Abstract
Purpose
Recent studies suggest new mechanisms of Botulinum toxin (BoNT) other than inhibiting acetylcholine (ACh) release from nerve terminals. The aim of this study was to determine whether other mechanisms for BoNT exist, so that it directly inhibits smooth muscle contraction.
Materials and Methods
Guinea pig antral muscle strips were studied in vitro after 2 hours of exposure to Botulinum toxin type A (BoNT/A). Contractile responses to electric field stimulation (EFS), high K+ (60 mM) and ACh (100 µM) were evaluated 24 and 48 hours after antral intramuscular injection of BoNT/A or vehicle.
Botulinum toxin (BoNT) is the most powerful inhibitor of muscular contraction. It is produced by the bacterium Clostridium botulinum, and seven serologically different subtypes (A though G) exist in nature.1 One subtype is Botulinum toxin type A (BoNT/A), which has potent neuromuscular blocking action with fewer limitations2 and is used as a therapeutic agent to treat spastic disorders including strabismus, hemifacial spasm, achalasia and skin wrinkles.3
BoNT/A consists of a heavy chain of 100 kDa and a light chain of 50 kDa. The heavy chain mediates its cellular adherence and cytoplasmic entry of the light chain,4 whereas the light chain catalyzes the cleavage of a 25 kDa synaptosomal associated protein (SNAP-25; a protein that mediates synaptic vesicle membrane docking and fusion) at the neuromuscular junction, thereby preventing neurotransmitter release and inducing paralysis.1 Typically, BoNT/A causes reversible denervation atrophy. Its clinical effect starts 24 to 72 hours after administration of toxin and lasts for 2-6 months.2
Recently, SNAP-25, a substrate for BoNT/A, was found in the smooth muscle of feline esophagus5 and it inhibited potassium currents in functional studies of circular smooth muscle cells.6 This suggests a role for SNAP-25 in regulating muscle contractility and the possibility of a novel mechanism for BoNT. Actually, this novel mechanism was previously suggested in an in vitro study.7 A higher concentration of BoNT/A (10 U/mL) directly inhibited smooth muscle contractility, whereas at a lower concentration (2 U/mL) it inhibited acetylcholine (Ach) release from cholinergic nerves without affecting Ach-induced contractions. In that study, however, muscle strips were studied after 6 hours of exposure to high dose BoNT, instead of using a clinically important method, direct injection. Also, only short-term effects of BoNT were evaluated.
Therefore, the aims of our present study were 1) to determine whether other mechanisms for BoNT exist, especially direct inhibition of smooth muscle contractions and 2) to evaluate changes in the effects of BoNT on muscular contractility over time.
Guinea pigs, weighing 300-350 g, were used for the study. Guinea pigs were killed by anesthesia using intraperitoneal injection of pentobarbital sodium 35-40 mg/kg and decapitation. The stomachs were removed, opened along the longitudinal axis, and rinsed with Krebs-Hanseleite buffer (in mM: 120 NaCl, 4.6 KCl, 2.5 CaCl2, 1.2 MgCl2, 22 NaHCO3, 1.2 NaH2PO4, and 11.5 glucose, oxygenated with 95% O2-5% CO2, pH 7.4). The mucosa was removed from the antrum. Antral circular muscle strips were prepared and suspended in 5 mL organ baths. Muscle tension was measured along the circular muscle direction using an isometric force transducer (BIOPAC TSD 105; BIOPAC system, Inc., Santa Barbara, CA, USA). Muscle strips were suspended between platinum electrodes placed adjacent and parallel to the long axis of the muscle strip. Electrodes were connected to an electric stimulator (model S88K, Grass Instruments, Quincy, MA, USA). After 2 hours of equilibration period, contractile force was measured. The experimental procedures were conducted in accordance with the guidelines of the University of Yonsei Animal Care and Use Committee.
Guinea pigs were anesthetized with intraperitoneal injections of pentobarbital (35-40 mg/kg). A short abdominal incision was made, and the antrum of the stomach was isolated. Guinea pigs were injected with BoNT/A using a 27G needle. A total of 4 & 10 U of BoNT/A were diluted in 1 mL of saline and injected subserosally into the four cardinal points of the antrum: on the small and large curve, and on the posterior and anterior wall (1 & 2.5 U in each 0.25 mL injection, BoNT/A group). The control animals were anesthetized and laparotomized, but injected with saline. At 24 and 48 hours after injection of BoNT/A, antral muscle strips from control guinea pigs were prepared by exactly the same way as described previously.
Muscle strips were studied in vitro for their contractile responses to electrical field stimulation (EFS), high K+ (60 mM) and ACh (100 µM). First, BoNT/A was added in concentrations of 2, 4, or 10 U. EFS (4 Hz, 60 s) was done every 30 min for 6 hours in the continued presence of BoNT in order to find the most effective concentration of BoNT/A for the inhibition of muscle contraction. Second, after induction of muscle contraction by high K+, 10 U of BoNT/A was added to determine whether BoNT/A directly inhibits muscular contractility. Third, EFS at 1, 4, 8, or 20 Hz, 100 V, 0.5-ms pulse width duration (square wave), and 60 s train duration was done (1 and 4 Hz for activation of the intrinsic nerves; 8 and 20 Hz for the direct stimulation of muscle contraction). N-nitro-L-arginine methyl ester (L-NAME; 100 µM) was added to inhibit nitric oxide (NO)-mediated relaxation. After measuring initial control responses to EFS and ACh 100 µM, the same experiment was repeated with the addition of BoNT/A (10 U). Fourth, contractile responses to EFS were measured with antral muscle strips excised 24 and 48 hours after antral intramuscular injection of BoNT/A.
