Abstract
Purpose
Vascular disorders and viral infections are considered the main causes of sudden hearing loss (SHL), although its pathogenesis remain unclear. Treatments include carbogen inhalation and lipo-prostaglandin E1 (lipo-PGE1), both of which have circulation-enhancing effects. We investigated the effectiveness of carbogen inhalation and lipo-PGE1 in SHL.
Materials and Methods
This retrospective review included 202 patients with idiopathic SHL who visited our clinic within 14 days of symptom onset between January 2006 and June 2010. All patients received oral prednisolone for 10 days. Of the 202 patients, 44 received no additional treatment, 106 received additional carbogen inhalation, and 52 received additional lipo-PGE1. Hearing improvement was measured using Siegel's criteria.
Results
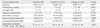
Overall recovery rates were 67.9% in the carbogen group, 53.8% in the lipo-PGE1 group, and 52.3% in the steroid-only control group (p=0.097). Limited to type 1 and type 2 categories of Sigels's criteria, the carbogen group had a significantly higher recovery rate (53.8%) than the lipo-PGE1 group (26.9%) and the steroid-only control group (38.6%) (p=0.005).
Sudden hearing loss (SHL) is considered a syndrome and not a diagnosis and defined as a hearing loss of at least 30 dB in three sequential frequencies occurring over 3 days or less.1 SHL was first reported by De Kleyn2 in 1944, there have been many studies regarding the disease, but the pathogenesis remains unclear. SHL involves a variety of causative factors, and therefore should be considered a syndrome rather than a single disease.3 The most common causes include viral infection and vascular disorders; other causes include rupture of the inner ear membrane, immune disorders, and acoustic tumors.4
The most widely accepted treatment for SHL is systemic corticosteroids,5 due to their ability to reduce inflammation, inhibit immune mechanisms, and regulate electrolyte balance. However, studies have shown that corticosteroid treatment is not significantly more effective than placebo, and includes serious side effects.6,7 Thus there have been continuous efforts to identify additional treatments.8 In the case of SHL caused by viral infection, studies on antiviral therapy have shown controversial therapeutic results.9
Vasodilators such as carbogen inhalation and lipoprostaglandin E1 (lipo-PGE1) have been used to treat SHL based on the theory that vasodilation of the inner ear may aid recovery if caused by a vascular disorder. Lipo-PGE1 is a prostanoid that acts as a vasodilator and improves vascular circulation. Carbogen inhalation increases arterial oxygen saturation and maximizes oxygen supply to the inner ear. Studies on the effects of carbogen and lipo-PGE1 in SHL have had controversical results. Shea and Kitabchi10 reported that carbogen inhalation had a therapeutic effect, while Cinamon, et al.6 found no therapeutic effect. Similarly, Zhuo, et al.11 reported that lipo-PGE1 had a therapeutic effect, while Ahn, et al.12 found no therapeutic effect. Despite controversial benefits, the theories remain that improving circulation may yield therapeutic results in cases where a vascular disorder underlies the SHL.
In this study, we compared 2 vasodilator treatments for SHL, carbogen inhalation and lipo-PGE1, to investigate their therapeutic effects.
This retrospective review was performed in 236 patients with SHL who visited our clinic between January 2006 and June 2010. All patients underwent a thorough history and physical examination, pure tone audiometry, speech audiometry, and impedence audiometry. Auditory Brainstem Response latency and temporal magnetic resonance imaging were selectively performed to rule out retrocochlear pathology. To minimize the bias, we excluded patients who presented more than 14 days of symptom onset and patients with other causes of hearing loss such as Meniere's disease, vestibular schwannoma, and ischemic brain lesion including AICA infarct.
All patients received identical initial treatment consisting of 1 mg/kg of prednisolone (Solondo®, 5 mg tablets, Yuhan Corp., Seoul, Korea) administered orally for 5 days and then tapered for 5 days (a half-dose on days 6 and 7, 20 mg on days 8 and 9, and 10 mg on day 10). Patients were divided into 3 groups: the steroid-only control group consisted of 44 patients who presented between January 2006 and May 2007 and received no additional treatment, the carbogen group consisted of 106 patients who presented between June 2007 and June 2009 and received additional carbogen inhalation treatment, and the lipo-PGE1 group consisted of 52 patients who presented between July 2009 and June 2010 and received additional lipo-PGE1 treatment.
