1) fresh in vitro fertilization cycle
2) singleton pregnancy at the initial ultrasonographic examination
3) maintained pregnancy for more than 26 weeks of gestation
4) completed antenatal care and delivery in a single center
5) two or more transvaginal ultrasonograpic examinations before 12 weeks of gestation, and performed by three infertility subspecialists (authors YSY, EJP, and WIP)
6) complete medical and obstetric records.
Abstract
The aim of this study is to assess the association between crown-rump length (CRL) measured before the 10th gestational week and birth weight. Results from 316 transvaginal ultrasonography scans at the 46th, 53rd, 60th, 67th, and 74th days of pregnancy were compared in low birth weight (LBW) versus normal birth weight groups. A positive correlation between CRL and birth weight was observed when CRL was measured at days 60, 67, and 74. CRL measured on the 67th day of pregnancy was significantly smaller in the LBW group than in the normal birth weight group. A cut-off value of CRL=26.5 mm measured at day 67 has the highest power to predict LBW.
Low birth weight (LBW) infants are at increased risk of perinatal and infant death.1 LBW newborns have also been identified as an at-risk group for a number of health problems later in life.2 For this reason, the factors determining birth weight have been the focus of clinical interest for many years.
It has previously been suggested that variations in fetal size are largely determined in the second half of pregnancy. In 1993, however, a single study demonstrated a correlation between first-trimester crown-rump length (CRL) and birth weight.3 This finding has been interpreted to indicate that variations in fetal growth begin during the first trimester. Consequently, one large-scale retrospective study demonstrated that fetuses smaller than expected in the first trimester (on the basis of menstrual history) had a higher likelihood of LBW and premature delivery.4 Several recent studies have shown that the first-trimester CRL can predict whether the fetus is large or small for gestational age (LGA or SGA, respectively).5,6 However, the results of these studies were based on ultrasonography performed after 10 weeks of gestation. To our knowledge, whether or not CRL measured before the 10th gestational week is related to birth weight has never been assessed. Moreover, the CRL cut-off value to predict LBW has never been documented.
The purpose of this study is to assess the association between CRL measured before the 10th gestational week and birth weight. We also determined the optimal CRL cut-off value to predict LBW.
The medical records of ultrasonographic examinations performed between 2003 and 2009 at two in vitro fertilization centers were obtained along with women's medical and obstetrical histories, antenatal complications, and pregnancy outcomes. The inclusion criteria of the study subjects were women who had:
We excluded women with severe medical diseases and fetal malformations. A total of 148 women were included.
Total of 632 ultrasonographic scans were performed from 39th to 84th day of gestation for these women. Among these, 316 scans of day 46, 53, 60, 67 and 74 were analyzed. The day of oocyte aspiration was designates as a reference to calculate gestational age (14th day of pregnancy).
The correlation between CRL measured on a specific date and birth weight was analyzed using Pearson's regression test. The difference in CRL between normal and LBW groups was analyzed using the Mann-Whitney U test. The receiver operating characteristic (ROC) curve was used to determine the sensitivity and specificity of CRL measurement to predict LBW.
The mean age of the study subjects was 32.8 years (range: 21-43). The mean gestational age was 38.7 weeks (range: 21-41). The mean birth weight of the babies was 3166 g (range: 1420-4150). Among the 148 newborns, 14 babies weighed less than 2500 g at birth, and 18 were delivered before 37 weeks of gestation.
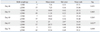
A positive correlation between CRL and birth weight was observed when CRL was measured at gestational days 60, 67, and 74 (Table 1). This positive correlation was repeated at the same gestational days when only term pregnancies were analyzed (Table 2). No association was observed between CRL and gestational age on any other dates of CRL measurement (Table 1). CRL measured at day 67 differed significantly between LBW and normal birth weight groups. The difference was not significant when CRL was measured on other days (Table 3).
In the ROC curve, days 60, 67, and 74 exhibited larger areas under the curve than days 46 and 54. The cut off value of 26.5 mm measured at day 67 had the highest power to predict LBW (sensitivity: 83.3% and specificity: 73.7%) (Fig. 1).
The main results of this study are that the CRL measured in the early first trimester of pregnancy is closely associated with birth weight, and that the accuracy of birth weight prediction is particularly high at day 67 (9+3 week) of pregnancy. This is the first report to demonstrate the CRL cut-off value that optimally predicts LBW.
Smith, et al.4 observed that a CRL discrepancy of 2-6 days smaller than expected is related to an increased risk of LBW (OR 1.7), but is not associated with perinatal death. In pregnancies conceived by controlled ovarian hyperstimulation, a strong association has been observed between fetal growth during the first trimester and birth weight, suggesting that impairment of fetal growth starts in the first trimester.7 In that study, a CRL discrepancy of 2-6 days is associated with an increased risk of SGA (OR 1.1), intrauterine growth restriction (OR 2.8), and preterm delivery before 32 weeks (OR 2.0). Another study observed a correlation between the CRL Z-score and birth weight Z-score.8 In agreement with these findings, our own series reveals a relationship between CRL in the first trimester and birth weight. New knowledge proven by this study is that this relationship is significant from the day 60 (8+3 week) of pregnancy. Contrary to other studies, our data failed to demonstrate a relationship between CRL and duration of pregnancy.
An advantage of this study is that their dates of ovulation are clearly documented because the subjects were conceived by in vitro fertilization only. Most previous studies that calculated gestational age relied on menstrual history or included women who had conceived by intrauterine insemination. As ovulation occurs between 8 and 40 h after the luteinizing hormone peak, the timing of ovulation cannot be precisely documented even in the intrauterine insemination cycle.9,10 The other advantage is setting the cut-off value. Previous studies used CRL or Z-score discrepancies as an independent variable. Even though a cut-off value is more clinically relevant than CRL or Z-score discrepancies, this study can only suggest the timing of the measurement at day 67 (9+3 week) of pregnancy. A larger scale study assessing the cut-off value of the other days of early pregnancy may give rise to more practical information.
The inter- and intra-observer variation could not be addressed because this is a retrospective study. The other drawback of this study is a small number of SGA group which affects the statistical power.
Our preliminary data demonstrate the likelihood that CLRs less than the suggested cut-off value will result in an LBW infant. This result can be used to convey gestational age-specific CRL to the antenatal caregivers of women who have conceived by in vitro fertilization.
Figures and Tables
Fig. 1
ROC curve for prediction of low birth weight (<2500 g) for each ultrasonography date. Gestational days 60, 67 and 74 have larger areas under the curve than other days. ROC, receiver operating characteristic.

