Abstract
Purpose
Venous thromboembolism (VTE), including deep vein thrombosis and pulmonary embolism, is a serious and life-threatening complication in elderly (older than 65 years) patients undergoing hip fracture surgery (HFS). However, few have reported on the influences of VTE on postoperative rehabilitation in these patients. This study was performed to determine whether VTE affects clinical
outcomes in patients who underwent HFS.
Materials and Methods
We retrospectively evaluated 330 HFSs in 325 consecutive patients, which were performed from January 2009 to June 2010. From chart review, we identified 15 patients with symptomatic VTE. We compared Geriatric depression scale, Modified Barthel index and Berg balance scale scores as well as 10 meter gait speed at discharge and hospital stay between a symptomatic VTE group and a non-VTE group.
Venous thromboembolism (VTE), including deep vein thrombosis (DVT) and pulmonary embolism (PE), is a potentially life-threatening complication in patients undergoing hip fracture surgery (HFS). Among different case series, the incidence of symptomatic VTE without any thromboprophylaxis following HFS widely ranged from 3% to 50%.1-6
Previous studies on VTE have mainly focused on the incidence, risk factors and prophylactic modalities.1,7-9 VTE following HFS in elderly patients with medical co-morbidities could affect clinical outcomes, ambulatory function and hospital stay after the operation. However, the effect of symptomatic DVT and PE on postoperative rehabilitation in elderly HFS patients is rarely mentioned.10
We therefore attempted to discern whether symptomatic VTE affects postoperative rehabilitation in elderly HFS patients.
From January 2009 to June 2010, 288 patients (293 hips) older than 65 years of age underwent hip surgery due to a femoral neck fracture or an intertrochanteric fracture at our institute. There were 201 women and 87 men with a mean age of 79.6 years (range, 65-96 years) at the time of operation. Their mean body mass index was 21.8 kg/m2 (range, 13.3-32.0 kg/m2). Regional anesthesia was used in 270 surgeries and general anesthesia in 23. Hip arthroplasty was performed in 259 hips and internal fixation in 34.
Perioperatively, 8 patients (8 hips) were treated with anticoagulants: 4 patients (4 hips) due to previous history of a thrombo-embolic event, 3 patients (3 hips) due to cardiac disease and 1 patient (1 hips) due to cerebro-vascular disease. In the remaining 280 patients, thigh-length antiembolic stockings were applied and the ankle pump was encouraged without any pharmacological thromboprophylaxis.
On postoperative day 1 to 3, closed suction drainage was removed. On postoperative day 3 to 10, patients were mobilized with protected weight-bearing as tolerated along with use of assistive devices (walker or crutches).
As the patients' walking ability improved, their assistive devices were changed appropriately by a physical therapist. Patients who could not ambulate independently even at 1 week after the operation were transferred to the rehabilitation unit for ambulatory training.
During the hospitalization period, we carefully monitored clinical signs of DVT including pain and tenderness in the calf or thigh, swelling or erythema of the operated limb, and a positive Homans' sign. We suspected DVT or PE in 37 patients who undertook consultation with cardiovascular physicians. A diagnosis of DVT was made using duplex ultrasonography or lower extremity CT angiography. PE was confirmed by a ventilation/perfusion scan or pulmonary CT angiography.
After discharge, patients were routinely followed up at 6 weeks, 3 months and 6 months. Geriatric depression scale, Modified Barthel index, Berg balance scale and 10 meter gait speed were evaluated at 6 weeks follow-up.
The Geriatric depression scale comprises a 30-item easy-to-administer inventory, and is one of the most widely used instruments for screening elderly persons for depression.6,11,12
The Modified Barthel index evaluates 10 aspects of daily living, with a maximal value of 100 and a minimal value of 0, in terms of functional status and degree of disability. A score of 100 indicates the absence of disability.13
The Berg balance scale evaluates ability of 14 tasks to challenge balance during sitting, standing or stepping. It has a minimum value of 0 and maximum value of 56, and higher values indicate better balance.14