Carbogen inhalation treatment involved inhaling mixed gas (5% CO2, 95% O2) once a day for 1 hour for 5 days. Lipo-PGE1 treatment involved daily intravenous injection of 5 µg lipo-PGE1 mixed with 500 mL normal saline for 5 days.
The follow-up hearing testing schedule is given in Fig. 1. The Therapeutic effects were evaluated at least 2 months after end of treatment which known for hearing stabilazation,13 using the pure tone average (average of the 0.5, 1.0, 2.0, and 3.0 kHz hearing thresholds). We used Siegel's criteria for hearing improvement analysis (Table 1). 'Overall recovery' was defined as showing any recovery after the conclusion of treatment (Siegel's criteria I, II, and III). 'Favorable recovery' was defined as final hearing corresponding to Siegel's criteria I and II. We compared the hearing recovery rate and the degree of hearing recovery between groups. We compared the average relative hearing gain (RHG; hearing difference between pre- and post- pure tone threshold) between the 3 groups.
Given that serviceable hearing is important in patients with SHL, we also segmentally repeated same analysis limited to patients with more than moderate-severe initial hearing loss (initial hearing level over 56 dB). RHG was compared between 3 groups in patients who had more than moderate-severe initial hearing loss and RHG was also analyzed according to frequencies in same patients.
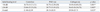
202 out of 236 patients with SHL were included in this study and were consisted of 110 men (54.5%) and 92 women (45.5%). Their mean age was 49.6±16.9 years (range, 13 to 89). The average time between symptom onset and presentation to clinic was 3.5±3.1 days. There were no significant differences in age, gender, disease duration, follow-up period, or initial hearing threshold of the affected ear between groups (Table 2).
Overall average hearing thresholds before and after treatment were 73.2±27.6 dB and 47.1±31.7 dB, respectively. Overall recovery was achieved by 123 patients (60.9%), 88 (43.6%) of whom achieved favorable recovery, which corresponds to Siegel's criteria I and II.
Comparing the recovery rate by the criteria of overall recovery, 72 of 106 (67.9%) in the carbogen group, 28 of 52 (53.8%) in the lipo-PGE1 group, and 23 of 44 (52.3%) in the control group attained hearing recovery. The higher rate of overall recovery in the carbogen group was not statistically significant (p=0.097). However, when comparing favorable recovery, the carbogen group (53.8%) experienced a significantly higher recovery rate than did the lipo-PGE1 group (26.9%) or the control group (38.6%) (p=0.005) (Fig. 2).
In regards to RHG, the carbogen group had higher RHG (29.58 dB) than did the lipo-PGE1 group (20.15 dB) or the control group (21.48 dB), but the difference was not statistically significant (p=0.033) (Table 3).
Word recognition score improved in correlation with average pure tone threshold and there was no statistical difference (p=0.291) (data not shown).
We examined the treatment efficacy in patients with initial hearing level over 56 dB (n=132). In this subset, the carbogen group (n=73) had significantly higher rates of overall and favorable recovery (p=0.008 and p=0.001, respectively) (Fig. 3). In addition, the carbogen group had significantly higher RHG than the other groups (p=0.002) (Table 3). However, when RHG was categorized into frequencies, there was no significant difference between groups except 2.0 kHz (Fig. 4).
If limited to patients with profound hearing loss (n=55), the carbogen group (n=30) tended to have better treatment effect compared to control group (n=15) or lipo-PGE1 group (n=10), but there was no statistical difference between groups in overall and favorable recovery (p=0.712 and p=0.756, respectively) (data not shown).
There were no major complications during treatment. Although several patients experienced severe hyperglycemia, the patients' blood glucose level were normalized after the end of treatment. The incidence of hyperglycemia was not significantly different between groups (data not shown) and it was likely due to the side effect of the systemic corticosteroids.
Although the underlying mechanism of SHL is unknown, the most common causes are thought to be viral infection and vascular disorders of the inner ear.4 Antivirals have been proposed to treat SHL caused by a viral infection, although Stokroos, et al.9 found no significant difference in recovery between patients receiving acyclovir (68% of 22 patients) and those in the control group (43% of 21 patients). Furthermore, Westerlaken, et al.14 reported that antiviral treatment had no effect on hearing gain.