Antral muscle strips around the BoNT/A injection site were removed and immersed in 10% formalin for 6 hours. After fixation, tissues were embedded in paraffin, and 5 µm sections were stained with hematoxylin and eosin. Pathologic changes in the injected area were compared with those of controls under light microscopy.
BoNT/A reduced EFS-induced contractions in a concentration-dependent fashion. In normal Krebs solution, EFS (4 Hz, 60 s) induced contractions of muscle strips (0.64±0.18 kg/cm2) (n=7). Addition of 2, 4, or 10 U of BoNT/A decreased EFS-induced contractile responses to 0.52±0.14, 0.43±0.12 and 0.34±0.15 kg/cm2 (n=7, p<0.05), respectively (Fig. 1). Ten U of BoNT/A was the most effective dose for the inhibition of muscle contraction.
BoNT/A had an inhibitory effect on muscular contractility induced by high K+. High K+ depolarizes the smooth muscle cell membrane and opens voltage-dependent calcium channels, which results in an influx of extracellular calcium and an activation of contractile machinery.8,9 In this study, high K+ (60 mM) induced a considerable muscle contraction (2.65±0.75 kg/cm2) (n=4), and this contractile response was substantially reduced (-47%) by BoNT/A (10 U) to 1.39±0.37 kg/cm2 (n=4, p<0.05) (Fig. 2).
BoNT/A decreased EFS-induced muscle contractions (1 and 4 Hz for the activation of intrinsic nerves; 8 and 20 Hz for the direct stimulation of muscle contraction). The addition of L-NAME (100 µM) increased contractile responses to EFS (n=4, p>0.05). When both L-NAME (100 µM) and BoNT/A (10 U) were applied to the muscle strips, there was no significant change in EFS-induced muscle contractions (EFS at 1, 4, 8, or 20 Hz) (n=4, p>0.05) (Fig. 3).
BoNT/A caused a significant decrease in muscular contractions in response to ACh. The addition of L-NAME (100 µM) increased contractile responses to Ach (100 µM) (n=4, p>0.05). However, when both L-NAME (100 µM) and BoNT/A (10 U) were applied to muscular strips, there was a significant decrease in muscle contraction in response to ACh (n=4, p<0.05) (Fig. 4).
At 24 hours after antral intramuscular injection of BoNT/A (4 & 10 U), there was a significant decrease in muscular contraction in response to EFS (1, 4, 8, or 20 Hz, respectively; n=4, p<0.05). However, no significant difference was found between EFS-induced contractile responses in the presence of BoNT/A (4 and 10 U; n=4, p>0.05).
At 48 hours after the injection of BoNT/A, overall contractile responses to EFS were slightly enhanced compared to 24 hours. Muscular contractions in response to EFS were significantly decreased (at 1, 4, 8, or 20 Hz, respectively; n=4, p<0.05). However, no significant difference existed between contractile responses to EFS in the presence of BoNT/A (4 or 10 U; n=4, p>0.05) (Fig. 5).
There were no pathologic changes in the muscular strips taken 24 and 48 hours after the injection of BoNT/A 4 U. However, in case of injection with BoNT/A 10 U, intramuscular hemorrhage and infiltration of inflammatory cells were detected (Fig. 6).
In this study, we tried to acquire evidence of direct inhibition of muscular contraction by BoNT. At BoNT/A concentrations of 4 & 10 U, contractile responses of smooth muscle strips to low (1 & 4 Hz) and high (8 & 20 Hz) frequency EFS were significantly inhibited, and these effects lasted for at least 48 hours. Also, BoNT/A inhibited muscular contractions caused by high K+ and ACh. Considering that high K+ depolarizes the smooth muscle cell membrane and activates muscle contractions, these results suggest a possibility of a novel mechanism for BoNT/A-direct inhibition of muscle contraction.
NO is involved in both short-lasting and sustained non adrenergic non cholinergic relaxation.10 In the present study, pretreatment with L-NAME inhibited NO-mediated relaxation and considerably increased contractile response to EFS and ACh. Furthermore, addition of BoNT/A and L-NAME notably decreased muscle contractions in response to ACh. In contrast, the inhibition of contractile responses to EFS when induced by BoNT/A and L-NAME was not significant. It is, therefore, possible that muscle strips might be in poor condition after 2 hours' incubation, or muscle contraction to low & high frequency EFS may not be strong enough to show a profound BoNT/A-induced decrease in muscle tone when compared with the contractile response to ACh and High K+.