We compared VTE patients and non-VTE patients using Fisher's exact test for categorized data and Mann-Whitney U test for continuous data. p-values less than 0.05 were considered to be statistically significant.
The design and protocol of this study were reviewed and approved by the institutional review board of our hospital, who waived informed consent (IRB No. B-1006-103-118).
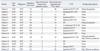
Fifteen patients (5.1%) were diagnosed as having a VTE: 5 patients had symptomatic DVT, 6 had both symptomatic DVT and PE, and 4 had symptomatic PE. Diagnoses were made at 5 to 56 days after the operation (mean, 16.3 days), and these 15 patients were treated with heparin and/or warfarin after the diagnosis (Table 1).
In total, 28 patients who did not undergo the rehabilitative evaluations and 12 patients who could not answer the questions on the Geriatric depression scale were excluded. The remaining 248 patients, 234 non-VTE patients and 14 VTE patients, were included in the comparison.
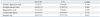
Baseline characteristics were similar between VTE patients and non-VTE patients (Table 2).
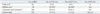
Moreover, there were no significant differences between VTE patients and non-VTE patients in terms of Geriatric depression scale, Modified Barthel index, Berg balance scale and 10 meter gait speed (Table 3).
Unlike Western countries who report high incidences of DVT and PE after HFS, symptomatic DVT and PE are uncommon in East Asian patients undergoing HFS. Accordingly, in this study, we attempted to determine whether the occurrence of symptomatic DVT or PE affected rehabilitation after HFS.
In this study, incidence of VTE was 5.1% even without any chemical thromboprophylaxis, which was comparable with that for Western patients after HFS who underwent chemical thromboprophylaxis (Table 4).15 One explanation for the low incidences of symptomatic VTE in our study might be the low prothrombotic risk factors and the absence of some genetic factors involved in VTE in East Asian patients.16-21 Old age, female gender, obesity, underlying disease, type of anesthesia, and prolonged immobilization in bed are known to be risk factors of VTE according to studies from Western countries.22-25 In our study, no variables were shown to be risk factors of VTE, and only old age showed marginal significance (p=0.062). These results may be explained by ethnic differences between our patients and Western patients or our patient number of VTE patients might not have been large enough to detect the significance of these factors.
In terms of rehabilitation after HFS, the objective of this study, functional recovery as reflected by ambulatory state, the Modified Barthel index, Berg balance scale and gait speed was not significantly decreased even in cases of symptomatic VTE. However, in this study, hospital stay was prolonged in VTE patients (26.3±17.1 vs. 37.7±15.4, p=0.012). After surgery, delayed mobilization, a well-known risk factor for VTE,23-26 might be the reason for the pronged hospital stay and increased risk of VTE occurrence in these patients. In addition, titration of oral warfarin might be necessary in patients with symptomatic VTE before discharge.
This study has several limitations as a retrospective review of prospectively collected data. First, rehabilitative evaluations were available only in 248 patients. The outcomes of other unavailable 40 patients could affect our results. Second, the fact that the rehabilitation was not affected by occurrence of VTE could be related to relatively small numbers of patients with inadequate power to detect differences. Third, we did not perform studies to confirm asymptomatic VTE and could not determine the incidence of asymptomatic VTE. It might be argued that VTE patients might have received more intensive rehabilitation than non-VTE patients, which might have affected the results. However, the duration of physical therapy was similar in the two groups.
In conclusion, our study showed that occurrence of symptomatic DVT and PE did not affect rehabilitation after HFS in East Asian patients with a low incidence of symptomatic VTE.
Figures and Tables
References
1. Haake DA, Berkman SA. Venous thromboembolic disease after hip surgery. Risk factors, prophylaxis, and diagnosis. Clin Orthop Relat Res. 1989; 212–231.
2. Todd CJ, Freeman CJ, Camilleri-Ferrante C, Palmer CR, Hyder A, Laxton CE, et al. Differences in mortality after fracture of hip: the east Anglian audit. BMJ. 1995; 310:904–908.