As treatments for SHL, carbogen inhalation and lipo-PGE1 aim to improve circulation in vascular disorders of the inner ear. PGE1 is a prostanoid that improves circulation by blocking receptor-mediated platelet coagulation, and it exhibits biological activities such as cell protection and vasodilation.15 PGE1 is rapidly metabolized in the lung, requiring high dosages that can cause systemic side effects such as arrhythmias, venous thrombosis, and thrombophlebitis.16 To minimize these complications by preventing its rapid metabolism in the lung, PGE1 molecules are surrounded by 0.2-Ag lipid microspheres derived from beans to yield lipo-PGE1, reported to have similar efficacy but higher potency.17
Carbogen inhalation therapy (inhalation of a mixture of 5% CO2 and 95% O2) is based on the theory that carbon dioxide causes vasodilation, increasing blood flow and oxygen to the injured hair cells of cochlear and inner ear structures. According to a study on therapeutic gas proportions, arterial CO2 tension affects oxygen saturation more than does arterial O2 tension. The authors reported that inhalation of 100% O2 gas decreased perilymphic oxygen saturation, while inhalation of a mixture of 95% O2 with 5% CO2 increased perilymphic oxygen saturation.18 Likewise, Fisch, et al.19 reported that carbogen inhalation increases inner ear oxygen saturation as measured by perilymphic oxygen saturation. Furthermore, Kallinen, et al.20 reported that carbogen inhalation is an effective treatment for high frequency hearing loss, although there was no significant difference in RHG in frequencies between patients receiving carbogen and those receiving lipo-PGE1 in this study.
In this study, carbogen inhalation had advantages over lipo-PGE1 and steroids alone particularly in patients with an initial hearing level over 56 dB. This benefit may be due to the vasodilatory effects of CO2 along with the increased oxygen partial pressure in the inner ear. Paradoxically, although PGE1 and lipo-PGE1 are reported to improve cochlear blood flow, they simultaneously decrease systemic blood flow.21 These may explain the reasons for the failure of increase in inner ear oxygen partial pressure.
In conclusion, SHL has a variety of causes and is currently treated with combination modalities. Our findings suggest that efficacy of carbogen inhalation treatment is positive and it can be a reasonable addition to oral corticosteroids to target the vascular component.
Figures and Tables
 | Fig. 1Diagram for treatment and follow-up schedule. After a 10 day-course of corticosteroids and additional treatments, pure tone audiograms were measured. The final hearing test was performed at least 2 months after end of treatment. OPD, outpatient department. |
 | Fig. 2Final hearing results after treatment according to Siegel's criteria. The 'overall' recovery rate (Sigel's type I, II, and III) of the carbogen group (72 of 106, 67.9%) was higher than that of the lipo-PGE1 group (28 of 52, 53.8%) and the control group (23 of 44, 52.3%), although the difference was not statistically significant (p=0.097). The 'favorable' recovery (Sigel's type I and II) rate of the carbogen group (57 of 106, 53.8%) was significantly higher than that of the lipo-PGE1 group (14 of 52, 26.9%) and the control group (17 of 44, 38.6%) (p=0.005). The chi-square test was used. lipo-PGE1, lipo-prostaglandin E1. |
 | Fig. 3Final hearing results after treatment according to Siegel's criteria in patients with ≥56 dB initial hearing. The 'overall' recovery (Sigel's type I, II, and III) rate of the carbogen group (52 of 73, 71.2%) was significantly higher than that of the lipo-PGE1 group (11 of 22, 50.0%) and the control group (14 of 33, 42.5%) (p=0.011). In addition, the 'favorable' recovery (Sigel's type I and II) rate of the carbogen group (37 of 73, 50.7%) was significantly higher than that of the lipo-PGE1 group (4 of 22, 18.1%) and the control group (8 of 33, 24.3%) (p=0.004). The chi-square test and Fischer's exact test were used. lipo-PGE1, lipo-prostaglandin E1. |
 | Fig. 4Degree of hearing recovery (dB) according to frequencies in patients whose hearing was worse than 56 dB. There were no statistically significant differences in any frequency between groups except 2.0 kHz (*p=0.004). One-way ANOVA with post-Hoc test was used. lipo-PGE1, lipo-prostaglandin E1. |
References
1. Arts HA. Flint PW, editor. Sensorineural hearing loss in adults. Cummings Otolaryngology: head & neck surgery. 2010. 5th ed. Philadelphia: Mosby;2117–2130.