The classical mechanism for BoNT is to inhibit ACh release from cholinergic nerves. Recently, several studies have suggested the possibility of other mechanisms of action of BoNT. In addition to be a local muscle relaxant, BoNT appears to act at the level of central nervous system.11,12 BoNT can also alleviate pain by interacting with several other neuronal signaling pathways such as those triggered by substance P, glutamate, and calcitonin gene related peptide.13,14 BoNT/A selectively degrades SNAP-25, a protein required for vesicle fusion, thereby preventing neurosecretory vesicles from fusing with the nerve membrane.15 Interestingly, SNAP-25 also exists in esophageal smooth muscle and inhibits outward potassium currents. Therefore, if SNAP-25 is cleaved by BoNT/A, esophageal smooth muscle tone would be decreased by hyperpolarization of the membrane.6 This might be the mechanism for direct inhibition of muscle contraction by BoNT/A. However, whether SNAP-25 exists in stomach smooth muscle cell of guinea pig, or whether BoNT/A can enter smooth muscle cells is not yet certain. These points need to be verified in future studies.
Nowadays, BoNT/A is used therapeutically for a variety of spastic disorders of gastrointestinal smooth muscle. Injection of BoNT into the lower esophageal sphincter has been shown to reduce the symptoms of achalasia (dysphasia, regurgitation, and chest pain), decrease lower esophageal sphincter pressure, and improve esophageal emptying, compared with the injection of placebo.16,17 BoNT injection into the internal or external anal sphincter causes relaxation of the anal sphincters, enhances microcirculation at the fissure site, and promotes fissure healing.18,19 Most of these studies evaluated results by symptom control and improvements in manometric findings, whereas few studies have directly investigated changes in muscle tone and mechanism of action over time. Typically, a 24 to 72 hour delay exists between the administration of toxin and the onset of clinical effects.2 Even though the delay in onset of clinical effects is not fully understood, the delay could be related to either a delayed or protracted effect of the protease on substrate metabolism, or to proximal spread of the toxin to the central nervous system.20 However, in this study, the onset of effects occurred at least 24 hours after the injection of BoNT/A. Furthermore, it took BoNT/A only 2 hours to induce relaxation of muscle strips. Therefore, BoNT/A might have a different mechanism of action to relieve symptoms caused by various diseases, instead of simple relaxation of muscle. Also, the onset of BoNT/A effects might depend on the amount of BoNT/A: a relatively large amount of BoNT/A could have a fast direct effect on muscle and nerve, while small amounts might take a longer time for diffusion and can not induce direct inhibition of muscular contractility.
Interestingly, muscle strips taken 24 & 48 hour after the injection of BoNT/A were not responsive to high frequency EFS. These results indicate that BoNT/A directly inhibits muscular contractility, and it is possible that other factors affected muscle tone after surgery. For example, post operative ileus of the stomach could be responsible for decreased contractile responses to EFS. However, given that controls also underwent post operative ileus after surgery, the considerably decreased contractile response to high frequency EFS may be caused by BoNT/A. In addition, inflammatory responses including physical damage could have an influence on the contractility of antral muscle strips. Actually in the present study, hemorrhage and inflammatory responses were noted in the muscle strips taken 24 & 48 hours after antral intramuscular injection of 10 U of BoNT/A. Even though muscle strips receiving 4 U of BoNT/A did not have any sign of inflammation or hemorrhage, contractile responses of these strips to EFS were very similar to the responses of muscle strips receiving 10 U of BoNT/A. Therefore, inflammation or physical damage itself does not seem to be the cause of decreased contractile responses to EFS.
In the beginning of this study, we planned to evaluate muscle tone one week after the injection of BoNT/A. However, once guinea pigs underwent surgery and injection, they could not eat enough food and most of them died within one week. Similar outcomes were observed with a lower concentration of BoNT/A. Because 4 U of BoNT/A did not cause any inflammation or hemorrhage around the injection site, physical or chemical damage might not be the direct cause of the deaths of the guinea pigs. One possible explanation is the inhibition of antral motility by BoNT/A: BoNT/A injected into the gastric wall of rats could reduce body weight and food intake through the inhibition of antral motility.21 The other explanation involves systemic toxicity of BoNT. The exact lethal dose for the injection of BoNT is not yet known. In the case of intramuscular injection in monkeys, the fatal dose range of BoNT/A was 38-42 U/kg.22 Considering the body weight of a guinea pig, 10 U of BoNT/A could be enough to cause death.
In summary, BoNT/A can directly inhibit antral muscular contractility, in addition to blocking the release of ACh from nerves, and this effect lasts at least 48 hours after antral intramuscular injection of BoNT/A. These results provide an evidence for a new mechanism of BoNT-direct inhibition of muscular contraction.
Figures and Tables
Fig. 1
Effect of various concentrations of BoNT/A on muscular contractions to EFS. BoNT/A reduced the EFS-induced contraction in a concentration-dependent fashion. (A) Tension recordings from guinea pig antral muscle strips showing progressive loss of contractile force with increasing concentration of BoNT/A. (B) Contractions of muscle strips to EFS were inhibited most effectively by 10U/m of BoNT/A. EFS, electric field stimulation.

