Abstract
Purpose
To evaluate meniscofibular ligament (MFibL) at the posterolateral corner of the knee joint on the magnetic resonance arthrography (MRA) with 70° knee flexion.
Materials and Methods
The MRA of the knee joint was performed at 70° knee flexion. Eighteen patients (19 knee joints) underwent scanning of sagittal, coronal, and axial fat-suppressed T1 weighted images (T1FS), and coronal fat-suppressed T2 weighted images. Sagittal three-dimensional (3D) gradient echo (GRE) images were also obtained. Retrospective review of 19 knee MRA studies was independently performed by two musculoskeletal radiologists. The statistical significance was proved by chi-square test.
Results
The MFibL ligament was optimally demonstrated on the far lateral sagittal 3D GRE and T1FS MRA images. The MFibL appeared as a curvilinear or straight hypointense band of variable thickness, extended from the posterolateral meniscus to upper anteromedial aspect of the fibular head. The MFibL was demonstrated with scale 2 (more than a half length of the ligament) by both reviewers in 73.68% (n=14/19) of the knee 3D GRE images and 89.47% (n=17/19) of the knee T1FS images. The visualization on T1FS and that on GRE were not statistically different from each other (p>0.05). The interobserver agreements were significantly good on both 3D GRE and T1FS images in detecting the ligament (kappa values, 0.642 and 0.683, respectively).
The meniscofibular ligament (MFibL) is a structure relevant to the stability of the posterolateral corner of the knee joint1 which runs between the apex of the fibular head and the posterior third of the lateral meniscus, being located anterior to the popliteus tendon.2 The anatomical literature reported that the MFibL is present in 80% of individuals.3 However, a recent anatomic study using dissection microscopy and transillumination methods showed that the MFibL is present in all cadaveric specimens.2 Obaid, et al.4 identified the MFiblL in 16-63% using magnetic resonance imaging (MRI). A wide range of detection rate on MRI depends on whether there is fluid in the posterolateral corner.
Recently, direct magnetic resonance (MR) arthrography (MRA) of the knee has been advocated as a means of assessing postoperative recurrent meniscal tear, osteochondral lesion, detection of loose bodies, and delineation of synovial plicae. The MRA of the knee can provide detailed information about the anatomy of the posterolateral corner.5 We postulated that preoperative evaluation of the anatomical structures of knee joints in identical circumstances as the arthroscopic surgery, in posture and in fluid injection, might help arthroscopists to simulate surgery before actually performing it. Thus, magnetic resonance (MR) arthrography was performed in arthroscopic postures of knee joints over a given time period. All the above all structures were visualized on MR arthrography, and the MFibL appeared to be out of the most dramatically visualized structures. Since the presence of fluid in the posterolateral corner improves visualization of the ligament4 and the MFibL has a posterior displacement in knee flexion,6 the MFibL was evaluated by using MRA at 70° knee flexion in the present study.
We reviewed the MRA of the knee joint in flexion of 18 patients between July 2008 and February 2009. There were 7 male and 11 female patients (a total of 19 knee joints) with an average age of 45.9 years with the range of 19-63 years. Patients with a history of any kind of knee surgery, PCL insufficiency, and posterolateral rotatory instability were excluded. Informed consent was obtained from all patients for MRA analysis. This study was reviewed and approved by the institutional review board.
MRA was performed on a 3-T MR system (Achieva®, Philips Medical Systems, Best, the Netherlands) with SENSE-Flex-M coil, after intra-articular injection of 50 mL of diluted dimeglumine gadopentetate solution (2 mmol/L, Magnevist®, Schering, Berlin, Germany) (mixture with a concentration of 0.2 mL of Magnevist® per 45 mL of normal saline and 5 mL of Iodine contrast) under the fluoroscopic guidance. A 20-gauge 90-mm needle was introduced just lateral to the patellar ligament and was directed upward and slightly medially toward the femoral notch at 70° knee flexion. No complications such as hematoma, allergic reaction, delayed infection, hemarthrosis or synovitis, were encountered.
After an intra-articular contrast medium administration, each patient was examined with the MR unit in 70° knee flexion. The 3-T MRA protocol with the knee at 70° flexion included axial, sagittal, and coronal T1-weighted turbo spin echo (TSE) sequences with fat-suppression (TR/TE=900/20 ms; 3 mm slice thickness and 1 mm interslice gap; field of view 160×160 mm; echo train length 14; and matrix 292×292); coronal T2-weighted TSE sequence with fat-suppression (TR/TE=3500/70 ms; 3 mm slice thickness and 1 mm interslice gap; field of view 160×160 mm; echo train length 14; and matrix 292×292); and sagittal three-dimensional (3D) thrive gradient echo sequence (TR/TE=8.6/3.8 ms and flip angle 6°; slice thickness 0.5 mm for 15 knee joints and 1.5 mm for the other four knee joints; no gap; field of view 140×140 mm; matrix 280×280; and average scan duration 4 minutes 30 seconds).
The radiological assessment for the presence or absence of the MFibL was carried out using sagittal fat suppressed T1 weighted images and sagittal 3D gradient echo images of the knee MRA by two musculoskeletal radiologists who were unaware of the clinical information. The presence of visible MFibL was assessed by the presence of curvilinear or straight, hypointense band of variable thickness extending between the inferior margin of the posterior third of the lateral meniscus and the fibular head (Figs. 1 and 2). The visualization of MFibL was assessed by using the visual confidence scale: 2 for more than a half length of the ligament, 1 for less than a half length, and 0 for no visibility.