2. De Kleyn A. Sudden complete or partial loss of function of the octarus system in apparently normal person. Acta Otolaryngol. 1944. 32:407–429.
3. Park MS. Rha KS, editor. Sudden sensorineural hearing loss. Otorhinolaryngology-Head and Neck Surgery. 2009. 2nd ed. Seoul, Korea: Ilchokak;781–788.
4. Lazarini PR, Camargo AC. Idiopathic sudden sensorineural hearing loss: etiopathogenic aspects. Braz J Otorhinolaryngol. 2006. 72:554–561.

5. Wilson WR, Byl FM, Laird N. The efficacy of steroids in the treatment of idiopathic sudden hearing loss. A double-blind clinical study. Arch Otolaryngol. 1980. 106:772–776.

6. Cinamon U, Bendet E, Kronenberg J. Steroids, carbogen or placebo for sudden hearing loss: a prospective double-blind study. Eur Arch Otorhinolaryngol. 2001. 258:477–480.

7. Kanzaki J, Taiji H, Ogawa K. Evaluation of hearing recovery and efficacy of steroid treatment in sudden deafness. Acta Otolaryngol Suppl. 1988. 456:31–36.

8. Moon IS, Lee JD, Kim J, Hong SJ, Lee WS. Intratympanic dexamethasone is an effective method as a salvage treatment in refractory sudden hearing loss. Otol Neurotol. 2011. 32:1432–1436.

9. Stokroos RJ, Albers FW, Tenvergert EM. Antiviral treatment of idiopathic sudden sensorineural hearing loss: a prospective, randomized, double-blind clinical trial. Acta Otolaryngol. 1998. 118:488–495.

11. Zhuo XL, Wang Y, Zhuo WL, Zhang XY. Is the application of prostaglandin E1 effective for the treatment of sudden hearing loss? An evidence-based meta-analysis. J Int Med Res. 2008. 36:467–470.

12. Ahn JH, Kim MR, Kim HC. Therapeutic effect of lipoprostaglandin E1 on sudden hearing loss. Am J Otolaryngol. 2005. 26:245–248.

13. Moon IS, Kim J, Lee SY, Choi HS, Lee WS. How long should the sudden hearing loss patients be followed after early steroid combination therapy? Eur Arch Otorhinolaryngol. 2009. 266:1391–1395.

14. Westerlaken BO, Stokroos RJ, Dhooge IJ, Wit HP, Albers FW. Treatment of idiopathic sudden sensorineural hearing loss with antiviral therapy: a prospective, randomized, double-blind clinical trial. Ann Otol Rhinol Laryngol. 2003. 112:993–1000.

15. Karetova D, Bultas J, Vondracek V, Aschermann M. Alprostadil: modes of actions in peripheral arterial occlusive disease. Am J Ther. 1997. 4:359–363.
16. Ferreira SH, Vane JR. Prostaglandins: their disappearance from and release into the circulation. Nature. 1967. 216:868–873.

17. Hoshi K, Mizushima Y, Kiyokawa S, Yanagawa A. Prostaglandin E1 incorporated in lipid microspheres in the treatment of peripheral vascular diseases and diabetic neuropathy. Drugs Exp Clin Res. 1986. 12:681–685.
18. Kallinen J, Didier A, Miller JM, Nuttall A, Grénman R. The effect of CO2- and O2-gas mixtures on laser Doppler measured cochlear and skin blood flow in guinea pigs. Hear Res. 1991. 55:255–262.

19. Fisch U, Murata K, Hossli G. Measurement of oxygen tension in human perilymph. Acta Otolaryngol. 1976. 81:278–282.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download