Table 1
Analysis of Correlations between CRL and Birth Weight and CRL and Gestational Age on Each Day of Ultrasonography

ACKNOWLEDGEMENTS
The authors gratefully acknowledge the contribution of Drs. Yong-Kyun Cho, Seo-You Hong, and Yong-Soo Seo for their scientific comments. We are also grateful to Ms. Hye-Joo Hwang for technical assistance.
References
1. Kramer MS. Determinants of low birth weight: methodological assessment and meta-analysis. Bull World Health Organ. 1987; 65:663–737.
2. Ligi I, Grandvuillemin I, Andres V, Dignat-George F, Simeoni U. Low birth weight infants and the developmental programming of hypertension: a focus on vascular factors. Semin Perinatol. 2010; 34:188–192.

3. Dickey RP, Gasser RF. Ultrasound evidence for variability in the size and development of normal human embryos before the tenth post-insemination week after assisted reproductive technologies. Hum Reprod. 1993; 8:331–337.

4. Smith GC, Smith MF, McNay MB, Fleming JE. First-trimester growth and the risk of low birth weight. N Engl J Med. 1998; 339:1817–1822.

5. Pardo J, Peled Y, Yogev Y, Melamed N, Ben-Haroush A. Association of crown-rump length at 11 to 14 weeks' gestation and risk of a large-for-gestational-age neonate. J Ultrasound Med. 2010; 29:1315–1319.

6. Thorsell M, Kaijser M, Almström H, Andolf E. Large fetal size in early pregnancy associated with macrosomia. Ultrasound Obstet Gynecol. 2010; 35:390–394.

7. Bukowski R, Smith GC, Malone FD, Ball RH, Nyberg DA, Comstock CH, et al. Fetal growth in early pregnancy and risk of delivering low birth weight infant: prospective cohort study. BMJ. 2007; 334:836.

8. Salomon LJ, Hourrier S, Fanchin R, Ville Y, Rozenberg P. Is first-trimester crown-rump length associated with birthweight? BJOG. 2011; 118:1223–1228.

9. Testart J, Frydman R. Minimum time lapse between luteinizing hormone surge or human chorionic gonadotropin administration and follicular rupture. Fertil Steril. 1982; 37:50–53.

10. Garcia JE, Jones GS, Wright GL Jr. Prediction of the time of ovulation. Fertil Steril. 1981; 36:308–315.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download