All images of the knee MRA were reviewed separately by two musculoskeletal radiologists, and the interobserver agreement of the visual confidence scale was calculated. The radiological assessment by consensus for the presence or absence of the MFibL was carried out, and the MFibL visualization was recorded. The presence was defined if both reviewers read the ligament as the scale 1 or 2.
The kappa statistics was used to determine the interobserver agreement between the two reviewers. We calculated unweighted kappa values for disagreement for each sequence. The visualization of MFibL on fat suppressed T1 weighted images (T1FS) and 3D gradient echo images (GRE) was compared using the chi-square test. A p value<0.05 was accepted as significant. All other statistical analyses were performed with SPSS software (version 18.0; SPSS Inc., Chicago, IL, USA).
The MFibL was optimally visualized on the far lateral sagittal 3D GRE and T1FS MRA images. The MFibL appeared as a curvilinear or straight hypointense band of variable thickness extending between the lateral meniscus and the fibular head. From the total of 19 knee MRAs at 70° knee flexion, the MFibL was depicted on the far lateral T1FS image and 3D GRE images as a thin linear (n=16/19)(Fig. 1) or thick (n=3/19) (Fig. 2) hypointense structure anterior to the popliteus tendon.
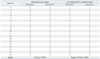
The interobserver agreements were significantly good. On 3D GRE images, reviewer 1 identified the MFibL in 94.7% (n=18/19) by scale 2 and 5.3% (n=1/19) by scale 1, whereas reviewer 2 identified the MFibL in 89.5% (n=17/19) by scale 2 and 10.5% (n=2/19) by scale 1 (kappa=0.642, p=0.003). On sagittal T1FS images, both reviewers identified the MFibL in 78.9% (n=15/19) by scale 2 (kappa=0.683, p=0.003) (Table 1). No image was shown by scale 0 on both 3D GRE and T1FS images, i.e. all the cases of this MR study showed the MFibL at least partially.
Both reviewers found scale 2 MFibL in 89.47% (n= 17/19) of the knee T1FS images and 73.68% (n=14/19) of the knee 3D GRE images. There was no statistically significant difference in visualization of the MFibL between T1FS and 3D GRE sequence (p>0.05).
The MFibL was depicted on MRA as a thin linear (Fig. 1) or thick (Fig. 2) hypointense structure anterior to the popliteus postero tendon. The MFibL can be thickened due to larger rotation of the fibula, resulting from repetitive lateral meniscus tear.2,7,8 The MFibL is a ligament of variable thickness extending between the inferior margin of the lateral meniscus and the fibular head. Previous cadaveric studies have shown that the mean thickness of the MFibL with its capsular layer was 3.84 mm with a range of 2.6-6.1 mm.7 In this study, the thickening of MFibL was noted in three knee joints: one with medial meniscal tear, one with anterior cruciate ligament tear, and another with a ruptured popliteal cyst. Possible relation with knee abnormalities is expected to be clarified in the future.
The posterosuperior popliteomeniscal fascicle extends in a posterior direction from the posterosuperior corner of the posterior horn of the lateral meniscus to the posterior joint capsule.9 The posteroinferior popliteomeniscal fascicle, although the presence is controversial, is a broad aponeurotic extension from the popliteus muscle to the inferior margin of the lateral meniscus.10,11 These fascicles could be differentiated from the linear structures between the lateral aspect of the mid to posterior body of the lateral meniscus and the styloid process of the fibula that matched the description of a meniscofibular ligament. The MFibL can be distinguished from the posterosuperior and posteroinferior popliteomeniscal fascicles (Fig. 3).
The MRA with knee flexion was performed in a way similar to the arthroscopic posture which consists of a fluid capsular distention, knee flexion, and mild external rotation. Since the conventional MR of the knee is performed in a neutral position (about 10° knee flexion), a discrepancy may exist between MR findings and arthroscopic findings. Thus, the knee flexed MRA would be helpful for the pre-arthroscopic MR evaluation. In this study, T1FS sequence images showed high signal-to-noise ratio (SNR), and the visualization capacity of MFibL was comparable to that of 3D GRE sequences (Fig. 4). However, the 3D GRE images could be beneficial as partial volume effects could be eliminated with a minimal slice thickness of 0.5 mm.
Some limitations exist in this study. There was no cadaveric correlation with the MRA findings. The SNR of the MRA was relatively low because there was no available dedicated coil for a posture of knee flexion. Most existing knee coils are in a cylindrical shape which limits the knee from flexion. Advanced dedicated coil for knee flexion and imaging sequences would resolve this problem in the future.
Overall, the MFibL was identified in all patients on the far lateral sagittal GRE images and T1FS images of MRA with knee flexion posture. This posture is identical to the posture for the conventional arthroscopy, which could potentially be useful in recognizing structures in the posterolateral corner of the knee, including the MFibL.
Figures and Tables
Fig. 1
MR arthrographic appearance of the meniscofibular ligament (MFibL). (A and B) A sagittal fat suppressed T1 weighted image of MR arthrography (A) and a corresponding sagittal 3D gradient echo MR arthrography (B) demonstrate the MFibL as a linear hypointense structure (white arrows) extending between the apex of the fibular head and the posterior third of the lateral meniscus. The popliteus tendon is located posterior to MFibL (black arrow). (C) Virtual MR arthroscopy reveals the relationship between the popliteus tendon and the MFibL (white arrows). LC, lateral condyle of femur; T, tibia; F, fibula; LM, lateral meniscus; MR, magnetic resonance; 3D, three-dimensional.