Fig. 2
Effect of BoNT/A on muscle contractions to high K+. BoNT/A 10 U significantly inhibited contractile response induced by High K+ (60 mM).

Fig. 3
Effect of L-NAME and BoNT/A on muscle contractions induced by EFS. The addition of L-NAME (100 µM) increased contractile responses to EFS (p>0.05). When L-NAME (100 µM) and BoNT/A (10 U) were both applied to the muscle strips, there was a slight decrease of in EFS-induced muscle contractions (EFS at 1, 4, 8, or 20 Hz; p>0.05). L-NAME, N-nitro-L-arginine methyl ester; EFS, electrical field stimulation.
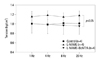
Fig. 4
Effect of L-NAME and BoNT/A on muscular contractions to ACh. The addition of L-NAME (100 µM) increased (p>0.05) contractile responses to Ach (100 µM). However, when L-NAME (100 µM) and BoNT/A (10 U) were both applied to muscular strips, there was a significant decrease in muscle contraction in response to ACh (p<0.05). L-NAME, N-nitro-L-arginine methyl ester; ACh, acetylcholine.

Fig. 5
Contractile responses to EFS of antral muscle strips excised 24 and 48 hours after injection of BoNT/A. (A) At 24 hours after intragastric injection of BoNT/A (4 & 10 U), there was a significant decrease in muscular contraction in response to EFS (1, 4, 8, or 20 Hz; p<0.05). However, no significant difference was found between EFS-induced contractile responses in the presence of BoNT/A (4 and 10 U; p>0.05). (B) At 48 hours after injection of BoNT/A, overall contractile responses to EFS were slightly enhanced compared to 24 hours. Muscular contractions in response to EFS were significantly decreased (p<0.05). No significant difference existed between contractile responses to EFS in the presence of BoNT/A (4 or 10 U; p>0.05). EFS, electric field stimulation.

