Abstract
Purpose
There are conflicting results surrounding the prognostic significance of epidermal growth factor receptor (EGFR) status in glioblastoma (GBM) patients. Accordingly, we attempted to assess the influence of EGFR expression on the survival of GBM patients receiving postoperative radiotherapy.
Materials and Methods
Thirty three GBM patients who had received surgery and postoperative radiotherapy at our institute, between March 1997 and February 2006, were included. The evaluation of EGFR expression with immunohistochemistry was available for 30 patients. Kaplan-Meier survival analysis and Cox regression were used for statistical analysis.
Results
EGFR was expressed in 23 patients (76.7%), and not expressed in seven (23.3%). Survival in EGFR expressing GBM patients was significantly less than that in non-expressing patients (median survival: 12.5 versus 17.5 months, p=0.013). Patients who received more than 60 Gy showed improved survival over those who received up to 60 Gy (median survival: 17.0 versus 9.0 months, p=0.000). Negative EGFR expression and a higher radiation dose were significantly correlated with improved survival on multivariate analysis. Survival rates showed no differences according to age, sex, and surgical extent.
Glioblastoma (GBM) is the most common primary malignant brain tumor in adults. Due to its diffuse infiltrative growth, radical resection is usually impossible and most recurrences occur in the vicinity of original sites.1 Ever since postoperative radiotherapy was introduced survival has improved;2,3 however, the prognosis of GBM is remains poor with a median survival of around one year. The addition of temozolomide to radiotherapy has enhanced survival, but only by about 2-3 months.4,5 These poor prognoses highlight the need for new effective therapeutic approaches, in addition to current treatments, to improve survival outcomes.
In contrast to normal cells, whose growth is regulated by organized growth stimulatory pathways, the growth of cancer cells is dysregulated and activated constitutively by multiple pathways. Epidermal growth factor receptor (EGFR) plays a central role in both development and tumorigenesis within many organ systems, including the central nervous system.6 The EGFR gene is the most commonly amplified gene in GBMs and is amplified several times in tumor cells, compared to normal cells.7-9 Overexpression of EGFR appears to correlate with glioma grade, which is observed in about 40-50% of GBMs, compared to 10-26% of anaplastic astrocytomas.10,11 Therefore, EGFR may potentially be a grading markers of GBMs.
Among researchers the prognostic significance of EGFR expression in GBM patients is still debated. Some have found poor prognoses to be associated with amplification of the EGFR gene or overexpression of EGFR in GBM patients,12-17 while others have not.11,18-24 Therefore, we conducted this retrospective analysis to evaluate the impact of EGFR expression on the clinical outcomes of GBM patients who received surgery and postoperative radiotherapy at a single institution in order to obviate treatment related biases as much as possible.
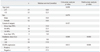
Thirty three consecutive GBM patients who had received both surgery and postoperative radiotherapy at our institution, between March 1997 and February 2006, were reviewed. As tissue specimens were lost for three patients, only 30 patients were finally included in the analysis. Analysis of these patients was approved by the Institutional Review Board. Patients were followed until their death, with four patients still living at the time of the analysis. All patients received conventional radiotherapy, 1.8-2.0 Gy/day, for about 4-6 weeks after operation. Three patients received less than 50 Gy because of tumor progression at 44.0 Gy, sepsis attributed to aspiration pneumonia at 12.6 Gy, and refusal of further radiotherapy at 37.8 Gy. Excluding these, the remaining 27 patients received doses of 50 Gy or greater (median: 61.2 Gy, range: 55.2-65.1 Gy). Median age at diagnosis was 55.5 years (range: 24-77 years). There were 18 male and 12 female patients. Resection of at least 50% of tumor was done in 20 patients, less than 50% tumor resection in eight, and biopsy in two patients (Table 1).
Formalin-fixed and paraffin embedded tissue blocks were cut serially into 4 µm thick sections. All processes of immunohistochemistry were performed automatically using a Ventana autostainer (Benchmark; Ventana Medical Systems, Tucson, AZ, USA). For antigen retrieval, retrieval solution (Ventana) was automatically poured on the sections, and then the sections were heated at 100℃ for 60 minutes. Endogenous peroxide activity was blocked by immersion in 3% hydrogen peroxide for four minutes. With primary antibodies for EGFR (mouse monoclonal antibody, 1 : 1, Zymed; Invitrogen, Camarillo, CA, USA), the tissue sections were incubated for 32 minutes at 36℃. Immunoperoxidase staining was performed with the DAB system (iView DAB detection kit; Ventana Medical Systems, Tucson, AZ, USA), and then the sections were lightly counterstained with hematoxylin.
Two pathologists independently interpreted the results of immunohistochemical studies without any clinical or other histological information. Intensity of staining was assessed gradually (0, negative; 1, weak; 2, intermediate; 3, strong), and a grade of more than two (intermediate or strong intensity) was considered representative of positive cells. The percentage of positive cells in a tumor mass was measured by the pathologists. Immunohistochemical staining was considered positive when more than 10% of tumor cells showed membranous or cytoplasmic immunoreactivity.
Fisher's exact test was used for the evaluation of the associations between EGFR expression and patient characteristics. Survival was measured from the date of the surgery for GBM. Survival analysis was carried out with the Kaplan-Meier method and a log rank test. Multivariate analysis was performed with a Cox proportional hazards model. Statistical analyses were performed using SPSS software version 17.0 (SPSS Inc., Chicago, IL, USA).
The expression of EGFR was positive in 23 patients among the 30 patients whose specimens were available for study (Table 1). EGFR expression was predominately located in the cell membrane of the GBM, followed by that in the cytoplasm (Fig. 1). Expression in the nuclear membrane was found in three patients. EGFR was strongly stained in all positive specimens, negating the need to perform analysis of intensity differences among positive slides. Instead, the percentage of EGFR positive cells out of all tumor cells was counted. EGFR expression was not different according to patient characteristics, such as age, sex, extent of surgical resection, and radiation dose (Table 2).