Fig. 2
MR arthrographic appearance of meniscofibular ligament (MFibL). Continuous sagittal fat suppressed T1 weighted images of knee MR arthrography demonstrate the MFibL as a linear, hypointense structure (white arrows), extending between the apex of the fibular head and the posterior third of the lateral meniscus. The popliteus tendon is located posterior to MFibL (black arrow). LC, lateral condyle of femur, T, tibia; F, fibula; FCL, fibular collateral ligament; BF, biceps femoris tendon; MR, magnetic resonance.

Fig. 3
Posterosuperior and posteroinferior popliteomeniscal fascicules. A sagittal fat suppressed T1 weighted image of MR arthrography (A) and a corresponding sagittal 3D gradient echo MR arthrography (B) demonstrate the posteosuperior (black arrow) and posteroinferior (white arrow) popliteomeniscal fascicles. LC, lateral condyle of femur; T, tibia; MR, magnetic resonance; 3D, three-dimensional.

Fig. 4
The difference between fat suppressed T1 weighted image and 3D gradient echo image. A sagittal fat suppressed T1 weighted image of MR arthrography (A) demonstrates the MFibL as a linear hypointense structure (white arrows). The popliteus tendon is located posterior to the MFibL (black arrow). However, the MFibL can partially be delineated on the corresponding sagittal 3D gradient echo MR arthrography (B). LC, lateral condyle of femur; T, tibia; F, fibula; MFibL, meniscofibular ligament; MR, magnetic resonance; 3D, three-dimensional.

ACKNOWLEDGEMENTS
This study was supported by a faculty research grant of Yonsei University College of Medicine (6-2009-0163).
References
1. Covey DC. Injuries of the posterolateral corner of the knee. J Bone Joint Surg Am. 2001. 83-A:106–118.

2. Bozkurt M, Elhan A, Tekdemir I, Tönük E. An anatomical study of the meniscofibular ligament. Knee Surg Sports Traumatol Arthrosc. 2004. 12:429–433.

3. Standring S. Gray's anatomy: The Anatomical Basis of Clinical Practice. 2005. 39th ed. Elsevier Churchill-Livingstone;1477.
4. Obaid H, Gartner L, Haydar AA, Briggs TW, Saifuddin A. The meniscofibular ligament: an MRI study. Eur J Radiol. 2010. 73:159–161.

5. Munshi M, Pretterklieber ML, Kwak S, Antonio GE, Trudell DJ, Resnick D. MR imaging, MR arthrography, and specimen correlation of the posterolateral corner of the knee: an anatomic study. AJR Am J Roentgenol. 2003. 180:1095–1101.

6. Krudwig WK, Witzel U, Ullrich K. Posterolateral aspect and stability of the knee joint. II. Posterolateral instability and effect of isolated and combined posterolateral reconstruction on knee stability: a biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2002. 10:91–95.

7. Ogden JA. The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res. 1974. 186–191.
8. Bozkurt M, Yilmaz E, Atlihan D, Tekdemir I, Havitçioğlu H, Günal I. The proximal tibiofibular joint: an anatomic study. Clin Orthop Relat Res. 2003. 136–140.
9. Peduto AJ, Nguyen A, Trudell DJ, Resnick DL. Popliteomeniscal fascicles: anatomic considerations using MR arthrography in cadavers. AJR Am J Roentgenol. 2008. 190:442–448.

10. Terry GC, LaPrade RF. The posterolateral aspect of the knee. Anatomy and surgical approach. Am J Sports Med. 1996. 24:732–739.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download