Fig. 6
Pathologic changes in antral muscle strips taken 24 and 48 hours after intragastric injection of 10 U BoNT/A. Intramuscular hemorrhage and infiltration of inflammatory cells were detected in the muscle strips taken 24 (A) and 48 (B) hours after injection of BoNT/A (H&E stain, A: ×400, B: ×100).

References
1. Schiavo G, Matteoli M, Montecucco C. Neurotoxins affecting neuroexocytosis. Physiol Rev. 2000. 80:717–766.

2. Brin MF. Botulinum toxin: chemistry, pharmacology, toxicity, and immunology. Muscle Nerve Suppl. 1997. 6:S146–S168.

4. Lalli G, Herreros J, Osborne SL, Montecucco C, Rossetto O, Schiavo G. Functional characterisation of tetanus and botulinum neurotoxins binding domains. J Cell Sci. 1999. 112(Pt 16):2715–2724.

5. Ji J, Lau H, Sheu L, Diamant NE, Gaisano HY. Distinct regional expression of SNARE proteins in the feline oesophagus. Neurogastroenterol Motil. 2002. 14:383–394.

6. Ji J, Salapatek AM, Lau H, Wang G, Gaisano HY, Diamant NE. SNAP-25, a SNARE protein, inhibits two types of K channels in esophageal smooth muscle. Gastroenterology. 2002. 122:994–1006.

7. James AN, Ryan JP, Parkman HP. Inhibitory effects of botulinum toxin on pyloric and antral smooth muscle. Am J Physiol Gastrointest Liver Physiol. 2003. 285:G291–G297.
8. Karaki H, Urakawa N, Kutsky P. Potassium-induced contraction in smooth muscle. Nihon Heikatsukin Gakkai Zasshi. 1984. 20:427–444.

9. Shaari CM, Sanders I. Quantifying how location and dose of botulinum toxin injections affect muscle paralysis. Muscle Nerve. 1993. 16:964–969.

10. Lefebvre RA, Baert E, Barbier AJ. Influence of NG-nitro-L-arginine on non-adrenergic non-cholinergic relaxation in the guinea-pig gastric fundus. Br J Pharmacol. 1992. 106:173–179.

11. Giladi N. The mechanism of action of botulinum toxin type A in focal dystonia is most probably through its dual effect on efferent (motor) and afferent pathways at the injected site. J Neurol Sci. 1997. 152:132–135.

12. Erdal J, Ostergaard L, Fuglsang-Frederiksen A, Werdelin L, Dalager T, Sjö O, et al. Long-term botulinum toxin treatment of cervical dystonia--EMG changes in injected and noninjected muscles. Clin Neurophysiol. 1999. 110:1650–1654.

13. Mense S. Neurobiological basis for the use of botulinum toxin in pain therapy. J Neurol. 2004. 251:Suppl 1. I1–I7.

15. Blasi J, Chapman ER, Link E, Binz T, Yamasaki S, De Camilli P, et al. Botulinum neurotoxin A selectively cleaves the synaptic protein SNAP-25. Nature. 1993. 365:160–163.

17. Annese V, Basciani M, Perri F, Lombardi G, Frusciante V, Simone P, et al. Controlled trial of botulinum toxin injection versus placebo and pneumatic dilation in achalasia. Gastroenterology. 1996. 111:1418–1424.

19. Fernández López F, Conde Freire R, Rios Rios A, García Iglesias J, Caínzos Fernández M, Potel Lesquereux J. Botulinum toxin for the treatment of anal fissure. Dig Surg. 1999. 16:515–518.

20. Wiegand H, Erdmann G, Wellhöner HH. 125I-labelled botulinum A neurotoxin: pharmacokinetics in cats after intramuscular injection. Naunyn Schmiedebergs Arch Pharmacol. 1976. 292:161–165.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download