The median survival was 13.0 months, and 1- and 2-year survival rates were 63.3% and 16.7%, respectively. On univariate analysis, a higher radiation dose (>60 Gy vs. ≤60 Gy) and negative EGFR expression (negative vs. positive) were significantly correlated with improved survival, the median survivals of which were 17.0 months vs. 9.0 months (p=0.000) and 17.5 months vs. 12.5 months (p=0.013), respectively. After multivariate analysis, a higher radiation dose and negative EGFR expression remained significant in their association with improved survival (Table 3) (Fig. 2). Although the small patient number in each group may make the statistical difference thereof be of little importance, negative EGFR expression was significantly correlated with better survival in the patient groups of >60 Gy and ≤60 Gy (p=0.037 and p=0.020, respectively). There were four long-term survivors who were alive at the time of the analysis. The percentages of EGFR expressing cells in their specimens were at most 5%; three were 0% and one was 5%.
Although EGFR is the most commonly amplified gene in GBM patients, the prognostic significance of EGFR has remained controversial. EGFR expression can be examined at the gene, DNA, RNA, and protein level. To do so, immunohistochemistry has been widely used for the evaluation of EGFR expression on paraffin-embedded tumor specimens. However, the determination of EGFR immunoreactivity could be affected by multiple factors, such as the choice of fixative, the storage time of tumor tissue, the choice of antibody, and the lack of criteria for evaluation.25-28 Therefore, a method that is less dependent on the above factors should be developed.
The present study used immunohistochemical staining for the analysis of EGFR expression in GBM tissues. In the literature, results for the influence of EGFR expression on survival according to immunohistochemical staining differed among researchers (Table 4). Some insisted that EGFR expression had a negative effect on survival compared to non-expression.16,17 Others argued that EGFR expression had an insignificant effect on survival.19,20 The median survival of patients exhibiting EGFR expressing GBM cells was significantly less than that of EGFR negative patients in the present study.
The definition of EGFR positivity can be influenced by stain intensity and the fraction of stained cells. Because the intensity of EGFR expression was homogenously strong in all positive specimens of this study, guidelines for positivity could be drawn according to the percentage of positive cells without consideration of any staining intensity. In addition to the initial EGFR positivity, based on the presence of any positive cells, several cutoff points were taken into consideration for further analysis (Table 5). When 10% and 20% positive cells among GBM cells were used as the lowest cutoff points for EGFR positivity, the survival rates of EGFR positive patients were significantly lower than that of EGFR negative patients. Moreover, survival was not different when the lowest cutoff point of 30% was applied.
Analyzing Radiation Therapy Oncology Group (RTOG) trial data, Chakravarti, et al.18 showed that immunohistochemically determined total EGFR levels were not of prognostic value in GBM patients. They selected 155 GBM patients from the RTOG trials of 7401, 7918, 8302, 8409, 9006, 9305, 9602, and 9806. However, the radiotherapy methods applied in the trials were heterogenous. Irradiation volume ranged from peritumoral to the whole brain, in addition to varying radiation doses from 48 Gy to 81.6 Gy, and fractionation schemes from conventional, hyperfraction, to stereotactic radiosurgery boost. Therefore, in order to obtain a reliable conclusion, it was necessary to conduct an EGFR study with data from more homogenously managed patients. Patients in the present study were treated at a single hospital, so they were considered to have been managed similarly. The present study observed significantly poorer outcomes in EGFR expressing patients; however, these results were observed in only a small number of patients, which may make the results less valuable.
Because most recurrences in GBM patients occur within two cm of the pre-surgical, initial tumor margin,1 delivering a larger dose to improve local control and survival is necessary. However, confirmatory data to support that irradiation of more than 60 Gy improves prognoses in GBM patients is lacking.29,30 Recently, RTOG conducted a radiation dose escalation study using three dimensional conformal radiotherapy (3DCRT), and found that delivering a higher than standard (60 Gy) radiotherapy dose was feasible with an acceptable risk of late central nervous system toxicity.31 This study applied 3DCRT in all patients, and the patients that received greater than 60 Gy demonstrated better survival than those irradiated with 60 Gy or less. The survival conbenefit of patients receiving higher than 60 Gy was sustained after excluding less than 50 Gy (data not shown) in the analysis. Therefore, radiation dose escalation trials should be tried with sophisticated radiotherapy methods, such as 3DCRT, intensity modulated radiotherapy, stereotactic radiotherapy, radiosurgery, and proton therapy.
The effect of surgical resection extent in the treatment of GBM is still under debate,32-35 but an inferior survival in patients who undergo biopsy only compared to surgery was evident in most studies.32,36,37 We also found that survival was lower in patients that underwent less than 10% resection compared to patients who underwent greater surgical resection, although the difference was not significant (Table 3). Moreover, there were only two patients with less than 10% resection in this study, so further analysis with more patients may provide more statistically powerful results.
To obtain more confirmatory or less biased results of EGFR expression on survival in GBM patients, data from a large number of GBM patients who were treated homogenously are needed. When the prognostic significance of EGFR expression is verified, we should have another option for which to treat GBM patients, in addition to the unsatisfactory treatment modalities currently available.
Figures and Tables
Fig. 1
Immunohistochemical staining of EGFR in glioblastoma tissue. The tumor cells of a glioblastoma showed large irregular nuclei and abundant cytoplasm on H&E staining (A), and were strongly positive for EGFR (B). Tumor cells of another patient showed negativity for EGFR (C) (×400). EGFR, epidermal growth factor receptor.