3. Zahn HR, Skinner JA, Porteous MJ. The preoperative prevalence of deep vein thrombosis in patients with femoral neck fractures and delayed operation. Injury. 1999; 30:605–607.

4. Geerts WH, Pineo GF, Heit JA, Bergqvist D, Lassen MR, Colwell CW, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004; 126:3 Suppl. 338S–400S.
5. Dhillon KS, Askander A, Doraismay S. Postoperative deep-vein thrombosis in Asian patients is not a rarity: a prospective study of 88 patients with no prophylaxis. J Bone Joint Surg Br. 1996; 78:427–430.
6. Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982-1983; 17:37–49.

7. Eriksson BI, Bauer KA, Lassen MR, Turpie AG. Steering Committee of the Pentasaccharide in Hip-Fracture Surgery Study. Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after hip-fracture surgery. N Engl J Med. 2001; 345:1298–1304.

8. Hitos K, Fletcher JP. Venous thromboembolism and fractured neck of femur. Thromb Haemost. 2005; 94:991–996.

9. Sasaki S, Miyakoshi N, Matsuura H, Saitoh H, Kudoh D, Shimada Y. Prospective randomized controlled trial on the effect of fondaparinux sodium for prevention of venous thromboembolism after hip fracture surgery. J Orthop Sci. 2009; 14:491–496.

10. Cordell-Smith JA, Williams SC, Harper WM, Gregg PJ. Lower limb arthroplasty complicated by deep venous thrombosis. Prevalence and subjective outcome. J Bone Joint Surg Br. 2004; 86:99–101.
11. Bae JN, Cho MJ. Development of the Korean version of the Geriatric Depression Scale and its short form among elderly psychiatric patients. J Psychosom Res. 2004; 57:297–305.

12. Montorio I, Izal M. The Geriatric Depression Scale: a review of its development and utility. Int Psychogeriatr. 1996; 8:103–112.

13. Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol. 1989; 42:703–709.

14. Berg KO, Maki BE, Williams JI, Holliday PJ, Wood-Dauphinee SL. Clinical and laboratory measures of postural balance in an elderly population. Arch Phys Med Rehabil. 1992; 73:1073–1080.
15. Lieberman DV, Lieberman D. Proximal deep vein thrombosis after hip fracture surgery in elderly patients despite thromboprophylaxis. Am J Phys Med Rehabil. 2002; 81:745–750.

16. Klatsky AL, Armstrong MA, Poggi J. Risk of pulmonary embolism and/or deep venous thrombosis in Asian-Americans. Am J Cardiol. 2000; 85:1334–1337.

17. Westrich GH, Weksler BB, Glueck CJ, Blumenthal BF, Salvati EA. Correlation of thrombophilia and hypofibrinolysis with pulmonary embolism following total hip arthroplasty: an analysis of genetic factors. J Bone Joint Surg Am. 2002; 84-A:2161–2167.
18. Kim YH, Kim JS. The 2007 John Charnley Award. Factors leading to low prevalence of DVT and pulmonary embolism after THA: analysis of genetic and prothrombotic factors. Clin Orthop Relat Res. 2007; 465:33–39.

19. Pellegrini VD Jr, Clement D, Lush-Ehmann C, Keller GS, Evarts CM. The John Charnley Award. Natural history of thromboembolic disease after total hip arthroplasty. Clin Orthop Relat Res. 1996; 27–40.
20. Thomas DP, Roberts HR. Hypercoagulability in venous and arterial thrombosis. Ann Intern Med. 1997; 126:638–644.

22. Mraovic B, Hipszer BR, Epstein RH, Pequignot EC, Parvizi J, Joseph JI. Preadmission hyperglycemia is an independent risk factor for in-hospital symptomatic pulmonary embolism after major orthopedic surgery. J Arthroplasty. 2010; 25:64–70.

23. Sikorski JM, Hampson WG, Staddon GE. The natural history and aetiology of deep vein thrombosis after total hip replacement. J Bone Joint Surg Br. 1981; 63-B:171–177.

24. Memtsoudis SG, Besculides MC, Gaber L, Liu S, González Della Valle A. Risk factors for pulmonary embolism after hip and knee arthroplasty: a population-based study. Int Orthop. 2009; 33:1739–1745.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download