Abstract
Purpose
Laparoscopy-assisted distal gastrectomy (LADG) is a widely accepted surgery for early gastric cancer. However, its use in advanced gastric cancer has rarely been studied. The aim of this study is to investigate the feasibility and survival outcomes of LADG for pT2 gastric cancer.
Materials and Methods
Between January 2004 and December 2009, we evaluated 67 and 52 patients who underwent open distal gastrectomy (ODG) and LADG, respectively, with diagnosis of pT2 gastric cancer. The clinicopathological characteristics, postoperative outcomes, and survival were retrospectively compared between the two groups.
Results
There were statistically significant differences in the proximal margin of the clinicopathological parameters. The operation time was significantly longer in LADG than in ODG (207.7 vs. 159.9 minutes). There were 6 (9.0%) and 5 (9.6%) complications in ODG and LADG, respectively. During follow-up periods, tumor recurrence occurred in 7 (10.4%) patients of the ODG and in 4 (7.7%) patients of the LADG group. The 5-year survival rate of ODG and LADG was 88.6% and 91.3% (p=0.613), respectively. In view of lymph node involvement, 5-year survival rates were 96.0% in ODG versus 97.0% in LADG for patients with negative nodal metastasis (p=0.968) and 80.9% in ODG versus 78.7% in LADG for those with positive nodal metastasis (p=0.868).
In spite of improvement of the survival of patients with gastric cancer, it is one of the most common causes of cancer-related death in the world.1,2 The incidence of early gastric cancer in Korea has been increasing because of recent improvements for early diagnosis.3 Since laparoscopy-assisted distal gastrectomy (LADG) for early gastric cancer was first performed in 1991 and first reported in 1994,4 many authors have reported their experiences of minimally invasive surgery of the stomach.5-8 As the experience with laparoscopy-assisted gastrectomy (LAG) for early laparoscopgastric cancer gradually accumulated, it was expected that the next step of treatment modality for advanced gastric cancer would be laparoscopic surgeries. However, few reports related to the efficacy of laparoscopic surgery in the management of advanced gastric cancer have been published.9-12
To date, many surgeons have been concerned with advanced gastric cancer surgery by laparoscopy. However, the most reports about LAG for advanced gastric cancer treatment included more than a pT2 lesion (muscularis propria). From the pathological and clinical viewpoints of the primary tumor stage,13,14 pT2 gastric cancer is considered to be an intermediate-stage carcinoma between early and advanced cancer. The patients with gastric cancer involving muscularis propria have been reported to have better prognoses than those with gastric cancer involving subserosa and serosa.13-15 Therefore, before the analysis of LAG for advanced gastric cancer is performed, study of the effectiveness of LAG should be performed on pT2 gastric cancer, which has a relatively better prognosis compared with T3 and T4 gastric cancers. Thus, we investigated the feasibility and survival outcomes of laparoscopic surgery for pT2 (muscular propria) gastric cancer.
Patients with gastric cancer treated with gastrectomy by a single surgeon between January 2004 and December 2009 were included in the present study. In the early period before 2006, our indication of LADG for gastric cancer was cT1N0M0 according to the 6th edition of the American Joint Committee on Cancer (AJCC) staging criteria.16 During that period, 15 patients who were preoperatively evaluated with cT1 were diagnosed with pT2. After 2006, we extended the indication to cT2N1M0. In this retrospective study, 119 cases with pT2 tumors were consecutively selected from patients with gastric cancer, on whom a radical operation was performed. Lymph node dissection was done to standard D2 or more lymphadenectomy according to 2010 Japanese gastric cancer treatment guidelines (ver. 3).17 Of 119 patients, 67 underwent open distal gastrectomy (ODG) and 52 underwent LADG. Clinicopathologic features, such as age, gender, body mass index, comorbidity diseases, tumor size, histologic type, reconstruction, resection margin, lymph node dissection, metastatic lymph node status, postoperative outcomes, recurrences, and survival, were reviewed. All values were expressed as means±standard deviations (SDs). Postoperative hospital stay and follow-up periods were expressed as median±SDs. Major complication was defined as those for which reoperations were needed or that resulted in postoperative death, and minor complication was defined as those for which conservative care was necessary, delaying hospital discharge.
Follow-up results were obtained from patients' hospital records and telephone calls, and recurrence was determined by endoscopy, computed tomography, positron emission tomography, etc.18 The gastric cancer stage was classified according to the seventh edition of the AJCC staging criteria.19
All laparoscopy-assisted gastrectomies were performed according to the standard procedure guidelines as follows.18 All patients were placed in lithotomy position under general anesthesia. The surgeon stood on the patient's right, with the first assistant on the patient's left and the camera assistant between the patient's legs. An initial 11 mm trocar for a 30 degree rigid laparoscope was inserted through the supraumbilical area using an open technique. After the establishment of a pneumoperitoneum at 12 mm Hg, four surgical ports were inserted. First, the greater omentum was divided at the mid portion of the transverse colon about 4-5 cm from the gastroepiploic arcade toward the lower pole of the spleen using Harmonic ACE (Ethicon Endo-Surgery, Cincinnati, OH, USA). Next, the right omentum and lymph nodes were dissected along the right gastroepiploic vessels (no. 4d). The infrapyloric nodes (no. 6) and the nodes along the superior mesenteric vein (no. 14v, if necessary) were dissected. After the suprapyloric