Fig. 2
EGFR expression in relation to survival in glioblastoma patients. (A) Median survival times of negative and positive EGFR expression were 17.5 and 12.5 months, respectively (p=0.013). Survival differences according to EGFR expression were sustained in patients stratified according to radiation doses of up to 60 Gy (p=0.020) (B) and more than 60 Gy (p=0.037) (C). EGFR, epidermal growth factor receptor.
References
1. Wallner KE, Galicich JH, Krol G, Arbit E, Malkin MG. Patterns of failure following treatment for glioblastoma multiforme and anaplastic astrocytoma. Int J Radiat Oncol Biol Phys. 1989. 16:1405–1409.

2. Andersen AP. Postoperative irradiation of glioblastomas. Results in a randomized series. Acta Radiol Oncol Radiat Phys Biol. 1978. 17:475–484.

3. Walker MD, Green SB, Byar DP, Alexander E Jr, Batzdorf U, Brooks WH, et al. Randomized comparisons of radiotherapy and nitrosoureas for the treatment of malignant glioma after surgery. N Engl J Med. 1980. 303:1323–1329.

4. Kocher M, Frommolt P, Borberg SK, Rühl U, Steingräber M, Niewald M, et al. Randomized study of postoperative radiotherapy and simultaneous temozolomide without adjuvant chemotherapy for glioblastoma. Strahlenther Onkol. 2008. 184:572–579.

