Urol. 2006; 24:604–610.

10. Schroeder-Printzen I, Ludwig M, Köhn F, Weidner W. Surgical therapy in infertile men with ejaculatory duct obstruction: technique and outcome of a standardized surgical approach. Hum Reprod. 2000; 15:1364–1368.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download