nodes (no. 5) and the nodes along the proper hepatic artery (no. 12a) were dissected, the duodenum just distal to the pyloric ring was transected. Then the nodes along the common hepatic artery (no. 8a) and the proximal splenic artery (no. 11p) were dissected. After dissecting the nodes along the left gastric artery (no.7) and the nodes around the celiac artery (no. 9), the right cardial nodes (no. 1) and the nodes along the lesser curvature (no. 3) were dissected. A 5-cm upper midline or transverse skin incision was made from the substernal angle or right subcostal area, and an incision template (Alexis™ Wound retractor, Applied Medical, Rancho Santa Margarita, CA, USA) was applied on the incision site. Billroth I gastroduodenostomy was performed by a circular stapler (Proximate CDH 29; Ethicon Endo-Surgery, Cincinnati, OH, USA), and Billroth II gastrojejunostomy using flexible laparoscopic stapling devices (Echelon Flex, Ethicon Endo-Surgery, Cincinnati, OH, USA) was performed or a handsewing technique was adopted as used for conventional open surgery.
Chi-square and independent t-tests were used to compare the clinicopathological factors of patients with ODG and LADG using GraphPad InStat® (version 3.06, GraphPad Software, Inc., San Diego, CA, USA). Statistical significance was assumed for p values <0.05. Survival curves were calculated by the Kaplan-Meier method. The log-rank test was used to analyze survival differences, and SPSS version 18.0 (SPSS, Chicago, IL, USA) was used for the analysis.
Clinical and pathological data for the 119 evaluable patients are shown in Table 1. No statistically significant differences were seen between both groups, except in the proximal margin (ODG, 6.5±3.6 versus LADG, 5.0±2.9 cm; p=0.014). The mean number of retrieved lymph nodes in ODG was 39.3±11.2, and it was 39.1±15.2 in LADG. Lymph node metastasis was identified in 32 (47.8%) and 19 patients (36.5%) of ODG and LADG, respectively. According to N stage classification, N0, N1, N2, and N3 with ODG and LADG were 35, 12, 12, and 8, and 33, 9, 9, and 1, respectively.
Operation time was significantly longer in the LADG group than in the ODG group (207.7±40.6 versus 159.9±39.0 minutes, respectively; p<0.0001). First flatus times, postoperative median hospital stay, and postoperative complications had no statistical differences between both groups. There were 6 (9.0%) and 5 (9.6%) operation-related complications in the ODG and LADG groups, respectively. Immediate postoperative intra-abdominal bleeding occurred in one case in the ODG group who needed operative hemostasis. Stump leakage occurred in one case in the LADG group, which was corrected by surgical intervention, and one patient died of postoperative multi-organ failure. As for perioperative blood transfusion, 5 cases of the ODG group required transfusion and 2 of the LADG group did, but no statistical significance was shown between both groups (Table 2).
The median follow-up period for the ODG group was 60.4 months (range, 7.0-91.7 months) and 53.2 months for the LADG group (range, 1.0-82.2 months; p=0.114) (Table 2). Tumor recurrence was detected in 7 cases (10.4%) in the ODG group and in 4 cases (7.7%) in the LADG group during the follow-up periods. Details of patients with distant and local recurrence are shown in Table 3. The 5-year survival rate of the ODG and LADG groups were 88.6% and 91.3% (p=0.613), respectively (Fig. 1). In view of lymph node involvement, the 5-year survival rates for patients with negative nodal metastasis were 96.0% in the ODG group versus 97.0% in the LADG group (p=0.968). For those with positive nodal metastasis, the 5-year survival rates were 80.9% in the ODG group versus 78.7% in the LADG group (p=0.868) (Fig. 2A and B).
Early detection of gastric cancer has increased recently because of improved diagnostic procedures and regular individual checkups.3 Although gastrectomy with lymphadenectomy had been firmly accepted as a standard treatment for every stage of gastric cancer since the 1980s,20,21 laparoscopic surgery for gastric cancer has recently become an alternative treatment option. Many authors have reported their experiences and its advantages, such as good cosmetic effects, improved quality of life, minimal degree of pain, shorter hospital stay, early rehabilitation, and early return to social activity.5-8,22,23
As experience with LAG for early gastric cancer substantially increased, particularly in Korea and Japan, some surgeons are concerned with laparoscopic surgery for advanced gastric cancer. However, the application of laparoscopic surgery to advanced gastric cancer remains questionable because of the technical difficulty of lymphadenectomy, and scant data on the oncologic adequacy of the procedure are available.9-12,18
Most reports about LAG for the treatment of advanced gastric cancer included more than pT2 lesions.8-10 According to the depth of invasion of gastric cancer, it is classified by mucosal, submucosal, muscular, subserosal, and serosal cancer. Advanced gastric cancer confined to the muscularis propria is considered to be an intermediate-stage carcinoma between early and advanced cancer. Although gastric carcinoma invading muscularis propria has been classified as advanced stage, postoperative survival for patients with pT2 gastric cancer has been reported to be better than that for patients with other advanced gastric carcinomas.13,14,24 Therefore, before LAG is performed for advanced gastric cancer, a study of the effectiveness of LAG should be performed on pT2 gastric cancer, which has a relatively better prognosis compared with T3 and T4 gastric cancers. In our study, therefore, we analyzed and compared ODG and LADG. No statistical differences were seen between both groups, except in the proximal margin. The tumor size was bigger in the ODG group because until 2006, we had usually favored laparoscopic surgeries mainly in the early gastric cancer which were generally small in size. In cases of pT2 done laparoscopically, they