5. Stupp R, Hegi ME, Mason WP, van den Bent MJ, Taphoorn MJ, Janzer RC, et al. Effects of radiotherapy with concomitant and adjuvant temozolomide versus radiotherapy alone on survival in glioblastoma in a randomised phase III study: 5-year analysis of the EORTC-NCIC trial. Lancet Oncol. 2009. 10:459–466.

6. Nicholas MK, Lukas RV, Jafri NF, Faoro L, Salgia R. Epidermal growth factor receptor - mediated signal transduction in the development and therapy of gliomas. Clin Cancer Res. 2006. 12:7261–7270.

7. Fuller GN, Bigner SH. Amplified cellular oncogenes in neoplasms of the human central nervous system. Mutat Res. 1992. 276:299–306.

8. Libermann TA, Nusbaum HR, Razon N, Kris R, Lax I, Soreq H, et al. Amplification, enhanced expression and possible rearrangement of EGF receptor gene in primary human brain tumours of glial origin. Nature. 1985. 313:144–147.

9. Wong AJ, Bigner SH, Bigner DD, Kinzler KW, Hamilton SR, Vogelstein B. Increased expression of the epidermal growth factor receptor gene in malignant gliomas is invariably associated with gene amplification. Proc Natl Acad Sci U S A. 1987. 84:6899–6903.

10. Salomon DS, Brandt R, Ciardiello F, Normanno N. Epidermal growth factor-related peptides and their receptors in human malignancies. Crit Rev Oncol Hematol. 1995. 19:183–232.

11. Waha A, Baumann A, Wolf HK, Fimmers R, Neumann J, Kindermann D, et al. Lack of prognostic relevance of alterations in the epidermal growth factor receptor-transforming growth factor-alpha pathway in human astrocytic gliomas. J Neurosurg. 1996. 85:634–641.

12. Etienne MC, Formento JL, Lebrun-Frenay C, Gioanni J, Chatel M, Paquis P, et al. Epidermal growth factor receptor and labeling index are independent prognostic factors in glial tumor outcome. Clin Cancer Res. 1998. 4:2383–2390.
13. Ruano Y, Ribalta T, de Lope AR, Campos-Martín Y, Fiaño C, Pérez-Magán E, et al. Worse outcome in primary glioblastoma multiforme with concurrent epidermal growth factor receptor and p53 alteration. Am J Clin Pathol. 2009. 131:257–263.

14. Shinojima N, Tada K, Shiraishi S, Kamiryo T, Kochi M, Nakamura H, et al. Prognostic value of epidermal growth factor receptor in patients with glioblastoma multiforme. Cancer Res. 2003. 63:6962–6970.
15. Smith JS, Tachibana I, Passe SM, Huntley BK, Borell TJ, Iturria N, et al. PTEN mutation, EGFR amplification, and outcome in patients with anaplastic astrocytoma and glioblastoma multiforme. J Natl Cancer Inst. 2001. 93:1246–1256.

16. Simmons ML, Lamborn KR, Takahashi M, Chen P, Israel MA, Berger MS, et al. Analysis of complex relationships between age, p53, epidermal growth factor receptor, and survival in glioblastoma patients. Cancer Res. 2001. 61:1122–1128.
17. Zhu A, Shaeffer J, Leslie S, Kolm P, El-Mahdi AM. Epidermal growth factor receptor: an independent predictor of survival in astrocytic tumors given definitive irradiation. Int J Radiat Oncol Biol Phys. 1996. 34:809–815.

18. Chakravarti A, Seiferheld W, Tu X, Wang H, Zhang HZ, Ang KK, et al. Immunohistochemically determined total epidermal growth factor receptor levels not of prognostic value in newly diagnosed glioblastoma multiforme: report from the Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys. 2005. 62:318–327.

19. Bouvier-Labit C, Chinot O, Ochi C, Gambarelli D, Dufour H, Figarella-Branger D. Prognostic significance of Ki67, p53 and epidermal growth factor receptor immunostaining in human glioblastomas. Neuropathol Appl Neurobiol. 1998. 24:381–388.

20. Donato V, Papaleo A, Castrichino A, Banelli E, Giangaspero F, Salvati M, et al. Prognostic implication of clinical and pathologic features in patients with glioblastoma multiforme treated with concomitant radiation plus temozolomide. Tumori. 2007. 93:248–256.

21. Galanis E, Buckner J, Kimmel D, Jenkins R, Alderete B, O'Fallon J, et al. Gene amplification as a prognostic factor in primary and secondary high-grade malignant gliomas. Int J Oncol. 1998. 13:717–724.