were EGC like pT2, so their sizes were smaller than those done by the open method. There was a statistically significant difference in the proximal margin between both groups, since it was easier to secure the safety margin in the open group than in LADG in which to obtain adequate operative field was restricted. However, the mean length of proximal margins of the LADG group was 5 cm and considered to be adequate for this safety. There were no significant differences in the number of retrieved lymph nodes between the groups. This suggests that laparoscopy-assisted gastrectomy may retrieve as many lymph nodes as open surgery. In postoperative results, although the operation time of the LADG group was longer than that of the ODG group, the postoperative median hospital stay and the first flatus time of the LADG group were not different from those of the ODG group. Postoperative mortality rates for laparoscopic gastrectomy reported by other authors range between 0% and 3%.5,9,10,25 In our study, one death (1.9%) occurred in the LADG group because of multi-organ failure on postoperative day 28. He was preoperatively in a very complicated state. His underlying diseases were pneumonia, atrial fibrillation, right middle cerebral artery infarction, and hypertension. He underwent LADG (Billroth-I). After the operation, he was taken to the intensive care unit because of his unstable condition. Unfortunately, his cardiac, pulmonary, and renal functions gradually failed. In other reports regarding the postoperative morbidity, results ranged from 2% to 20% for patients who underwent LAG.5-7,9-11 The postoperative morbidity rate was 7.7% (4 patients) in the LADG group and 9.0% (6 patients) in the ODG group. In this study, tumor recurred in 7 patients (10.4%) in the ODG group and in 4 patients (7.7%) in the LADG group. The 5-year survival rate of the patients with pT2 gastric cancer has been reported to be 70%-80%.13,14,26 In our study, 5 year survival rates of 119 pT2 gastric cancer patients between the ODG and LADG groups were 88.6% and 91.3% (p=0.446), respectively. No statistical differences in survival rates were observed between the two groups.
An important point is that lymph node metastasis is one of the most significant prognostic factors for pT2 gastric cancer. Some reports have documented that the N stage is recognized as the most important prognostic factor for patients with pT2 gastric cancer.24,27 Regarding the incidence of lymph node metastasis with pT2 gastric cancer, Kim, et al.28 reported 45.7%, and Abe, et al.29 reported 48.9%. In the present study, it was 47.8% (32 of 67 patients) and 36.5% (19 of 52 patients) for the ODG and LADG groups, respectively. The reason that the incidence of lymph node metastasis in our LADG series was low might be that we performed the LADG in EGC-like pT2 cancers, as mentioned above. Some reports showed good prognosis of pT2 gastric cancer with negative nodal metastasis. Park, et al.26 reported a 95.6% 5 year survival rate, and Abe, et al.29 indicated that the 10 year survival rate was 100% if deaths due to other causes were excluded. In present study, the 5-year survival rate with negative nodal metastasis of pT2 gastric cancer was high in both groups (ODG, 96.0%; LADG, 97.0%; p=0.968). However, the 5-year survival rate with positive nodal metastasis of pT2 gastric cancer was decreased (ODG, 80.9%; LADG, 78.7%; p=0.868). Therefore, it is highly likely that lymph node metastasis influenced the prognosis of pT2 gastric cancer. In view of no differences in the extent of lymph node dissection, number of retrieved lymph nodes, and survival rates (prognosis) between both groups, laparoscopy-assisted gastrectomy for pT2 gastric cancer may be feasible. Moreover, because lymph node metastasis is closely related with the postoperative prognosis in pT2 gastric cancer, it will be mandatory to perform adequate radical lymph node dissection in LADG. However, there was no statistical difference in the length of median follow-up period between both groups, and the follow-up period of LADG group was shorter than that of ODG group, thus leaving the possibility to affect the interpretation of recurrence rate. Therefore, longer period of follow-up for both groups will be needed to analyze the recurrence rate and survival.
The drawbacks of this study include the retrospective design of a small number of cases and the possibility of bias in data. In fact, the number of the patients enrolled in this study was too small to assert eligibility of LADG in terms of oncologic safety. Despite a small retrospective comparison series, we believe that this is an important study in establishing a basis for larger, prospective studies. Therefore, a prospective, randomized, controlled trial with available indications is essential to overcome those drawbacks. Nevertheless, we cautiously propose that LADG would be a feasible alternative for T2 gastric cancer.
In conclusion, the study was designed to assess the feasibility of LADG for pT2 gastric cancer, and its data suggested that LADG might be an acceptable alternative for some of pT2 gastric cancer. Nevertheless, further clinical observations and prospective, controlled studies for advanced gastric cancer will be needed to elucidate the long-term effects of laparoscopy-assisted gastrectomy.
Figures and Tables
Fig. 1
Comparison of 5-year survival rate for pT2 gastric cancer between ODG and LADG. There was no statistically difference between both groups (p=0.446). ODG, open distal gastrectomy; LADG, laparoscopy-assisted distal gastrectomy.
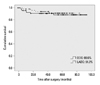
Fig. 2
Comparison of 5-year survival rate for pT2 gastric cancer between ODG and LADG according to lymph node metastasis. The 5 year survival rates of negative nodal metastasis (A) between both groups were 96.0% and 97.0% (p=0.968), and those of positive nodal metastasis (B) were 80.9% and 78.7% (p=0.868), respectively. ODG, open distal gastrectomy; LADG, laparoscopy-assisted distal gastrectomy.