22. Newcomb EW, Cohen H, Lee SR, Bhalla SK, Bloom J, Hayes RL, et al. Survival of patients with glioblastoma multiforme is not influenced by altered expression of p16, p53, EGFR, MDM2 or Bcl-2 genes. Brain Pathol. 1998. 8:655–667.

23. Quan AL, Barnett GH, Lee SY, Vogelbaum MA, Toms SA, Staugaitis SM, et al. Epidermal growth factor receptor amplification does not have prognostic significance in patients with glioblastoma multiforme. Int J Radiat Oncol Biol Phys. 2005. 63:695–703.

24. Viana-Pereira M, Lopes JM, Little S, Milanezi F, Basto D, Pardal F, et al. Analysis of EGFR overexpression, EGFR gene amplification and the EGFRvIII mutation in Portuguese high-grade gliomas. Anticancer Res. 2008. 28:913–920.
25. Atkins D, Reiffen KA, Tegtmeier CL, Winther H, Bonato MS, Störkel S. Immunohistochemical detection of EGFR in paraffin-embedded tumor tissues: variation in staining intensity due to choice of fixative and storage time of tissue sections. J Histochem Cytochem. 2004. 52:893–901.

26. Derecskei K, Moldvay J, Bogos K, Tímár J. Protocol modifications influence the result of EGF receptor immunodetection by EGFR pharmDx in paraffin-embedded cancer tissues. Pathol Oncol Res. 2006. 12:243–246.

27. Kersting C, Packeisen J, Leidinger B, Brandt B, von Wasielewski R, Winkelmann W, et al. Pitfalls in immunohistochemical assessment of EGFR expression in soft tissue sarcomas. J Clin Pathol. 2006. 59:585–590.

28. Langner C, Ratschek M, Rehak P, Schips L, Zigeuner R. Are heterogenous results of EGFR immunoreactivity in renal cell carcinoma related to non-standardised criteria for staining evaluation? J Clin Pathol. 2004. 57:773–775.

29. Nelson DF, Diener-West M, Horton J, Chang CH, Schoenfeld D, Nelson JS. Combined modality approach to treatment of malignant gliomas--re-evaluation of RTOG 7401/ECOG 1374 with long-term follow-up: a joint study of the Radiation Therapy Oncology Group and the Eastern Cooperative Oncology Group. NCI Monogr. 1988. (6):279–284.
30. Souhami L, Seiferheld W, Brachman D, Podgorsak EB, Werner-Wasik M, Lustig R, et al. Randomized comparison of stereotactic radiosurgery followed by conventional radiotherapy with carmustine to conventional radiotherapy with carmustine for patients with glioblastoma multiforme: report of Radiation Therapy Oncology Group 93-05 protocol. Int J Radiat Oncol Biol Phys. 2004. 60:853–860.

31. Tsien C, Moughan J, Michalski JM, Gilbert MR, Purdy J, Simpson J, et al. Phase I three-dimensional conformal radiation dose escalation study in newly diagnosed glioblastoma: Radiation Therapy Oncology Group Trial 98-03. Int J Radiat Oncol Biol Phys. 2009. 73:699–708.

32. Simpson JR, Horton J, Scott C, Curran WJ, Rubin P, Fischbach J, et al. Influence of location and extent of surgical resection on survival of patients with glioblastoma multiforme: results of three consecutive Radiation Therapy Oncology Group (RTOG) clinical trials. Int J Radiat Oncol Biol Phys. 1993. 26:239–244.

33. Kowalczuk A, Macdonald RL, Amidei C, Dohrmann G 3rd, Erickson RK, Hekmatpanah J, et al. Quantitative imaging study of extent of surgical resection and prognosis of malignant astrocytomas. Neurosurgery. 1997. 41:1028–1036.

34. Sandberg-Wollheim M, Malmström P, Strömblad LG, Anderson H, Borgström S, Brun A, et al. A randomized study of chemotherapy with procarbazine, vincristine, and lomustine with and without radiation therapy for astrocytoma grades 3 and/or 4. Cancer. 1991. 68:22–29.

35. Lacroix M, Abi-Said D, Fourney DR, Gokaslan ZL, Shi W, DeMonte F, et al. A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg. 2001. 95:190–198.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download