ACKNOWLEDGEMENTS
This work was supported by a grant of the Korea Healthcare technology R&D project, Ministry of Health, Welfare, & Family Affairs, Republic of Korea (1020410).
References
1. Ohtsu A, Yoshida S, Saijo N. Disparities in gastric cancer chemotherapy between the East and West. J Clin Oncol. 2006. 24:2188–2196.

2. Adachi Y, Shiraishi N, Kitano S. Modern treatment of early gastric cancer: review of the Japanese experience. Dig Surg. 2002. 19:333–339.

3. Hyung WJ, Kim SS, Choi WH, Cheong JH, Choi SH, Kim CB, et al. Changes in treatment outcomes of gastric cancer surgery over 45 years at a single institution. Yonsei Med J. 2008. 49:409–415.

4. Kitano S, Iso Y, Moriyama M, Sugimachi K. Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc. 1994. 4:146–148.
5. Kim MC, Kim KH, Kim HH, Jung GJ. Comparison of laparoscopy-assisted by conventional open distal gastrectomy and extraperigastric lymph node dissection in early gastric cancer. J Surg Oncol. 2005. 91:90–94.

6. Kim MC, Kim HH, Jung GJ. Surgical outcome of laparoscopy-assisted gastrectomy with extraperigastric lymph node dissection for gastric cancer. Eur J Surg Oncol. 2005. 31:401–405.

7. Kitano S, Shiraishi N, Kakisako K, Yasuda K, Inomata M, Adachi Y. Laparoscopy-assisted Billroth-I gastrectomy (LADG) for cancer: our 10 years' experience. Surg Laparosc Endosc Percutan Tech. 2002. 12:204–207.

8. Kim KH, Kim MC, Jung GJ, Kim HH. The learning curve in laparoscopy assisted distal gastrectomy (LADG) with systemic lymphadenectomy for early gastric cancer considering the operation time. J Korean Surg Soc. 2006. 70:102–107.
9. Hwang SI, Kim HO, Yoo CH, Shin JH, Son BH. Laparoscopic-assisted distal gastrectomy versus open distal gastrectomy for advanced gastric cancer. Surg Endosc. 2009. 23:1252–1258.

10. Lee J, Kim W. Long-term outcomes after laparoscopy-assisted gastrectomy for advanced gastric cancer: analysis of consecutive 106 experiences. J Surg Oncol. 2009. 100:693–698.

11. Shuang J, Qi S, Zheng J, Zhao Q, Li J, Kang Z, et al. A case-control study of laparoscopy-assisted and open distal gastrectomy for advanced gastric cancer. J Gastrointest Surg. 2011. 15:57–62.

12. Goh PM, Khan AZ, So JB, Lomanto D, Cheah WK, Muthiah R, et al. Early experience with laparoscopic radical gastrectomy for advanced gastric cancer. Surg Laparosc Endosc Percutan Tech. 2001. 11:83–87.

13. Nakamura K, Kamei T, Ohtomo N, Kinukawa N, Tanaka M. Gastric carcinoma confined to the muscularis propria: how can we detect, evaluate, and cure intermediate-stage carcinoma of the stomach? Am J Gastroenterol. 1999. 94:2251–2255.

14. Otsuji E, Kuriu Y, Ichikawa D, Okamoto K, Hagiwara A, Yamagishi H. Characteristics of gastric carcinoma invading the muscularis propria. J Surg Oncol. 2005. 92:104–108.

15. Lu Y, Liu C, Zhang R, Li H, Lu P, Jin F, et al. Prognostic significance of subclassification of pT2 gastric cancer: a retrospective study of 847 patients. Surg Oncol. 2008. 17:317–322.

16. Greene FL, Page DL, Fleming ID, Fritz A, Balch CM, Haller DG, et al. American Joint Committee on Cancer (AJCC) cancer staging manual. 2002. 6th ed. New York, NY: Springer.
17. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011. 14:113–123.
18. Kim KH, Kim MC, Jung GJ, Kim HH. Long-term outcomes and feasibility with laparoscopy-assisted gastrectomy for gastric cancer. J Gastric Cancer. 2012. 12:18–25.

19. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A. AJCC Cancer Staging Manual. 2010. 7th ed. New York: Springer.
20. Maruyama K, Okabayashi K, Kinoshita T. Progress in gastric cancer surgery in Japan and its limits of radicality. World J Surg. 1987. 11:418–425.

21. Sawai K, Takahashi T, Suzuki H. New trends in surgery for gastric cancer in Japan. J Surg Oncol. 1994. 56:221–226.

22. Adachi Y, Suematsu T, Shiraishi N, Katsuta T, Morimoto A, Kitano S, et al. Quality of life after laparoscopy-assisted Billroth I gastrectomy. Ann Surg. 1999. 229:49–54.

23. Kim YW, Baik YH, Yun YH, Nam BH, Kim DH, Choi IJ, et al. Improved quality of life outcomes after laparoscopy-assisted distal gastrectomy for early gastric cancer: results of a prospective randomized clinical trial. Ann Surg. 2008. 248:721–727.

24. Sarela AI, Turnbull AD, Coit DG, Klimstra D, Brennan MF, Karpeh MS. Accurate lymph node staging is of greater prognostic importance than subclassification of the T2 category for gastric adenocarcinoma. Ann Surg Oncol. 2003. 10:783–791.

25. Pugliese R, Maggioni D, Sansonna F, Scandroglio I, Ferrari GC, Di Lernia S, et al. Total and subtotal laparoscopic gastrectomy for adenocarcinoma. Surg Endosc. 2007. 21:21–27.

26. Park do J, Kong SH, Lee HJ, Kim WH, Yang HK, Lee KU, et al. Subclassification of pT2 gastric adenocarcinoma according to depth of invasion (pT2a vs pT2b) and lymph node status (pN). Surgery. 2007. 141:757–763.

27. Isozaki H, Fujii K, Nomura E, Mabuchi H, Nishiguchi K, Hara H, et al. Prognostic factors of advanced gastric carcinoma without serosal invasion (pT2 gastric carcinoma). Hepatogastroenterology. 1999. 46:2669–2672.
28. Kim WS, Park SH, Kim JH. Lymphadenectomy for Stomach Cancer in T2 Stage. J Korean Surg Soc. 2002. 63:468–472.
29. Abe S, Yoshimura H, Nagaoka S, Monden N, Kinugasa S, Nagasue N, et al. Long-term results of operation for carcinoma of the stomach in T1/T2 stages: critical evaluation of the concept of early carcinoma of the stomach. J Am Coll Surg. 1995. 181:389–396.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download